Adult Sheep Lameness Flashcards
what are contagious causes of lameness in sheep
Interdigital dermatitis (scald)
Footrot
Contagious ovine digital dermatitis (CODD)
Strawberry footrot
Maedi Visna
Septic arthritis (joint ill)
Foot and mouth disease
what are non contagious causes of lameness
Shelly hoof
White line disease
Abscess
Interdigital fibroma
Trauma
- Joints, bones, muscle, nerves
Septic arthritis
White muscle disease
what causes scald/footrot
Mild: Fusobacterium necrophorum
Severe: Dichelobacter nodosus
what is interdigital dermatitis (scald)
Inflammation of skin between digits
what are the clinical signs of interdigital dermatitis
Very painful
Moist
Hairless
White or pink
Ulcerated
what are predisposing factors to interdigital dermatitis
Damage to interdigital skin
Continual wet conditions
Thistles, coarse/long grass
how is interdigital dermatitis treated in lambs
Individuals: antibiotic spray
Group outbreaks: foot-bath fortnightly, clean field
how is interdigital dermtatits treated in adults
Antibiotic injection and spray
Outbreaks: foot-bath and move to clean pasture
what causes footrot
Dichelobacter nodosus +/- Fusobacterium necrophorum
where does footrot start in the foot
in the interdigital space and then under runs wall and sole horn
what are the clinical signs of footrot
Black, crumbling, moist debris
Pungent, distinctive smell
where does dichelobacter nodosus survive
In damp conditions
In the environment for 10-14 days (?)
In hoof trimmings for 6 weeks
In feet of chronic carriers
what are predisposing factors to footrot
Wet conditions
Warm
High stocking density
Genetic predisposition
how is footrot treated
Antibiotic injection (lasting minimum of 3 days)
Antibiotic spray
Isolate
Delayed treatment = delayed recovery
Foot trimming = delayed recover
Detrimental
how is footrot prevented
Cull
Vaccinate
Quarantine
Avoid
Treat
how do you reduce the challenge for footrot
Quarantine
Avoid spread at gatherings
avoid spread at high traffic areas
early treatment
how should sheep be quarantined to reduce footrot challenge
- Reduce imported strains (and CODD)
- Minimum 30 days
- Examine feet (start and end)
- Reject or treat
- Active lesions
- Chronically thickened digits
- Footbath (start and end)
- Vaccinate?
how is footrot spread avoided at gatherings
Avoid unnecessary gatherings
Reduce time gathered
Hard, well drained surface without loose stones
Clean and disinfect between groups
Mobile facilities move between groups/gathers
Lime on standing surface
Footbath after gathering
how is footrot spread reduced at high traffic areas
Water troughs, feed faces, gateways
Well drained surroundings
Move feeding spots frequently
Spread lime in gateways
Isolate lame sheep, especially at housing
how is early treatment for footrot used to reduce the challenge
- Correct treatment for lesion!
- Ideally within 3 days
- Reduces pasture contamination
- Increased probability of recovery
- If not recovered with 14 days re-assess the diagnosis
how can you increase resilience to footrot in a herd
culling
vaccination
how should you cull for footrot
Mark and record lame sheep
Cull if 2 bouts within 12 months
Cull if chronically lame
- Reduce contamination from chronic shedders
- Build immune flock — especially rams!
how are sheep vaccinated against footrot
Covers 10 common strains
Irritant
- Care with location
- Care with timing
Whole flock, including rams
Treatment or prevention
Moxidectin 1% injection (cydectin or zermex)
what agent causes contagious ovine digital dermatitis
Treponemes thought to be involved
Similar to DD in cattle
what does contagious ovine digital dermatitis result in
deformed digit
club digit
very painful
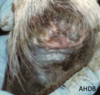
what are the clinical signs of contagious ovine digital dermatitis
Starts at coronary band — often red and inflamed
Lose horn capsule
Capsule re-grows
how is contagious ovine digital dermatitis treated
Amoxicillin, long acting and may need repeating
Macrolides — second line
Anti-inflammatories
Oxytetracycline may be less effective
how is contagious ovine digital dermatitis prevented
Quarantine — avoid buying in
Isolate cases
Footbath after gathering
Note: antibiotic footbaths are not responsible use!
Footrot vaccination can reduce