7 ⼀ENDOCRINE/OPHTHO Flashcards
46
how are pregnant patients screened for hyperthyroidism? (3)
torn
TSH
(low TSH) ➜ [free T4]
(normal [free T4]) ➜ [Total T3]
use trimester-specific norms
management? (2)

eye shield
+
[hospital admit (strict bed rest + 30° bed + serial intraocular pressures+ [prevent rebleeding and intraocular HTN → vision loss])]
HYPHEMA
Stress Hyperglycemia occurs when ⬜. This presents very similarly to ⬜
_________________
how do you differentiate the two? (2)
Stress Hyperglycemia is a/w ⇪ morbiditiy
[STRESS (severe illness > 39C)] ➜ [CortisolGlucocorticoid] secretion➜ ⇪ Insulin resistance ➜ hyperglycemia ;
DKA
_________________
DKA has [hgbA1C ≥6.5%] +[“FUDGe” DM classic s/s]
patient newly diagnosed with Papillary Thyroid Cancer
What’s 1st step after this?
_________________
What are the treatments? (2)
[Neck & Cervical lymph node US for initial staging]
_________________
- [< 1 cm = lobectomy]
- [TOTAL THYROIDECTOMY if: ≥1cm | extension outside thyroid | distant metz | hx head/neck radiation exposure]
Which antiDM are a/w weight gain? (3)
Insulin
[Thiazolidinediones (pioglitazone)]
Sulfonylurea
“Insulin Tops Scales”
What is Euthyroid Sick Syndrome? (4)
_________________
mgmt? (3)
⭐acute illness ➜ [⬇︎ peripheral conversion of T4➜ T3] → forces peripheral T4 to be converted to ®T3 instead
⭐but causes no other change to the thyroid →[nml TSH, nml T4 ]
with
⭐[low T3io\normal TSH and normal T4]
and
⭐[HIGH ®T3io\normal TSH and normal T4]
[ ✔︎TSH, ✔︎T4, , ⬇︎T3, ⇪®T3 ] = Euthyroid Sick Syndrome
should resolve once acute illness is resolved
_________________
Repeat Thyroid Function Test after acute illness is resolved –(if persist)–> give [Liothyronine T3] supplement
What is [reverse ®T3]?
_________________
what is it used for?
rT3 = [inactive metabolite of unconverted T4]
_________________
[rT3] Differentiates …
Euthyroid Sick Syndrome (illness ⬇︎ peripheral conversion of T4 ➜ T3 = [⬇︎T3] but [⇪ rT3 (from INC unconverted T4)])
_________from________
central hypOthyroidism (low TSH ➜ ⬇︎T4 ➜ [⬇︎T3] AND [⬇︎rT3])
How do you workup a patient with suspected [central hypOpituitarism] (5)

patients with [classic Congenital Adrenal Hyperplasia] require prompt therapy with ⬜ and chronic tx with ⬜
Why ? (3)
[high dose hydrocortisone] ; glucocorticoid and mineralocorticoid replacement
_________________
avoid adrenal crisis by maintaining BP / growth/ suppress adrenal androgens
classic CAH = 21hydroxylase deficiency CAH

Recite the Adrenal Gland blueprint for
Zona Glomerulosa (13)
*

Recite the Adrenal Gland blueprint for
Zona Fasciculata -7

Recite the Adrenal Gland blueprint for
Zona Reticularis-6

The most common enzyme deficiency for [Congenital Adrenal Hyperplasia] is
⬜
________________
cp?-3
21 hydroxylase
[(complete=CLASSIC CAH (C)] | [(reduced=NONClassic CAH (NC)]
🅶
▶C[⬇︎AldosteroneMineralocorticoid] → [Salt Wasting( losing Na+ / gaining K+)] → hypOtension + vomiting
🅵
▶C[⬇︎CortisolGlucocorticoid]
🆁
▶NC & C[⇪Testosterone] ← [⇪ 17HydroxyProgesterone]
= Virilization = [Ambiguous genitalia in females] + (acne, premature adrenarche/pubarche)

MC=MineraloCorticoid/GC=GlucoCorticoid
The 2nd most common enzyme deficiency for [Congenital Adrenal Hyperplasia] is
⬜
________________
cp?-5
11βhydroxylase
🅶
▶ [⇪ 11DOCSMC] = weak Mineralocorticoid → Salt Retention → Fluid Retention = HTN
▶[⬇︎AldosteroneMineralocorticoid]
🅵
▶[⇪11dcGC]
▶[⬇︎CortisolGlucocorticoid]
🆁
▶[⇪ ⇪Testosterone] ← [⇪⇪ 17HydroxyProgesterone] ← {[⇪11DOCSMC]🅶 & [⇪11dcGC]🅵}
= Virilization = [Ambiguous genitalia in females] + (acne, premature adrenarche/pubarche)
[11dc =11deoxycortisol] | [11DOCS =11DeOxyCorticoSterone] | MC=MineraloCorticoid/GC=GlucoCorticoid

The least common enzyme deficiency for [Congenital Adrenal Hyperplasia] is
⬜
________________
cp?-2
17 αhydroxylase
🅶
▶[⇪ ⇪ AldosteroneMineralocorticoid] ← [⇪⇪ 11DOCSMC]
= Salt Retention → Fluid Retention = HTN
🅵
▶[⬇︎CortisolGlucocorticoid]
🆁
▶[⬇︎Testosterone]
= ALL PATIENTS PHENOTYPICALLY FEMALE
[11dc =11deoxycortisol] | [11DOCS =11DeOxyCorticoSterone] | MC=MineraloCorticoid/GC=GlucoCorticoid

The most common enzyme deficiency for Congenital Adrenal Hyperplasia is ⬜
Which lab value is diagnostic for this deficiency?
21 hydroxylase (complete = classic CAH | reduced=nonClassic CAH)
⬆︎17 HydroxyPROGESTERONE

What benefits does maintaining Tight Glucose Control in DM pts give?
⬇︎ microvascular complications (retinopathy/nephropathy)
What are all the functions of [CortisolGlucocorticoid] - 6
⇪BIG ⬇︎FIB
- ⇪ Blood pressure (⬆︎a1 receptors)
- ⇪Insulin resistance –> DM
- ⇪Gluconeogenesis
_________________ - ⬇︎Fibroblast –> striae
- ⬇︎Immune system (WHITE)
- ⬇︎Bone formation by ⬇︎osteoBlast
what is Apathetic Thyrotoxicosis ? (4)
- [atypical elderly HYPERthyroidism] =
- [APATHY (lack of enthusiasm/interest), mimics DEPRESSION, lethargy, confusion, wt loss]
- (misdiagnosed as depression or dementia),
- likely NO thyromegaly
S/S of hypOthyroidism is mostly opposite of Hyperthyroidism sx
What are 9 symptoms specific to only hypOthyroidism?
Mostly opposite of TT Feels ARCHED but specifically causes {med}3…
menorrhagia
macroglossia
myalgia/arthralgia
[edema ([Myxedema nonpitting] / pedal)]
[eval labs (HLD, Macrocytosis & hypOnatremia in elderly)]
[eerie (HOARSE) voice]
diastolic HF
depression
dry coarse skin
BOTH HAVE FATIGUE AND HTN
Clinical definition of Diabetic Ketoacidosis (DKA) -2
[metabolic acidosis (HCO3<15 or pH<7.3)]
in the setting of [hyperglycemia > 200]
how do you manage HHONKS-6?
[HHONKS (Hyperglycemia HyperOsmolar NON Ketone State)]
FIPAAR control
-
Fluid control : (NS) < [Blood Sodium 135] < (1/2 NS)
_________________ -
Insulin control:
🍭[Continuous infusion until BG 200]]
🍭➜ [when BG ≤ 200 ⬇︎ infusion and add dextrose5%]
🍭➜ [on G.A.P.E.Resolution = start (subQ mealtime + basal insulin)] ➜ DC insulin infusion 2h later]
_________________ -
Potassium control: [✳]
_________________ -
Acid control: give HCO3 for [pH< 6.9 or HCO3< 15]
_________________ -
ANION GAP CONTROL: [correct to 10-14]
_________________ -
G.A.P.E.RESOLUTION = {[Glucose< 200] + [Anion Gap 10-14] + [pH>6.9 and HCO3 ≥15] + [Eating tolerated → ICU admitted]}
_________________
(monitor phosphate and Ca+ also)
[✳] : {serum K+: [(hold insulin) < –3.3–(give IV K+)– 5.2–> ✔︎]}
how do you manage DKA-6?
DKA:Diabetic Ketoacidosis
FIPAAR control
-
Fluid control : (NS) < [Blood Sodium 135] < (1/2 NS)
_________________ -
Insulin control:
🍭[Continuous infusion until BG 200]]
🍭➜ [when BG ≤ 200 ⬇︎ infusion and add dextrose5%]
🍭➜ [on G.A.P.E.Resolution = start (subQ mealtime + basal insulin)] ➜ DC insulin infusion 2h later]
_________________ -
Potassium control: [✳]
_________________ -
Acid control: give HCO3 for [pH< 6.9 or HCO3< 15]
_________________ -
ANION GAP CONTROL: [correct to 10-14]
_________________ -
G.A.P.E.RESOLUTION = {[Glucose< 200] + [Anion Gap 10-14] + [pH>6.9 and HCO3 ≥15] + [Eating tolerated → ICU admitted]}
_________________
(monitor phosphate and Ca+ also)
[✳] : {serum K+: [(hold insulin) < –3.3–(give IV K+)– 5.2–> ✔︎]}
[HHONKS (Hyperglycemia HyperOsmolar NON Ketonic State)**] is a complication of DM
What Blood Glucose precipitates this?
Blood Glucose > 600
How does DKA and HHONKS affect total body K+ levels?
⬇︎total body K+ (REGARDLESS OF WHAT SERUM VALUE SAYS)
DKA & HHONK causes severe osmotic diuresis –> ⬇︎total body K+ stores even though serum K+ level may be elevated = [maintain > 5.3K+ ✳]
In DKA and HHONKS management, when do you hold the insulin?
serumK <3.3
Remember that ALL DKA and HHONKS pts are Total Body K+ depleted due to osmotic diuresis regardless of what serum values say

In DKA and HHONKS management, when do you consider using Sodium Bicarbonate?
pH<6.9

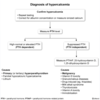
You suspect a pt has Cushing Syndrome
How do you work this up?-3
1st: .Determine if pt has ⇪ [CortisolGC]([Overnight low-dose dexamethasone suppression test] | [late night salivary cortisol assay] | [24 hr urine free cortisol])
2nd. If [CortisolGC] ⇪ = ⊕Cushing Syndrome
3rd: If ⊕Cushing Syndrome → perform ACTH workup(image) to determine if Cushing Syndrome [ACTH-dependent] or [ACTH-INdependent]

You suspect a pt has Cushing Syndrome
After completing step 1 and step 2 of Cushing Syndrome workup, your attending ask you to perform the [3rd step ⼀ACTH workup] to determine _______
What is the ACTH workup? -3
3rd: If ⊕Cushing Syndrome → perform ACTH workup(image) to determine if Cushing Syndrome [ACTH-dependent] or [ACTH-INdependent]

Name the characteristics of Cushing Syndrome - 7
“Fat Heavy People May HOG the Cushing”
- Fat reDistribution (central obesity, Moon face)
- Hyperpigmentation (from excess ACTH activating [Melanocyte MC1 R])
- Purple striae with skin atrophy and bruisability
- Muscle atrophy
- HTN
- Osteoporosis
- Glucose intolerance
________________
Cushing SYNDROME is caused by ⇪ [CortisolGlucocorticoid](which may be ACTH-INdependent or ACTH-dependent)
autoimmune adrenalitis is known as _____ disease
etx?
[Addison’s Primary Adrenal Insufficiency] disease
Autoimmune Primary Adrenal Insufficiency (suspect this in pts with other Autoimmune diseases - pernicious anemia, vitiligo, hypothyroid!)
Sx = HYPERKalelmia, hypOnatremia, wt loss, fatigue
What are the main causes of [Addison’s Primary Adrenal Insufficiency]? - 4
- TB
- Autoimmune adrenalitis
- CA
- Adrenal Hemorrhage
Main sx for [Addison’s Primary Adrenal Insufficiency] - 8
“Addison was a SNAP FHAG”
- [Sodium ⬇︎ DEC]
- [NAHA (Normal AG Hyperchloremic metabolic acidosis)]
- AnorexiaWT LOSS
- [Potassium ⇪ INC]
- Fatigue
- [Hyperpigmentation(ACTH and MSH)]
- [Androgen deficiency(⬇︎axillary/pubic hair)]
- GI Sx

What is Cosyntropin?
_________________
Describe how it used to workup ⬜
ACTH analog ⼀used for ACTH stimulation test – when [basal morning plasma cortisol] and [basal morning plasma ACTH] are equivocal
_________________
[Addison’s Primary Adrenal Insufficiency]

What test should you order to diagnose [Addison’s Primary Adrenal Insufficiency]? (3)
- basal morning plasma cortisol ⼀(dx = low cortisol)
- basal morning plasma ACTH ⼀(dx = HIGH ACTH)
- [Cosyntropin ACTH stimulation test] ⼀(use if 1 and 2 are equivocal)

Which 5 drugs cause Drug-Induced Lupus?
_________________
How is Drug-Induced Lupus diagnosed? (2)
HEMPI to DIL
Hydralazine
[Etanercept (TNFα R Blocker)]
Minocycline
Procainamide
[Infliximab (TNFα R Blocker)]
_________________
+ANA and +antiHistone

Why are frequent ophthalmologic exams necessary for prolonged CTS users?
CTS changes lens epithelial gene transcription ➜ CATARACTS
In addition to ⇪ glucose urinary excretion , how do SGLT2 inhibitors delay the progression of DM nephropathy?
inhibiting Na+/Glucose transporter ➜ [⇪ urinary glucose] AND [⇪ urinary Na+] and the [⇪ urinary Na+] travels to macula densa where it causes ⬇︎renin secretion ➜ [⬇︎Angiotensin II] ➜ ⬇︎efferent arteriole constriction ➜ ⬇︎GFR = delays DM nephropathy

pt p/w eye pain with foreign body sensation
what’s your workup? (4)

Both preseptal cellulitis and orbital cellulitis present with (⬜3)
_________________
How are they differentiated? (3)
[eyelid swelling-redness] / fever / conjunctivitis
_________________
orbital = orbit eye pain with movement + proptosis + ophthalmoplegia

How do you treat Orbital cellulitis? (2)
IVAbx ➜ [Surgical debridement (if fluid collection/abscess present)]

How do you workup Hyperthyroidism? -5

Exogenous thyrotoxicosis MOD
[OTC Thyroid supplement vs surreptitious prescription thyroid med] ➜ supressess [ANT Pit TSH] ➜ ⬇︎thyroid gland synthesis ( ⬇︎RAIU and ⬇︎thyroglobulin)

Common s/s of HYPERthyroidism -9
TT Feels ARCHED
- Tremor
- Tachycardia
- [Fatigue(+/- Apathy in Elderly)]
- Appetite ⬆︎ but Wt ⬇︎
- Reflexes ⬆︎
- Cardio* (Tachycardia, Palpitations,Exertional SOB, ⇪Myocontractility→HTN)*
- Heat intolerance –> SWEATING
- [Exophthalmos with lid lag = GRAVES DISEASE]
- Diarrhea +/- dyspepsia
Older pts may only have Fatigue, Cardio, or Apathetic!

For patients taking CTS, which patients need their dose regimens tapered down at the end?
[CTS > 3 Weeks] = TAPER DOWN
(taper allows for return of adequate endogenous cortisolglucocorticoid)

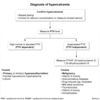
How do you workup Hypercalcemia? -4
MEASURE PTH!

Hypercalcemia can either be PTH-dependent or PTH-INdependent
What are the causes of [PTH-dependentHypercalcemia]? (4)
- Primary HyperParathyroidism
- Tertiary HyperParathyroidism(Intractable Hypercalcemia 2/2 Autonomous Parathyroid)
- [Familial hypOcalciuric Hypercalcemia]
- Lithium

Hypercalcemia can either be PTH-dependent or PTH-INdependent
What are the causes of [PTH-INdependentHypercalcemia]? (8)
- MALIGNANCY
- [VitD toxicity]
- [VitA toxicity]
- Granulomatous disease
- [LCD-TV Rx]
- Milk-alkali syndrome
- Thyrotoxicosis(Thyroid hormone causes bone resorption → ⇪ Ca+)
- Immobilization
normal range for
PTH
10-60
After working up Hypercalcemia, you determine cause is Malignancy
List the 3 Causes of [Hypercalcemia of Malignancy] , which Cancers cause them and their MOD

Which Rx cause Hypercalcemia (5)
NormalCa+ = 8.4-10.2
“LCD-TV with too much Calcium!”
Lithium
Ca+carbonate excess
DVitamin
Thiazides
VitaminA
nml TSH: [0.4-4.0]
which thyroid condition is a/w Thyroid Lymphoma?
hCAT
[hashimoto Chronic Autoimmune(antiTPO) Thyroiditis]
_________________
hCAT can progresses to Thyroid Lymphoma | [hCAT+ Pemberton = Thyroid Lymphoma]
chronic [antiTPO Lymphocyte] infiltrate thyroid targeting TPO

What is Pemberton’s sign?
_________________
What does it indicate? -2
facial plethora or neck vein distension when arms are raised
_________________
- obstructive ENLARGED THYROID
- [Thyroid lymphoma (if ⊕ in the setting hCAT)]
Medullary thyroid cancer
cp -2
- [thyroid nodule iTSo MEN]
- [Calcitonin ⇪ (from thyroid gland C cell neoplasia)]
* MEN = Multiple Endocrine Neoplasia // iTSo = in The Setting of*

Describe MEN1 (3)
PituitaryMacroAdenoma
Parathyroid hyperplasia
[Pancreatic-GI GLIV tumors ⼀Gastrinoma/gLucagonoma/Insulinoma/VIPoma]

Describe MEN2A (3)
- Parathyroid Hyperplasia
- Medullary Thyroid CA
- Pheochromocytoma

Pt with new diagnosis MEN2B
Prior to thyroidectomy, patient must be 1st evaluated for coexisting tumors such as ⬜ and Pheochromocytoma.
Name the dx labs for Pheochromocytoma (4)
_________________
Why is this important?
Parathyroid hyperplasia
_________________
1st: {[Plasma free metanephrines] –(confirm by)– >
2nd:
- [24h urinary fractionated metanephrines]
- catecholamines
- abd imaging]}
_________________
Undiagnosed Pheochromocytoma can cause fatal HDUS peri-thyroidectomy

MEN2A and MEN2B share the same initial workup
List the diagnostic workup for {new dx[MEN2A ] or new dx[MEN2B]} - (5)
- Calcitonin
- CEA
- [Neck US (r/o regional metastasis)]
- [Chromo10RET protooncogene] germline testing
- [Coexisting tumor r/o ([Parathyroid hyperplasia], [Medullary Thyroid Hyperplasia], Pheochromocytoma,)]

Describe MEN2B (4)

Pt p/w the 3 P’s of MEN1 ( _______ )
What’s the next step in Management of MEN1?
PituitaryMacroadenoma/Parathyroid hyperplasia/[Pancreatic-GI GLIV tumors]
_________________
[PARATHYROIDECTOMY with autotransplantation to muscle pocket]

Pt p/w the 3 P’s ( ⬜ ) of MEN1
Measurement of Gastrin is often used to diagnose ⬜, but Gastrin can only be measured in the setting of ⬜ serum Ca+ and No ⬜.
Why is this?
[Prolactinoma]/[Parathyroid hyperplasia]/[Pancreatic&GI GLIV tumors]
_________________
[Pancreatic Gastrinoma (Zollinger Ellison)]
- normal Ca+ (⇪ Ca+ ➜ falsely elevated gastrin)
- NO acid-reducing tx (PPI ➜ falsely elevated gastrin)

How are the thyroid and Calcium related?
[T3/T4thyroid hormone] causes bone resorption ➜ ⇪ serum Ca+/Hypercalcemia
Candida Endophthalmitis
clinical features (4) \_\_\_\_\_\_\_\_\_\_\_\_\_\_\_\_\_
Treatment? (3)
- [fundoscopic fluffy yellow-white chorioretinal lesions]
- [floaters + eye pain and ⬇︎acuity]
- [hospitalized patients on Parenteral nutrition = RF1]
- [s/p GI surgery or GI perforation = RF2]
_________________
Tx = [Vorizonazole + Intravitreal antifungal + vitrectomy]
_________________
RF = Risk Factor
What causes [Pancreatogenic DM]?
_________________
Which antiDM should be used to treat this? Which 3 should not? why?
Chronic pancreatitis (RF cystic fibrosis) ➜ islet cell damage ➜ ⬇︎insulin secretion then insulin deficiency ➜ glucose intolerance ➜ DM
_________________
✔︎ = INSULIN-replace Insulin pt stopped producing
❌❌= [GI peptide antiDM (DPP4 inhibitors / GLP1🟢)] - since these target GI peptides ➜ slows gastric emptying and ⇪ risk for pancreatitis
or
❌= [insulin secretagogues (Glipizide)]- impaired ability to secrete endogenous insulin from DEC islet beta cell reserve

Glipizide
MOA
insulin secretagogues
GLP1 R agonist
MOA
Name 3 examples
_________________
Glucagon-Like Peptide-1 R agonist
Food → intestine [GLP1] secretion naturally ➜ GLP1iLAGG → GLP1 is then cleaved-inactivated by DPP4
_________________
⇪ insulin secretion and insulin sensitivity
⬇︎Liver glucose secretion
⬇︎Appetite → wt loss
⬇︎Gastric emptying(⇪pancreatitis risk)
⬇︎Glucagon secretion
_________________
so… [GLP1🟢] → ⇪GLP1iLAGG
________________
liragluTIDE / exenaTIDE / dulagluTIDE

DPP4 inhibitors
MOA
Give 2 examples
Targets GI peptides ➜ slows gastric emptying
________________

linaGLIPtin
sitaGLIPtin
saxaGLIPtin
Why are [Pioglitazone thiazolidinedione] contraindicated in CHF?
[Pioglitazone thiazolidinedione] ⇪ insulin sensitivity by stimulating [PPAR-γ] on liver/muscle/fat]
BUT
it also stimulates [PPAR-γ] on renal CD ➜ ⇪ Na+ reabsorption ➜ fluid retention ➜ precipitates CHF
What is Amaurosis fugax?
sudden reversible transient monocular blindness 2/2 carotid artery atherosclerotic disease
Amaurosis fugax
tx?
carotid endarterectomy
Amaurosis fugax
dx?
carotid doppler US
What is subclinical thyrotoxicosis?
_________________
how is it managed?
mildly low TSH but [normal free T4, normal T3 and normal physiology (normal HR, bone density)]
_________________
RECHECK Thyroid function test in 8WKS (most TSH normalize on its own)
a Patient with chronic hypOparathyroidism presents with low serum Ca+ but HIGH urinary Ca+ from their Ca+ supplement
How do you mitigate this?
HCTZ
_________________
HCTZ [⇪ serum Ca+] while [⬇︎ urinary Ca+]
How is the thyroid system associated with Surgery?
[hypOthyroidism] ➜ [poor periOperative outcomes]
⼀BUT 911 surgeries are Ok if hypOthyroidism not severe (i.e. no myxedema coma)
Why must Levothyroxine at first be titrated very slowly in CAD pts ?
[levothyroxine T4] ⇪ myocardial O2 demand which can ➜ Myocardial ischemia ➜ in CAD pts can cause MI or arrhythmia = slow gradual [levothyroxine T4] titration
NPH is a ⬜ insulin that is sometimes used as ⬜. Why should it NOT be used in patients who’ve had hypOglycemic episodes?
intermediate-acting ; [basal insulin when injected BID]
_________________
NPH has a pronounced peak which can ➜ hypOglycemia = bad for patients who already have hypOglycemic episodes

When is it indicated to switch a T1DM pt from [manual SQ Basal/bolus insulin injection] to [automated SQ continuous infusion insulin pump]?
Pump Indicated if T1DM pt (on current manual injection) has…
- hypOglycemic episodes
- [suboptimal glycemic control HbA1C>7]
- highly variable BG readings
Patient presenting with new diagnosis T1DM. Tx requires exogenous insulin.
Describe the [manual SQ Basal/bolus insulin injection] regimen the patient will start with
T1DM require a
[(long basal) and (rapid bolusx3)] every day

Work up for Thyroid Nodule?
[Cancer RF = (> 1cm), fam hx, radiation hx, cervical LAD, compressive sx, thyroid hormone ∆]
[Suspicious US = hypOechoic, microcalcifications, internal vascularity]

After RF and US eval – Any Thyroid Nodule > ⬜ cm needs work up with FNA
List all the [High Risk Thyroid features] that warrant FNA for Thyroid Nodule (9)
> > 1 cm_________________
[Cancer RF = (> 1cm), fam hx, radiation hx, cervical LAD, compressive sx, thyroid hormone ∆]
[Suspicious US = hypOechoic, microcalcifications, internal vascularity]

Why are hypoglycemic episodes in long standing DM1 pts even more serious than newly diagnosed DM1 pts?
_________________
how is this mitigated?
✔︎ long standing DM1 pts overtime develop blunting of their autonomic feedback to [hypOglycemia (tremor, sweating, AMS)] = ⬇︎[hypOglycemia awareness system (HAS)]
✔︎ so this means… if long-standing DM1 present with hypOglycemia ⼀ it’s likely to be a SEVERE HYPOGLYCEMIA EPISODE (since , in a {blunted HAS} pt, only SEVERE HYPOGLYCEMIA can activate a {blunted HAS} to induce sx necessary to make pt aware/get help]
_________________
[Strict avoidance of any hypOglycemia x 2-3 weeks] restores patient’s HAS

nml TSH: [0.4-4.0]
Name the 2 [DeTC (Differentiated epithelial Thyroid CA)] subtypes
- [papillary thyroid cancer]
- [follicular thyroid cancer]
DeTC target TSH : [LR =TSH(0.1-0.5)6mo→ (Ln)] | [IR=TSH(0.1-0.5)] | [HR=TSH(<0.1)x yrs]
nml TSH: [0.4-4.0]
Why is it important to [prevent elevated TSH] in pts with DeTC?
Considering this, how do you determine the ideal TSH level DeTC patients should be kept? (3)
_________________
(DeTC=Differentiated epithelial Thyroid Cancer)
in [DeTC s/p thyroidectomy] pts, elevated TSH actually stimulates growth of residual thyroid cancer cells = goal TSH depends on Risk of Recurrence
[LR =TSH (0.1-0.5)6-12mothen → (low nml TSH range)]
[IR=TSH (0.1-0.5)]
[HR=TSH (<0.1)]x years
TSH*=DeTC TSH goal

nml TSH: [0.4-4.0]
management for [DeTC (papillary vs follicular)] varies and is dependent on ⬜ and importantly ⬜
_________________
(DeTC=Differentiated epithelial Thyroid Cancer)
[initial stage of CA] ; [Risk of Recurrence]
_________________
DeTC target TSH : [LR =TSH(0.1-0.5)6mo→ (Ln)] | [IR=TSH(0.1-0.5)] | [HR=TSH(<0.1)x yrs]

Name the 3 benefits to [STRICT blood glucose control] in DM pts
DECREASES…
- [microvascular complications ⼀nephropathy, retinopathy]
- [peripheral neuropathy onset]
- [peripheral neuropathy progression]
Gastroparesis = ⬜ and is ultimately diagnosed with what test?
delayed gastric emptying (2/2 DM, drugs, postviral) ; [nuclear gastric emptying study]
Clinical manifestations of gastroparesis? (5)
- [succussion splash]
- [early satiety]
- [Abd fullness postprandial]
- [dysautonomia (dizziness, diaphoresis)]
- [labile glucose control]
BE SURE TO R/O MECHANICAL OBSTRUCTION
Name 2 promotility drugs used to treat gastroparesis
- metoclopramide
- erythromycin
When is [screening for diabetic retinopathy and nephropathy] indicated ? (2)
[5y after T1DM dx]
and
[AT TIME OF DX for T2DM]
- give Statin if [age ≥40 with DM]*
What is the preferred antiHTN for DM pts?
ACEk2 inhibitor
_________________
this improves diabetic nephropathy AND INC GFR
Patients with Graves disease have [⬜positive | negative] Thyroid Stimulating Immunoglobulins and ⬜ uptake on [(RadioActive Iodine Uptake) scintigraphy]
Tx for hyperacute [symptomatic Hyperthyroidism] is Cardiac + Thyroid
[Cardiac⬜ PLUS Thyroid[AntithyroidMed1st line or _____or _____]
positive; diffuse
- propranolol
- Thyroid Tx ([AntithyroidMed] vs [Radioactive iodine ablation] vs [Thyroidectomy])

tx = [Propranolol] –> [PTU —(1 hr later)]–> [Potassium Iodine and PrednisoneCTS]
Tx for hyperacute [symptomatic Hyperthyroidism] is Cardiac + Thyroid
[Cardiac⬜ PLUS Thyroid[AntithyroidMed1st line or _____or _____]
Aside from being 1st line tx, when are AntithyroidMeds actually preferred as 1st line as Thyroid tx for [symptomatic Hyperthyroidism]? (4)
- Cardiacpropranolol
- Thyroid ([AntithyroidMed1st line] vs [Radioactive iodine ablation] vs [Thyroidectomysurgery])
a. [mild hyperthyroidism]
b. [Pregnancy (PTU→ MTZ → MTZ)]
c. Elderly(older with limited life expectancy)
d. Prep for [radioactive iodine ablation]

Patients with Graves disease have [⬜positive | negative] Thyroid Stimulating Immunoglobulins and ⬜ uptake on radioiodine scintigraphy
_________________
[RadioActive Iodine ablation] is contraindicated c❌d in pregnancy and lactation
When is it indicated for Graves tx? (5)
positive; diffuse
_________________
- alternative to AntiThyroids(if unable to tolerate)
- alternative to [ThyroidectomySurgery ](if surgery not preferred)
- [SEVERE hyperthyroidism +/- ophthalmopathy]
- [Moderate hyperthyroidism +/- ophthalmopathy]
- [mild hyperthyroidism +/- ophthalmopathy](* PATIENT PREFERENCE *)
C❌D(pregnancy, lactation)
| RAI ablation is useful in Graves/Toxic nodular thyroid since INC uptake concentrates Radioactive isotope in diseased thyroid

Patients with Graves disease have [⬜positive | negative] Thyroid Stimulating Immunoglobulins and ⬜ uptake on radioiodine scintigraphy
_________________
When is [ThyroidectomySurgery] indicated for Graves disease ? (5)

positive; diffuse
_________________
a.{Pregnant (and can’t 1st tolerate [ThionamidesAntithyroid])}
[b. GOITER(LARGE | Retrosternal_obstructive)]
c. [Thyroid CA (suspicion|confirmed)]
d. [1º Hyperparathyroidism superimposed]
e. SEVERE OPHTHALMOPATHY
What do you use to track thyroid function in pt who just started AntiThyroid Rx(drugs vs Radioactive Iodine vs SURGERY)? (3)
- [TSHnml0.4 - 4 (TSH q 4mo if Chronic Amiodarone Rx)]
- [FREE T4 nml0.9 - 1.7]
- [total T3]

[Free T4 = 0.9 - 1.7]
Identify and Explain the finding
What diagnosis does this indicate?

Seidel Sign ⼀concentrated fluorescein uptake (indicating corneal epithelial defect) with subsequent clearing in a waterfall pattern (indicating fluorescein is being washed out by inappropriately draining aqueous humor)
_________________
Full Thickness Corneal laceration

Pt presents with positive Seidel sign
a. Diagnosis?
_________________
b. Management of this diagnosis?
a. Full thickness Corneal LACERATION
_________________
b. ⼀URGENT OPTHO CONSULT!!
If laceration extends through the full thickness of cornea ➜ can create [perforated open globe injury] = STAT SURGICAL REPAIR
_________________
Seidel sign= concentrated fluorescein uptake with subsequent clearing (from draining aqueous humor) in waterfall pattern

How do you manage Corneal Abrasion? -3

- Both insulinoma and [surreptitious med use(Exogenous insulin vs Oral hypOglycemic agents)] can present with hypOglycemia sx*
- _________________*
When is it clinically indicated to workup a patient with hypOglycemia?
ONLY IF [⊕ WHIPPLE’S TRIAD*] = clinical hypOglycemia = workup indicated
- low BG
- [SADHAThypOglycemia sx]
- [SADHATsx] resolve with glucose admin
_________________
*Whipple’s Triad is required because many people have low BG without hypOglycemia sx = not clinically significant hypoglycemia

- Both insulinoma and [surreptitious med use(Exogenous insulin vs Oral hypOglycemic agents)] can present with hypOglycemia sx*
- _________________*
clinical hypOglycemia is characterized by the presence of ⬜
How do you workup clinical hypOglycemia? -4
[⊕ WHIPPLE’S TRIAD] = clinical hypOglycemia = workup indicated
- low BG
- [SADHAThypOglycemia sx]
- [SADHAThypOgluc sx] resolve with glucose admin

- Both insulinoma and [surreptitious med use(Exogenous insulin vs Oral hypOglycemic agents)] can present with hypOglycemia sx*
- _________________*
Why is [HIGH or normal serum Insulin] in a patient p/w hypOglycemia sx concerning and require additional workup? (2)
1) Normally, hypOglycemia ➜ negative feedback ➜ suppression of release of [Insulin/CPeptide/ProInsulin] = [low serum Insulin ✅]
2) If Pt has sx hypOglycemia but [High or normal serum Insulin] there must be an abnormal additional source of Insulin (exogenous vs endogenous) = additional workup

What is the [mixed meal challenge] used for?
evaluates Pts who only have hypOglycemia sx after eating

What lab is ordered alongside C-Peptide to evaluate endogenous insulin production?
Proinsulin

The most common cause of DEC vision in elderly patients are ⬜ with ⬜ .
Why is the evaluation so critical for these conditions? (2)
▶([cortical cataracts] ; [AMD])
▶Elderly Cataracts patients must be thoroughly evaluated for severity of [ccaAMD] since they:
1.may require both [Cataract lens extraction Surgery] AND [ccaAMD] tx (PO eye vitamin)]
or
- may not benefit from [Cataract lens extraction Surgery] at all (since opacified lens prevent [ccaAMD] progression)
[ccaAMD]: (Cortical Cataract) associated -Age related Macular Degeneration

The most common cause of DEC vision in elderly patients are ⬜ with ⬜ .
Describe each condition
([cortical cataracts] ; [ccaAMD])
_________________
[cortical cataracts]: nonpainful slow progressive lens opacification ➜ blurry vision but fields intact
with
[ccaAMD]:(potentially irreversible) loss of central vision due to central retina degeneration ➜ poor reading, scotomas, dim vision, [dry AMD with Drusen], [wet AMD with choroidal neovascularization]
[ccaAMD]: (Cortical Cataract) associated -Age related Macular Degeneration

Similar to CROA amaurosis fugax ⬜ also usually presents with sudden uL nonpainful vision loss
Retinal Detachment
Pt with sudden eye pain, has Visualization of leukocytes in the anterior segment of her eye
Dx?
_________________
What other 5 sx would you expect?
[IritisAnterior Uveitis]
_________________
- photophobia
- pain
- redness
- vision loss
- [irregular constricted pupil]
* 6. [Leukocytes in ANT segment]*

Infectious Keratitis sx (3)
- corneal opacity
- severe photophobia
- difficulty keeping affected eye open

s/p coronary angiography, patient soon after develops palpitations, fatigue, heat intolerance, sweating
Diagnosis? Explain
_________________
Which diagnostics support this dx? (3)
Iodine-induced hyperthyroidism;
[pts with Nodular thyroid dz or Chronic iodine deficiency] have INC risk for thyrotoxicosis following [iodine exposure (radiocontrast for Coronary angio or imaging /amiodarone) .
_________________
[DEC TSH], [⊝thyrotropin R Ab], [US: ⇪ vascularity +/- nodules]
s/p newly starting amiodarone, patient soon after develops palpitations, fatigue, heat intolerance, sweating
Diagnosis? Explain
_________________
Tx for this? (2)
Iodine-induced hyperthyroidism;
[pts with Nodular thyroid dz or Chronic iodine deficiency] have INC risk for thyrotoxicosis following [iodine exposure (radiocontrast for Coronary angio or imaging /amiodarone) .
_________________
- [BBlocker Propranolol]
- [Methimazole (add if Severe hyperthyroidism vs elderly heart disease)]
[Lugol ⬜ solution] is a solution containing ⬜ that does what mechanistically?
Indications? (2)
(LARGE LOAD iodiNe)
_________________
👄 (Wolff-Chaikoff phenomenon) = any [LARGE LOAD iodiNe] →actually paradoxically inhibits TPO (temporarily) → [⬇︎iodiNe organification and coupling] → [⬇︎thyroid hormone synthesis]
👄[Lugol (LARGE LOAD iodiNe) solution] = clinically activates (Wolff-Chaikoff phenomenon) → [⬇︎thyroid hormone synthesis] for:
_________________
1. [prethyroidectomy in Graves disease]
2. [acutethyroid storm tx]

Prednisone is used to treat which 3 thyroid diseases?
- [PDSGT-(Painful Dequervain Subacute Granulomatous Thyroiditis)] *
- [amiodarone destructive Type 2 thyroiditis] *
- thyroid storm ⼀DEC conversion of T4 ➜ [active T3]
_________________
*used in thyroid when destruction of gland ➜ preformed thyroid hormone being released.

[normal Retina] = (⬜-4) on fundoscopy
describe how a [Papilledema Retina] looks on fundoscopy (4)
🔎[Papilledema Retina] = [Retina io\Papilledema]
[normal Retina] = normalDSLs= [Disc margin defined/Small veins linear /Large veins defined]/ [splinter hemorrhage⊝]
_________________
“my Retina loves DSLs”

[Papilledema Retina(Retina in the setting of Papilledema)] = Papilledema⚠️DSLs
= [Disc margin OBSCURED / Small veins SERPENTINE / Large veins OBSCURED] / [splinter hemorrhage⊕]
normal range for
TSH
0.4 ⼀ 4.0
normal range for
[free thyroxine T4]
_________________
[Total Thyroxine T4]
free thyroxine T4[0.9 ⼀ 1.7]
_________________
5-12
“Thyroiditis” suggest ⬜2. And there’s 3 types: PDSGT, hCAT, [NSLP-hCAT]
[NSLPhCAT] : [Nonpainful(silent) Subacute Lymphocytic Postpartum]hCAT
Clinical Features (4)
_________________
Diagnostics (2)
[Lymphocyte infiltration ➜ [Transient HYPERthyroidism]
_________________
- variant of hCAT(dx = [⊕TPO antibody], [low RAIU])
- HYPERthyroid transiently → hypOthyroid (or sometimes Euthyroid) → spontaneous recovery
- GoiterNonpainful, small
- includes postpartum thyroiditis (midaged Women postpartum)
🔎TPO = ThyroPerOxidase

[NSLPhCAT] dx =same as hCAT dx:
a. ⊕TPO antibody
b. low RAI uptake
“Thyroiditis” suggest ⬜2. And there’s 3 types: PDSGT, hCAT, [NSLP-hCAT]
hCAT: [hashimoto Chronic Autoimmune Thyroiditis]
Diagnostics (2)
[Lymphocyte infiltration ➜ [Transient HYPERthyroidism]
_________________
* * *
- ⊕[Thyroid PerOxidase Ab]
- [lowRAI uptake]

“Thyroiditis” suggest ⬜2. And there’s 3 types: PDSGT, hCAT, [NSLP-hCAT]
hCAT: [hashimoto Chronic Autoimmune Thyroiditis]
Clinical Features (5)
{[Lymphocyte infiltration ➜ [Transient HYPERthyroidism]}
_________________
- [initial Transient HYPERthyroid[damage from AntiTPOLymphocytes(= Lymphocytes that secrete AntiTPO Abs) → infiltrate thyroid follicles → [preformed T4/T3/TG] thyroid reservoir release]
- damage ultimately → hypOthyroid(since damage impairs thyroid function)
- GoiterDIFFUSE
- daughter condition = [NSLPhCAT]
- → CA(hCAT can → Thyroid DLBL)

“Thyroiditis” suggest ⬜2. And there’s 3 types: PDSGT, hCAT, [NSLP-hCAT]
PDSGT: [PAINFUL DeQuervain Subacute Granulomatous Thyroiditis]
Clinical Features (5)
[Lymphocyte infiltration ➜ [Transient HYPERthyroidism]
_________________
- Postviral inflammatory process
- self-limited
- PAINFUL DIFFUSE ENLARGED GOITER
- FEVER [from postviral inflammatory process(*etx: viral antigens provoke [CD8 cytotoxic T-lymphocytes] against Thyroid follicles → follicular injury → **</sup>)
- HYPERthyroid(TT Feels ARCHED) symptoms
{PDSGT etx: *(Viral antigen cross rxn) → [PAINFUL autoimmune CD8 follicle infiltration( = large painful goiter, FEVER, ⇪ESR, ⇪CRP)] → [release of stored T4/T3 = transient HYPERthyroid] → DEC TSH → DEC iodine organification → DEC iodine demand = DEC RAIU**}
“Thyroiditis” suggest ⬜2. And there’s 3 types: PDSGT, hCAT, [NSLP-hCAT]
PDSGT: [PAINFUL DeQuervain Subacute Granulomatous Thyroiditis]
Dx labs (3)
[Lymphocyte infiltration ➜ [Transient HYPERthyroidism]
_________________
- - ⇪ ESR
- ⇪ CRP
- [low RadioActive Iodine Uptake]thyroid scintigraphy
{PDSGT etx: *(Viral antigen cross rxn) → [PAINFUL autoimmune CD8 follicle infiltration( = large painful goiter, FEVER, ⇪ESR, ⇪CRP)] → [release of stored T4/T3 = transient HYPERthyroid] → DEC TSH → DEC iodine organification → DEC iodine demand = DEC RAIU**}
“Thyroiditis” suggest ⬜2. And there’s 3 types: PDSGT, hCAT, [NSLP-hCAT]
PDSGT: [PAINFUL DeQuervain Subacute Granulomatous Thyroiditis]
Explain Why does PDSGT have low RAIU??
[Lymphocyte infiltration ➜ [Transient HYPERthyroidism]
_________________
-[Elevated ESR & CRP]labs
-[low RadioActive Iodine Uptake]thyroid scintigraphy
* * *
{*(Viral antigen cross rxn) → [PAINFUL autoimmune CD8 follicle infiltration( = large painful goiter, FEVER, ⇪ESR, ⇪CRP)] → [release of stored T4/T3 = transient HYPERthyroid] → DEC TSH → DEC iodine organification → DEC iodine demand = DEC RAIU**}
“Thyroiditis” suggest ⬜2. And there’s 3 types: PDSGT, hCAT, [NSLP-hCAT]
PDSGT: [PAINFUL DeQuervain Subacute Granulomatous Thyroiditis]
Tx (3)
[Lymphocyte infiltration ➜ [Transient HYPERthyroidism]
_________________
1. [NSAIDs ➜ Prednisone(refractory)]
2. [Propranolol (or Atenolol)]
3. [self limited (viral infxn → [PDSGT HYPERthyroid]3w → hypOthyroid → Euthyroid)]
* * *

{PDSGT etx: *(Viral antigen cross rxn) → [PAINFUL autoimmune CD8 follicle infiltration( = large painful goiter, FEVER, ⇪ESR, ⇪CRP)] → [release of stored T4/T3 = transient HYPERthyroid] → DEC TSH → DEC iodine organification → DEC iodine demand = DEC RAIU**}
On Thyroid Scintigraphy, when do you see Patchy uptake?
Clinical features of this condition (3)
toxic multinodular goiter
- {HYPERthyroidthyrotoxicosis (TT FeelsARCHED)}
- nodular enlargement
- OLDER patients

On Thyroid Scintigraphy, when do you see Diffuse uptake?
why do you see diffuse uptake in this condition?
[Graves1º HYPERthyroidthyrotoxicosis]
_________________
[thyrotropin R autoantibodies] stimulate thyroid diffusely to [INC iodine uptake] and [INC thyroid hormone synthesis]

clinical features of Ocular melanoma (4)
★ [1º malignant melanocytes from uvea(choroidal pigmented nevus)]
★ [identified incidentally frequently] ⼀[gold standard dx = US]
★ {⊝sx or [small (diameter<10mm) (thickness<3mm) pigmented lesion] = [observation (repeat exam in 3 mo, then q6 mo)]}
★ {⊕SX or [LARGE (d ≥10mm)(t ≥3mm)] = XBRT –(if VERY LARGE or extrascleral extension)–> Enucleation
Enucleation: removal of entire globe and intraocular contents
In hospital setting, American Diabetes Association suggest maintaining inpatient glucose at ⬜
140-180
▶Hospitalized [⬜ DM1 | DM2] patients’ basal insulin must be continued at all times in hospital. But because ⬜, inpatient basal insulin has to be DEC by ⬜% from prehospital dose
▶Describe the 3 basic components of Hospital Insulin administration
DM1 (inpatient basal insulin is req’d for ALL hospitalized DM1 patients and most DM2) ; [hospitalized patients eat less than normal = INC hypOglycemia risk] ; [25-50%]
BNC
[BasalLA or IA]= controls glucose between mealsALL DM1 (and most DM2)
[Nutritional bolusSA] = controls postprandial glucose excursionsreq’d only for patients eating obvi
[Correctional bolus Sliding ScaleSA] = corrects random hyperglycemic excursions
_________________
L/I/SA: Long/Intermediate/Short-ACTING
When should you consider insulin infusion pump for IDDM pts (5)
- critical illness
- DKA
- HHONKS
- perioperation
- [(SQ insulin) failure]
nml TSH: [0.4-4.0]
TSH-secreting pituitary adenomas cause ⬜ with elevated ⬜ and ⬜ levels. How can this pituitary adenoma be differentiated from other (FLAT PiG) pituitary adenomas? (3)
central Hyperthyroidism; [TSH] & [T4/T3]
- Although [mass effect (HA, visual ∆ )] = common pituitary adenoma sx…*
- 85% [TSH pituitary adenoma] tumors secrete [biologically inactive alpha subunit] =
- elevated [(Bi)alpha subunit]? = likely from ⊕[TSH pituitary adenoma]
tx = somatostatin analog vs transsphenoidal surgery
Dx?

[NMER]Glucagonoma
(necrolytic migratory erythematous rash)

DAN had a Glucagonoma!
Glucagonoma triad: DM, [NMER (necrolytic migratory erythematous rash)], [Anorexia weight loss]
Glucagonoma is a rare but malignant pancreatic tumor of the [islet alpha cell] that secretes VIP, calcitonin, GLP1 / dx = high glucagon level / tx = surgical</sub>
Sulfonylurea MOA
________________
List examples-5
closes {[pancreatic β islet cell] ATP-sensitiveK+ Efflux channel( which typically closes from ⇪ATP)} → inner cell membrane depolarization → Ca+ INflux → endogenous insulin Efflux secretion = insulin secretagogue
________________
- 2GGlimepir_ide
- 2GGlybur_ide
- 2GGliPiz_ide
4.1GChlorpropamide
5.1GTolbutamide
G = Generation

[MeglitiNides (“RepagliNide, “NategliNide”)] = same MOA as Sulfonylurea
Meglitinide
MOA
________________
List examples-2
insulin secretagogue= (same as Sulfonylurea MOA) stimulates endogenous insulin secretion
__________________
- Nateglin_ide_
- Repaglin_ide_

[Alpha glucosidase inhibitor] MOA
________________
List examples-2
inhibits α-glucosidease ➜ inhibits intestinal carb digestion → ⬇︎postprandial HYPERglycemia
________________
- Acarbose
- Miglitol

[DPP-4 inhibitors] MOD
________________
List examples-2
inhibits [DPP-4 GLP1 peptidase] –> ⬆︎GLP1–> ⬆︎Glucose-induced insulin release
_________________
- SitaGliptin
- SaxaGliptin

What are the GLP1 homologs?-2 ;
What do they do?
- ExenaTIDE
- LiragluTIDE
These require Injections
⬆︎Glucose-induced insulin release

“GLP1a says… “iLAGG behind food”
[⇪insulin secretion & sensitivity⇪[Glucose-induced Insulin Secretion]
[⬇︎Liver Glucose secretion]
[⬇︎ Appetite(secreted after food intake)]
[⬇︎Gastric emptying(⚠️Pancreatitis risk)]
[⬇︎ Glucagon secretion]
Classic Presentation for DM -5
FUDge

Clomiphene Citrate
MOA
_________________
Indication
[hypothalamic estrogen🟥]SERM;
PCOS Infertility

Leuprolide
MOA
_________________
Indication
[GnRH🟢] ; endometriosis
How does respiratory rate affect Calcium levels?
Tachypnea causes ⬇︎CO2 acid –> H+ ions dissociate from albumin so they can help maintain pH –> ⬆︎free albumin which bind to free ionized Ca+ –> overall ⬇︎ in ionized unbound calcium

[Normal serumCa+: 8.4-10.2]
Pt presents with hypOcalcemia
How do you work this up? -5

[Normal serumCa+: 8.4-10.2]
causes of hypOcalcemia can be categorized based on PTH level
What are the causes of [hypOcalcemia(HIGH PTH)]? -6
- vitD deficiency
- Chronic Kidney Disease
- Pancreatitis
- Sepsis
- Tumor lysis syndrome
- pseudohypOparathyroidism

[Normal serumCa+: 8.4-10.2]
causes of hypOcalcemia can be categorized based on PTH level
What are the causes of [hypOcalcemia(low/normal PTH)]? -9
- a. Parathyroidectomy
- b. Thyroidectomy
- c. radical neck surgery
- d. [Polyglandular autoimmune syndrome]
- e. Metastatic CA
- f. Wilson disease
- g. hemochromatosis
- h. [(PTH R) gene mutation]
- i. [(Calcium-sensing R) gene mutation]

cp for Glucagonoma - 3
DAN had a Glucagonoma!
- DM
- Anorexia weight loss
- Necrotic Migratory Erythema (perioral, extremities, perineum)

dx for Glucagonoma
DAN had a Glucagonoma!
Glucagon >500

Look for Necrotic Migratory Erythema!
Pt w hx Graves disease s/p [RadioActive iodine ablation], now with iatrogenic hypOthyroidism.
You’ve just learned, pt may also have Celiac disease.
How is Celiac disease related to Thyroid disease? (3)
★ [Celiacmalabsorption] is common with autoimmune thyroid disease = frequent cause of levothyroxine malabsorption
★ Pt now with iatrogenic hypOthyroidism needs Levothyroxine replacement , but potential [Celiacmalabsorption] will → [constant escalating dose requirements of Levothyroxine]
★ Celiac dx = (elevated serum anti-TED → endoscopy). If ⊕Celiac → gluten-free diet → restores nml Levothyroxine absorption
- Take Levothyroxine [on empty stomach30-60m ac] and [4h before other drugs]*
Pt w hx Graves disease s/p [RadioActive iodine ablation], now with iatrogenic hypOthyroidism.
You’ve just learned, pt may also have Celiac disease.
In pts with hypOthyroidism, name 6 co-conditions that will cause INC requirement for Levothyroxine replacement
- [Malabsorption_Disease (Celiac)]
- [Malabsorption_Rx (iron, Ca+)]
- [catabolic Thyroxine-T4_Rx (INC Thyroxine metabolism: phenytoin, carbamazepine, Rifampin)]
- Obesity
- Pregnancy
- overt prOteinuria
Take Levothyroxine [on empty stomach30-60m ac] and [4h before other drugs]
Explain how patients should take Levothyroxine? (2)
Take Levothyroxine [on empty stomach30-60m ac]
–and —
Take Levothyroxine [4h before other drugs]
Pts with hypOthyroidism will require a [Levothyroxine replacement regimen]
Describe the 3-part [Levothyroxine replacement regimen] for pts with hypOthyroidism
IBM
I: { Initial[75-125mcg/day](or 25-50 for elderly | CVD) }
⬇
B:{ [Boost/INC Dose q6w until TSH nml0.4-4 }
⬇
M: {Maintain & Monitor TSH q6-12months]
- note: elevated TSH despite constant escalating levothyroxine doses = levothyroxine malabsorption (c/s Celiac)*
How is an ovarian tumor related to thyroid regulation?
[Struma Ovarii ovarian teratoma] = rare ovary tumor that ectopically secretes thyroid hormone → [rare ectopicHYPERthyroidism with low TSH]

nml TSH: [0.4-4.0]
clinical features of [NSLPhCAT]
(5)
[Nonpainful Subacute Lymphocytic Postpartum Thyroiditis]hCAT = [(transienthyperT) → ( transienthypOT ) → normalT]
_________________
1. within ≤1 year postpartum {[TPO Ab inflammation] → [release of preformed T4 + preformed Thyroglobulin] → [nonpainful goiter + transienthyperT] }
2. {[transienthyperT] → [transienthypOT with ⬇︎RAIUdue to positive feedback’s_⬇︎TSH] ) → normalT] (PDSGT also)}
3. [variant of hCAT] (PDSGT also)
4. [⊕TPO Ab] ⼀(PDSGT also)
5. [⇪T4, ⇪Thyroglobulin, ⬇︎TSH, ⬇︎RAIU]

What is Thyroglobulin? (2)
used to build thyroid hormone in thyroid follicle, and then co-secreted with endogenous thyroid hormone secretion

= in pts exogenously taking thyroid hormone → [⇪ T4 but ⬇︎Thyroglobulin]
- = Graves disease → [⇪ T4, ⇪ Thyroglobulin]*
- =hCAT (PST, PT) → [⇪ T4, ⇪ Thyroglobulin] (2/2 inflammatory release of preformed T4 and preformed Thyroglobulin)*
Diabetic retinopathy requires years to develop and occurs 2/2 ⬜3. For patients with sx, what’s most likely to improve their sx?
- macula edema
- proliferative diabetic retinopathy [→ vitreous bleeding → retinal detachment = blindness]
- lens edema
improve glycemic control
Amiodarone….is Thyrotoxic lol and TSH should be obtained every 4 months while on chronic Amiodarone therapy
Explain all the mechanisms for how Amiodarone cause thyroid dysfunction? (5)
Amiodarone’s

hypOT1: nml pt[LARGE LOAD IODINE]= Wolff-Chaikoff Effect: [large load iOdine] DEC thyroid hormone synthesis = hypOT)
hypOT2. [intrinsic inhibition (Thyroid hormone synthesis)= hypOT]TX: LEVOTHYROXINE
hypOT3. [intrinsic inhibition (T4 → T3 conversion)= hypOT ]TX: NONE
HyperT1. Nodular/Graves[LARGE LOAD IODINE]= AIT1: large iOdine load INC thyroid hormone synthesis = HyperT)]TX: Antithyroids
HyperT2. [[AIT2]=destructive thyroiditis: ( → preformed T hormone release→ INC thyroid hormone = HyperT )]TX: Prednisone CTS-GC]
[T or F]
TSH should be obtained once a year for patients on chronic amiodarone therapy
FALSE
chronic Amiodarone pts require TSH every 4 months
Pts taking Levothyroxine must take it [____ with water] ⬜ minutes before breakfast.
[Calcium supplements] and [Iron supplements] ⬜ absorption of levothyroxine; thus Ca+/Fe should only be taken ≥ ⬜ hours after taking levothyroxine.
on empty stomach; 30-60m
PREVENT; 4h ;
otherwise Ca+/Fe may possibly cause worsening hypOT in pts taking Levothyroxine
Why does T2DM rarely present with ketoacidosis at disease onset? (2)
T2DM does not involve absolute insulin deficiency (like T1DM) and glucose metabolism is sufficient to prevent ketosis
What is [monogenic DM (MODY)]? (3)
MDM [(Monogenic DM (Maturity Onset DM of Young)]:
- AUTO DOM EARLY ONSET DM = 2-3 GEN FAM HX
- defective glucose sensing and defective insulin secretion
- Young/normal wt but early DM
What are the 4 ways to Diagnose DM
“Having Treats Feels Risky”

note: Asymptomatic patients with Abnml screening require a repeat of the same test on a different day for confirmation
Central Retinal artery occlusion
symptoms (4)
Vision Loss that’s…
- monocular
- [Severe BUT nonpainful
- …with temporal sparing]
- [hx of amaurosis fugax]

Central Retinal artery occlusion
management (4)
- optho consult
- intraarterial thrombolytics
- ocular massage
- IOP reduction (ANT chamber paracentesis)

Central Retinal artery occlusion
clinical findings -2
- [Pale fundus(2/2 diffuse ischemia)]
- [cherry red macula]

Central Retinal Vein occlusion
symptom
blurred-to-severe nonpainful vision loss

Central Retinal Vein occlusion
clinical finding
Blood & Thunder (Fundus w retinal hemorrhages & optic disc edema)

Central Retinal Vein occlusion
management -2
[Observation]
[+/- intravitreal injection of VEGF inhibitors]

[Torn Retinal Detachment]
symptoms (3)
- Floaters
- [Flashing lights(Photopsia)]
- {[Field of periphery nonpainful vision loss 1st]→ [central nonpainful vision loss 2nd]}= “Descending Visual Curtain” progressive vision loss

[Torn Retinal detachment]
clinical findings (2)
- marked elevation of retina
- Vitreous hemorrhage

Retinal detachment
management
Surgical correction (retinopexy, vitrectomy)

Vitreous hemorrhage
symptom (4)
- [Hazy vision +/- red hue]
- nonpainful vision loss
- Floaters
- Shadows

Vitreous hemorrhage
clinical findings (3)
- [red reflexabsent or DEC ]
- floating debris/RBC in Vitreous
- obscured fundus view

Vitreous hemorrhage
management (3)
- Bed rest with 30-45° Head-Of-Bed elevation
- photocoagulation
- vitrectomy (some cases)

What are the 4 causes of [acute nonpainful vision loss]?
CCTV is a nonpainful way to look😏 ✅
- Central Retinal occlusion⼀arterypale fundus + cherry red spot/amaurosis fugax hx
- Central Retinal occlusion⼀VeinBlood & Thunder fundoscopy
- Torn (Detached) RETINA[flashing lights Photopsia]
- Vitreous hemorrhagehazy vision/red hue/absent red reflex/floating debris

What are the most common causes of this condition? (4)

CAROTID ARTERY ATHEROSCLEROSIS > cardiogenic embolism, clotting DO, [giant cell arteritis (vasculitis)]
- Central Retinal artery occlusion*
clinical presentation of Optic Neuritis (3)
- [subacute (hours to days)] monocular PAINFUL vision loss ⼀ pain worse with eye movement.
- Fundoscopic optic disc edema
- (+/- afferent pupillary defect)

[Functional Pituitary Adenomas] consist of what 3 adenomas?
________________
Describe etx of [NONFunctional Pituitary Adenoma]
________________
Tx?
Functional Pituitary Adenoma=
Lactotrope > Somatotrope > Corticotrope
[NONfunctional pituitary adenomas] arise from [LH/FSH Gonatrope cells of the PITUITARY GLAND ➜ unique [isolated ⇪ (nonfunctional)αlpha subunit] ➜ [⊕feedback on hypothalamusGonatrope] → [decreased low LH/FSH gonadotropin levels] ➜ hypOgonadism
+
mass effect if tumor large enough
Tx = Trans-Sphenoidal Surgery

Why do pts with hypOthyroid require INC dose of levothyroxine if they start taking estrogen-containing OCP?
________________
how is this managed?
Estrogen stimulates liver to make ⇪ [thyroxine binding globulin] ➜ ⇪ binding sites to saturate➜ DEC free T3/T4
Normal thyroid ⇪ [free T3/T4] to saturate the additional TBG binding sites
BUT hypOthyroid patients are unable to INC thyroid hormone synthesis
________________
get TSH weeks after starting Estrogen-OCP and titrate to normal thyroid function
⬜ is the leading cause of death in pts with Acromegaly. What other comorbidity are they at risk for?
________________
which comorbidity is reversible with treatment?
[Cardiovascular disease (REVERSIBLE)] ; Colon CA
________________
Cardiovascular Disease is reversible with tx

[Anabolic Androgen Steroids] ➜ symptomatic ⬜ from DEC ⬜
________________
how long after d/c does it take to naturally recover?
hypOgonadism ; endogenous testosterone
________________
recovers weeks/months after d/c but will be permanently suppressed if chronic abuse

[Anabolic Androgen Steroids]
clinical features -8
MEATHEAd
- [Muscle mass ⇪]
- ERYTHROCYTOSIS
- Aggression
- [(Testosterone/LH/FSH DEC )→ (Testicular size DEC) + (spermatogenesis DEC)]
- [HLD( ⇪ LDL|⬇︎HDL)]
- [Erection & Libido[(normal during use) / (DECREASED DURING WITHDRAWAL)]
- Acne
- doubleD-Gynecomastia

Describe insulin regimen for IDDM or Type 1
________________
Basal + [3 prn meal]
- basal = [NPH BID] or [GluLargine QD]*
- ________________*
- 3 prn meal = [3 reg insulin c meals]*
what adjustments should be made for exercise induced hypoglycemia in a IDDM/Type 1 DM? -3
- [⬇︎basal insulin (NPH BID vs GluLargine QD)]
- eat before exercise
- avoid insulin injection into “exercise” limbs
tx Conjunctivitis -10
CAPE ⼀ CAD ⼀MAD
- B-[ContactLens → Fluoroquinolonedrops]
- B-[Azithromycindrops]
- B-[Polymyxin-trimethoprimdrops]
- B-[Erythromycin<u>ointment</u>]
- V-[CompressWarm/Cold]
- V-[Antihistaminedrops]
- V-[Decongestantdrops]
- A-[Mast cell stabilizer]freq episodes
- A-[Antihistaminedrops]intermittent/freq episodes
- A-[Decongestantdrops]freq episodes

⬜ is a rare complication of bacterial conjunctivitis and is managed with ⬜
_________________
How does this complication typically present? -3
Keratitis (inflammation of cornea) ; URGENT OPHTHALMOLOGY CONSULT FOR TX
_________________
[foreign body sensation] / photophobia / vision impairment

What is a [Hordeolum Stye]
bacterial infection of [eyelid sebaceous gland]

Why do pts with suspected Keratitis must receive URGENT OPHTHALMOLOGY CONSULT?
_________________
How is Keratitis diagnosed?
Keratitis can cause corneal scarring which ➜ blindness if untreated by optho
_________________
slit-lamp
How is Viral Conjunctivitis spread? -2
EYE DISCHARGE directly
Contaminated Surfaces

[T or F]
Crusted over eyes in the morning indicates patient is contagious with viral conjunctivitis
FALSE
(only EYE DISCHARGE and contaminated surfaces transmit viral conjunctivitis)
What are the two definitive treatments for thyroid disease
- Radioactive Iodine
- Thyroidectomy

Potassium Iodide Indication - 2
- PreOp tx for Thyroidectomy in Graves
- Thyroid Storm

How does looking at Thyroglobulin levels help determine etiology of thyroid disease?
Thyroglobulin is the base needed to make thyroid hormone.
If thyroid hormone is elevated…and Thyroglobulin is also elevated then Thyroid is naturally producing a lot of thyroid hormone
________________
If thyroid hormone is elevated …but Thyroglobulin is low then that means thyroid hormone must had been exogenousouly given

tx for Thyroid Storm - 3
HHH needs PPP
tx = [Propranolol] –> [PTU —(1 hr later)]–> [Potassium Iodine and PrednisoneCTS]

cp for Thyroid Storm - 3
HHH needs PPP
Hot, Head and Heart
- Hot = Fever
- Head = CNS dysfunction with tremor
- Heart = Tachycardia, palpitations, HTN, HF
________________
tx = [Propranolol] –> [PTU —(1 hr later)]–> [Potassium Iodine and PrednisoneCTS]

What is this a complication of?

Acute Sinusitis
________________
dx: Orbital Cellulitis
tx for [Toxic Adenoma Thyroid Nodule] -3
[PreTx (Methimazole)]
➜
[DefinitiveTX (RADIOACTIVE IODINE ABLATION OR SURGERY)]
characteristic features of [Toxic Adenoma Thyroid Nodule] -2
SYMPTOMATIC HyperThyroid
+
[Radioiodine uptake in nodule] with suppressed uptake in remainder of gland]

What’s the single most important risk factor for Osteoporosis?
AGE
_________________
less RF: fam hx / smoking / EtOH
Chronic Granulomatous Disease is a (⬜(Mode of Inheritance?)) that usually p/w ⬜ shortly after birth from ⬜
_________________
MOD for Chronic Granulomatous Disease
[X-linked recessive 1° immunodeficiency] ; recurrent infections ;
[catalase positive organisms (Aspergillus = MAJOR COD / Staph A=liver/skin abscess/adenitis)]
_________________
[Loss of NADPH oxidase] impairs intracell killing of [phagocytosed bacteria and fungi] ➜ recurrent infections
Macular degeneration affects [⬜ central | peripheral] vision,
while Glaucoma affects [⬜ central | peripheral] vision
central
- -[straight lines appearing curvy (wet/exudative-neovascular= aggressive and uL] while*
- -[dry/atrophic=gradual and BL)]*
- “Of course Mac is the Center!”*
- *
peripheral
[Glaucoma –> Gradual tunnel vision (from gradual loss of peripheral vision)]

clinical presentation for [Open Globe Laceration] -2
___________________
what causes this injury?
_________________
management? -4
teardrop pupil and [DEC visual acuity]
_________________
[small sharp objects penetrating globe at high velocity]
_________________
[IV abx / eye shielding / eye CT / Optho consult]

Elevated Calcitonin in pts with [Medullary Thyroid CA s/p total thyroidectomy] indicates ⬜?
_________________
next steps? -3
METASTASIS
_________________
[metastatic medullary thyroid CA dx] ➜ [CT neck/chest (look for metastasis)] ➜ Surgical Resection
What type of goiters develop from iodine deficiency?
_________________
How do you treat [retrosternal goiter w/compressive sx]?
multiNodular
_________________
Surgery
nml TSH: [0.4-4.0]
[Subclinical Hyperthyroidism Thyrotoxicosis] is defined as ⬜2
_________________
When is treatment indicated for [Subclinical Hyperthyroidism Thyrotoxicosis] -4
[low TSH] with [normal free T4]
_________________
* ONLY Treat(Antithyroid v RAI ablation) IF
- [TSH < 0.1]
- or [≥65 yo]
- or [⊕comorbidities (heart disease, osteoporosis)]
What is the Tuning Fork test ?
easy, inexpensive screen that assess for loss of 2TVP (usually of the BL feet) in DM
2TVP = 2-point/Touch/Vibration/Proprioreception
How do you treat diabetic neuropathy? (4)
[AGGRESSIVE GLYCEMIC CONTROL]
+
[Neuronal transmission adjusters (Duloxetine|Gabapentin-Pregablin|TCA)]
a. What role does adrenal gland play in sepsis physiology?
________________
b. What are [stress dose steroids] ?
_________________
c. What is the actual [stress dose steroids] dose for treating sepsis ?
a. normally, [stress (sepsis, surgery)] ➜ adrenal gland ⇪ [endogenous CortisolGlucocorticoid CTS] ➜ [⇪ adrenergic receptor sensitivity to catacholamines] ➜ [⇪ peripheral vasconstriction and ⇪ cardiac contractility] = MAINTAINS BLOOD PRESSURE DURING STRESS
________________

b. pts chronically immunosuppressed (RA on prednisonefor > 3 weeks) have hypofunction of adrenal glands (due to iatrogenic Cushing syndrome) = [relative cortisol deficiency during [stress/sepsis/surgery]➜ require [exogenous corticosteroid] = [stress dose steroids]
_________________
c. [Hydrocortisone IV 200 mg/day]to prevent/treat septic shock
What is [Inferior petrosal sinus sampling] used for?
In patients with elevated ACTH, differentiates source of ACTH ( [Corticotrope Functional Pitutiary Adenoma] vs [Ectopic (SOLC)] )

What level of prolactin indicates a Prolactinoma
>200

Prolactin inhibits LH release
Clinical Presentation of of Anterior Uveitis(4)
_________________
(C**a**LEB)
Constricted pupil / ANTERIOR UVEITIS / Limbus erythema / Eye pain / Blurred vision

Uveitis is associated with which conditions? (4)
systemic inflammatory DO
1. sarcoidosis
2. RA
3. JIA
4. HLA-B27

(C**a**LEB)sx
In an eyelid laceration, visible fat within the wound indicates a ______ injury
________________
This raises concern for injury to which structures? -2
orbital septal injury
________________
postseptal structures (Extraocular Muscles + eyelid retractors)

Between NPH and [long acting insulinDetemir/GLargine/DeGLudec] which is more likely to cause hypOglycemia?
NPH
NPH Peak effect MORE likely to → hypOglycemia

Microalbuminuria is an indicator of __(3)___.
What lab value is used and what are the values for normal, micro and macro?
- DM
- HTN
- PSGN
Urine [Albumin-Creatinine Ratio];
30-300
normal = < 30
micro = 30-300
MACRO = 300+
MOD for [High Output Heart Failure]

Causes of [High Output Heart Failure] -7
________________
What’s the most common?

[High Output Heart Failure] clinical presentation -3
- Edema (pulmonary & peripheral)
- warm extremities
- [systolic flow murmur with laterally displaced PMI]

what is [sub-clinical hypOthyroidism] ? -2
(INC TSH)
but
(normal [T4 Thyroxine])
most common cause of [sub-clinical hypOthyroidism] ?
hCAT

_________________
[hashimoto Chronic Autoimmune Thyroiditis]
how do you know when [subclinical hypOthyroidism] is advancing to hypOthyroidism
[INC anti-TPO (antiThyroid PerOxidase)]

[subClinical hypOthyroidism] puts females at risk for ⬜ complication?
PREGNANCY
(spontaneous abortion/preeclampsia, abruptio placenta)
cp of hypOpituitarism - 5
FLAT PiG
- FSH/LH ⬇︎ –> Amenorrhea, testicular atrophy
- ACTH ⬇︎ –> ⬇︎Cortisol BUT NOT ALDOSTERONE –> hypotension from ⬇︎arterial resistance
- TSH⬇︎ –> Fatigue/hypOthyroidism
- Prolactin⬇︎ –> LACTATION FAILURE (1ST SIGN OF SHEEHAN!)
- GH⬇︎ –> Anorexia
In hCAT , which antibodies are responsible for the attack on the thyroid gland?
_________________
hashimoto Chronic Autoimmune Thyroiditis
AntiThyroidPerOxidase

AntiTPO is also a/w miscarriage!!
sx of hypOglycemia (6)
low blood glucose gives you SADHAT
- Seizure
- AMS
- Diaphoresis
- HA
- Anxiety
- Tremor
labs for [factitious use of insulin]? -3
serum :
I Conceal Glucose
- 🔝 insulin
- ⬇️ cPeptide
- ⬇️ glucose
Zollinger Ellison
etx
_________________
cp-2
gastrin producing tumor in pancreas or duodenum –> [⬆︎⬆︎gastric acid > 1000] –>
- multiple duodenal/jejunal ulcers REFRACTORY to PPI
- steatorrhea from pancreatic enzyme inactivation
Be sure to screen Zollinger Ellison pts for MEN1 using PTH, Ca+ and Prolactin studies

for IDDM, how much daily insulin should be prescribed?

What things cause HYPERKalemia? -6

What are the opthalmological complications of DM-3; what causes them?
- Retinopathy (from ⬆︎VEGF –> abnormal angiogenesis)
- Glaucoma (⬆︎ Sorbitol eye pressure)
- Cataracts (Glycation of Ocular lens

What happens to [total thyroid hormone] serum level when drugs displace thyroid hormone?
________________
Which drugs do this?-3
[free hormone displacement] ➜ [Thyroid production ⬇︎] –> ⬇︎TOTAL thyroid levels but normal free hormone levels
- ASA
- Furosemide
- Heparin
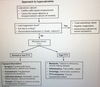
Precocious puberty occurs in [girls less than ⬜ years old] and [boys less than ⬜ years old]
________________
How do you work this up?(see image)

[G<8], [B<9]

Precocious Puberty = [g<8] [b<9]
A pt has just been diagnosed with [Gonadotropin Dependent (Central) Precocious Puberty]
What are the major causes of this?-2
IDIOPATHIC > Pituitary tumor
ALL PTS WITH THIS SHOULD UNDERGO CONTRAST BRAIN MRI REGARDLESS OF +/- HA/VISION SX. Precocious Puberty may be the first sign before the tumor

Danazol MOA
________________
Indication
testosterone derivative with progestin effects
________________
endometriosis
Teenage boy comes in with gynecomastia
How do you work this up?
YOU DONT! - Pubertal gynecomastia is seen in up to 66% of teenage boys mid-late puberty. It can be uL, BL and/or painful
Tx = self-limited to ≤2 years
How long does it take [RAI ablation] therapy to treat Hyperthyroidism?
_________________
How does radioiodine therapy actually worsen Graves ophthalmopathy?
- RAI: RadioActiveIodine*
1-4 mo
_________________
RAI eventually –> hypothyroidism –>⬆︎ thyroid stimulating autoantibodies –> stimulate [orbital fibroblast] → expands [orbital tissue]
Riedel thyroiditis MOD
progressive fibrosis of thyroid gland and surrounding tissue (that looks like CA)

cp for HyperParathyroidism - 4
Painful Bones([brown tumor], [VR osteitis fibrosa cystica], fx, pseudogout)
Renal Stones (Nephrolithiasis, Polyuria)
Abdominal Groans(constipation, pancreatitis, peptic ulcer, cholelithiasis)
Psychic Moans(Depression, Seizure)

Acromegaly cp - 13
etx: GH stimulates IGF1 secretion most of day –> acromegaly sx

Acromegaly Dx (6)
etx: GH stimulates IGF1 secretion most of day –> acromegaly

Acromegaly etx
GH stimulates IGF1 secretion most of day –> Acromegaly

⊝GH secretion is ⬇︎ by glucose and somatostatin
⊕GH secretion is ⇪ by EXERCISE and SLEEP
How does immobilization affect Ca+ levels
INCREASES
Immobilization –> ⬆︎osteoclast activity –> ⬆︎serum Ca+
Acute Rhabdomyolysis causes Ca+ to (⬜ [increase/decrease]) because of what?
DECREASE
________________
release of Ca+ and Phosphorous from damaged muscles –> CaPhosphate precipitation –> drops free serum Ca+
________________
HYPERcalcemia and HYPERphosphatemia can occur later during the remobilization phase during recovery
iCa+ = 0.76 - 1.49
How does [serum albumin] levels affect [ionized Ca+] levels?
IT DOESNT!

[serum albumin] does NOT affect iCal+
_________________
_________________
when *BOUND*albumin*which is neutral* ⬇︎(i.e. liver dz) → ⬇︎[ Ca⊕ normally bound to [albumin]] → ⬇︎[TOTAL Ca+].
__ __ __
{{ ⬇︎boundAlb 1.0 = ⬇︎TOTALCa+ 0.8}}
_________________
_________________
when [FREEalbumin(which is ⊝)] ⇪ → likely knocks off Ca⊕ from [anions] → ⬇︎[TOTAL Ca+].
[TOTAL Ca+].
_________________
_________________
Tx for PCOS - 5
[Wt loss–> SOCK]

SOCK:Spironolactone,OCP (1st line after wt loss),Clomiphene for infertility,Ketoconazole
________________
etx: DM/Obesity–>Hyperinsulinemia which –> ⬆︎⬆︎⬆︎LH secretion –> ⬆︎ovarian theca Androgen secretion –> Sx
Which CA is known for producing calcitonin?
[Medullary Thyroid Carcinoma]

also produces ACTH and VIP
associated with MEN2A and 2B
Why should pts with [Medullary Thyroid Carcinoma] have a fractionated metanephrine assay ordered?
Screen them for Pheochromocytoma

MTC and Pheochromocytoma are associated with MEN2A and 2B
How do you treat [Papillary Thyroid Carcinoma] - 3
Surgical Resection –> +/- radioiodine ablation and suppressive doses of thyroid hormone (in pts with risk of recurrence)
How is Mg associated with Ca+ levels
low Mg+ (especially in alcoholics) –> ⬇︎PTH hormone release and PTH resistance —> ⬇︎serum Ca+ AND low serum K+
serum Phosphorous levels are NOT affected by this phenomena!
What are the distinguishing features of Pancreatic VIPoma - 5
- Tea colored watery secretory diarrhea
- hypOkalemia
- hypOchlorhydria (from ⬇︎gastric acid)
- HYPERcalcemia from ⬆︎bone resorption
- Facial flushing

tx = octreotide for diarrhea
Pts with untreated Hyperthyroidism are at risk of developing what conditions? - 2
- Bone loss from ⬆︎osteoclast activity
- cardiac tachyarrhythmias
Hyperthyroidism = Graves > toxic adenoma > multinodular goiter
What is the most common side effect of AntiThyroid drugs? (i.e. Methimazole, PTU)
agranulocytosis
- Pt on AntiThyroid drugs who develop sore throat with fever should have WBC checked!*
- Radioactive Iodine tx can –> worsening ophthalmopathy*

In HYPERthyroidism, what is the mechanism for why pts have HTN?
⬆︎Myocontractility and HR

Why are pts who receive > 1 unit of pRBC or whole/blood transfusion at risk for hypOcalcemia?
pRBC and whole blood CONTAIN CITRATE
and citrate chelates Ca+ and chelates Mg → DEC Ca+ and DEC Mg
–> paresthesias, Chvostek, Trousseau, Hyperreflexia
Leukoreduction ⬇︎[Febrile Nonhemolytic Rxn] risk from transfusion

What is the most beneficial therapy to ⬇︎ the progression of DM nephropathy?
BP control < 130/80
do not push HbA1C < 7%
A Pt with Hyperthyroid pt develops Sore throat and Fever after being started on Methimazole
What should you assess for?
agranulocytosis
D/C the drug!
- Pt on AntiThyroid drugs who develop sore throat with fever should have WBC checked!*
- Radioactive Iodine tx can –> worsening ophthalmopathy*

A woman starts to rapidly develop facial and body hair
What test do you order first to determine etiology? - 2
DHEA and Testosterone
Hyperandrogenism suggest androgen secreting CA of ovary or adrenal glands so these test will help to determine that
Describe Euthyroid Sick Syndrome (2)
- ISOLATED low T3
- can occur anytime the body is “sick”
[Euthyroid Sick (low T3) Syndrome]
Which microscopic finding is associated with Papillary Thyroid CA?
Psammoma bodies (large lamellated calcifications with ground glass cytoplasm)
Why can’t [Follicular Thyroid CA] be evaluated with fine needle biopsy?
FTC involves invasion of the tumor capsule and/or blood vessels which can only be examined via surgical excision
This is also the reason FTC has the tendency to hematogenously spread
Tx for {[Prolactinoma 1-3cm] or Symptomatic} - 3
Prolactinoma dx = Prolactin > 200
- Cabergoline dopamine R agonist OR
- Bromocriptine dopamine R agonist
- Transsphenoidal resection if refractory

Tx for Prolactinoma >3cm
Prolactinoma dx = Prolactin > 200
Transsphenoidal resection surgery
{[Prolactinoma 1-3cm] or Sx⊕}= Cabergoline|Bromocriptine|Sgry prn

Graves Ophthalmopathy etx
________________
risk factors?-2
Activated T cells and Thyrotropin Autoantibodies both stimulate retroorbital fibroblast –> orbital tissue expansion
________________
Smoking, Female

cp for DM [LARGE nerve fiber] damage
________________
cp for DM [small nerve fiber] damage
[LARGE eNormous nerves] –> NEGATIVE SX = [NO 2TVP] [NO ankle reflexes]
________________
[small petit nerves] –> positive sx = pain, paresthesias
cp for [Klinefelter XXY] ?-6
- small phallus
- [hypOgonads (small testes)]
- hypOspadia
- gynecomastia
- Cryptochidism
- Eunuchoid body

Why do pregnant patients or patients started on OCPs require increased doses of levothyroxine if they’re taking it
Estrogen –> ⬇︎clearance of Thyroid Binding Globulin –> additional TBG binds up all the free T4 –> ⬇︎free T4

[Toxic Adenoma 1ºHyperthyroid-thyrotoxicosis] MOD
autonomous production of thyroid hormones from hyperplastic thyroid follicular cells

if multiple uptake present, consider multinodular goiter
How does looking at Thyroglobulin levels help determine etiology of thyroid disease?
Thyroglobulin is the base needed to make thyroid hormone.
If thyroid hormone is elevated…and Thyroglobulin is also elevated then Thyroid is naturally producing a lot of thyroid hormone
________________
If thyroid hormone is elevated …but Thyroglobulin is low then that means thyroid hormone must had been exogenousouly given

What is Conn’s syndrome
Primary Hyperaldosteronism
List the ophthalmoscopy findings for [simple Diabetic Retinopathy] - 3
_________________
What procedure prevents this?
- microhemorrhages
- retinal edema
- exudates
Argon laser photocoagulation
What are the precipitants of Pheochromocytoma?-3
________________
which medication should be given prior to these precipitants?
Don’t GAS a Pheochromocytoma
- General Beta Blockers (allows unopposed [α] stimulation)
- Anesthesia
- Surgery
Phenoxybenzamine (irreversible general alpha blocker)
PTHrelatedProtein is associated with Cancer (Humoral Hypercalcemia of Malignancy)
________________
What is the major mechanism difference between PTHrP and PTH?
PTH ⬆︎ conversion of [25VitaminD] to [1-25VitaminD]
PTHrP comes from [SQC, breast, renal, bladder, ovarian]
What are the triggers of Thyrotoxicosis - 5
- iodine contrast
- infection
- childbirth
- surgery
- trauma

What is the best way to monitor a pt being treated for DKA - 2
- Serum Anion Gap
- Beta Hydroxybutyrate levels
Primary Hyperparathyroidism and Familial hypocalciuric Hypercalcemia both present with serum Ca+ that is _____ (low/high)
How do you differentiate the two?
HIGH
FHH = [urine calcium : creatinine ratio < 0.01]
Primary Hyperparathyroidism = uccr>0.02
Sialadenosis etx
NONinflammatory swelling of the salivary glands caused by liver disease or malnutrition (DM, bulimia)
Demeclocycline MOA
________________
Indication?
inhibits ADH-mediated renal cortical collecting duct aquaporin insertion
________________
SIADH
Tolvaptan MOA
________________
Indication?-2
TolVaptan = [V2 vasopressin ADH R blocker] ;
- [severe HF Hypervolemia]
- [refractory SIADH]
In pts with Diabetes Insipidus, how do you differentiate between Central and Nephrogenic causes?
Water Deprivation Test
give Demopressin AVP after water deprivation and if urine becomes more concentrated = Central DI. If no change = nephrogenic DI. This is ALSO helpful for r/o Primary Polydipsia
___________________________x____________________________________
DI = inability to concentrate urine 2/2 [(central DI)⬇︎ADH] vs [(nephrogenic DI)renal ADH R⼀resistance]
cp for Primary Hyperparathyroidism
Asymptomatic Hypercalcemia
Hypercalcemia sx: Painful Bones, Renal Stones, Abd Groans and Psychic Moans
A DM pt is not well managed on single therapy Metformin
Out of the other DM drug classes, which is most effective for inducing weight loss?
[GLP1 agonist (exenatide, liraglutide)]

A DM pt is not well managed on single therapy Metformin
When is it appropriate to consider adding insulin?
HBA1c > 8.5%
A DM pt is not well managed on single therapy Metformin
Out of the other DM drug classes, which have the potential to actually cause weight gain?-3
Insulin
[Thiazolidinediones (pioglitazone)]
Sulfonylurea
“Insulin Tops Scales”
etx for Prader Willi Syndrome
_________________
cp?-4
“short, Phat & retarded”
PATERNAL deletion of chromo15q11 thru 13 ;
- HyperPhagia –> Phat (Obesity), Gastric rupture, DM2
- hypOtonia
- short stature
- Mentally retarded
etx for Angelman Syndrome
_________________
cp?-4
“short, sMiling & retarded”
maternal deletion of chromo15q11 thru 13 ;
- Frequent sMiling/Laughter (Moms make you smile)
- Hand Flapping
- short stature
- mentally retarded
explain how DM destroys nerves
deposition of [glycosylation products], [oxidative stress] and [microvascular injury] all –> small nerve AND Large nerve-length dependent axonopathy
What is the most common cause of primary hypogonadism in males?
Klinefelter XXY

[McCune Albright] syndrome etx?
all [McCune Albright] does is P P P
etx = autonomous activity of endocrine tissue from defect in cAMP kinase
causes of hypOparathyroidism -5
- surgery(inadvertent removal)
- Autoimmune hypOparathyroidism
- Congenital(failure to develop = DiGeorge vs 22q11 syndrome)
- [Familial Isolated hypOparathyroidism](Rare mutation in PTH precursor)
- [AutoDOM hypOparathyroidism](CaSR gain-of-function mutation)

hypOparathyroidism sx-7
TQT + BOD + Chvostek

Trousseau(cutting off Tricep/forearm circulation causes Carpal Spasm)
QT prolongation
[Tetany (Seizures/spasm)]
Brain(Parkinsonism/ ⇪ ICP)
Ocular cataracts
Dentition abnormalities
Chvostek(tapping along [Cheek-facial CN7) causes {Mouth/Nose/Eye-Contraction})
PseudohypOparathyroidism
clinical features -4
- Organ resistance to PTH
- AutoDOM
- short 4th and 5th digits
- short stature

The [Parathyroid gland] secretes ⬜ when the [⬜ receptor] detects ⬜
PTH; CaSR;
[(free ionized Ca+) ⬇︎]

Name all the functions of [PTHParathyroid gland] - 6
- [ ⇪ Ca+ bone resorption(via osteoclast activation) → ⇪ serum Ca+]
- [⇪renalPCT Ca+ reabsorption]
- [⇪GI Ca+ absorption]
- renally kicks out (P)
- Converts [inactive 25(OH)VitD] to [active 1,25(OH)2VitD]
- Intermittent PTH[⇪bone formation by activating osteoBlast]

[Slit Lamp Exam] indication
Evalutes for abnormalities of ANT eye (conjunctiva, cornea, ANT chamber, iris)

diagnosis?
________________
What’s the most common cause?

Vitreous Hemorrhage
________________
DM
Fundoscopy = Dark Red Glow with Loss of Fundus details

Causes of Corneal Abrasion - 3
________________
How do you diagnose Corneal Abrasion?
- Trauma
- Foreign Body under eyelid
- Contact lens –> Corneal epithelial defect
________________
Fluorescein exam revealing corneal staining defect
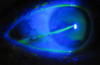
Glaucoma etx -3
⇪ intraocular pressure from…
_________________
[⇪⇪ AH inflow/production](tx = BB|[α2 R agonist] | CAI)
- -or - - -
[⬇︎⬇︎AH uveoscleraloutflow = OaG](tx = Latanoprosttopical prostaglandin)
- -or - - -
_________________
[⬇︎⬇︎AH trabecularoutflow = CaG](tx =Muscarinic agonist )
- [AH: Aqueous Humor] |[OaG/CaG: Open/Closed angle Glaucoma]*

Name the 5 Rx for chronic Glaucoma Tx (5)
________________
how specifically does B-blockers work?

Glaucoma Problem 1: [⇪⇪ AH inflow/production] (tx = β🟥|α2🟢| CAI)
_________________
Problem 2[⬇︎⬇︎AH uveoscleraloutflow](tx = [Prostaglandin🟢 LatanoprostTOPICAL]
_________________
Problem: 3[⬇︎⬇︎AH trabecularoutflow](tx =[Muscarinic🟢Pilocarpine </sup>]

β🟥 –> ⬇︎Aqueous humor secretion from Ciliary Epithelium
What target organ does the M3 Receptor work in (6)
“[M1s need Brain], [M2s need Heart], [M3s BEGs for Private Lounges”
“An M3 BEGS for Private Lounges”
Bladder(contraction) / Eyes / GI / Skin / [Peripheral Vasculature] / Lungs
What are the causes of [Acute Closed Angle Glaucoma]? -3

Anticholinergics / Sympathomimetics / Dim light

_________________
“Closed angle needs OPMAT .. STAT!”
What is the major complaint pts with Glaucoma have?

Gradual Tunnel Vision

HIGH tone hearing loss = [⬜ sensorineural | conductive] hearing loss
Sensorineural
Which is more efficient at transmitting sound between Bone and Air?
________________
Why?
AIR!

________________
Air interacts with ossicles FIRST, which Amplifies the sound conduction to cochlea
Ophthalmoscopy findings include cupping of the optic disc
Diagnosis?
Glaucoma
________________
Glaucoma affects peripheral vision –> tunnel vision! OAG is more common in Blacks

👓cupping is caused by thinning of outer rim of optic disc head
etx of Cataracts
________________
What are the most common presenting sx of Cataracts? -2

[⇪ lens opacity] –>
- [gradual BL NIGHT VISION ⬇︎]
- halos around lights
________________
Fundoscopy eventually shows lost of red reflex and retinal details

What is the treatment for Emergent Acute [Closed angle Glaucoma] - 5
“Closed angle needs OPMAT .. STAT!”
[OPHTHO CONSULT STAT!(for Emergent Iris resection!)]
Pilocarpine[Cholinergic M3 R agonist]
Mannitol
AcetazolamideCAI
TimololBB

diagnosis?

Retinoblastoma leukocoria

Dx for [Acute Closed angle Glaucoma] -2
Gonioscopy vs Ocular Tonometry

_________________
“Closed angle needs OPMAT .. STAT!”
diagnosis?

Zoster Ophthalmicus
________________
finding = Dendriform Corneal Ulcer

MOD for Trachoma
_________________
cp for Trachoma-2
Repeated Eye infections with Chlamydia Trachomatis A,B,C –> Inversion of Eyelashes
_________________
(INVERTED & PALE EYELASH HAIR FOLLICLES with Conjunctival injection) –> [Blindness from lash ulceration]

Subconjunctival Hemorrhage is self limited to how long?

2 days

How does this abnormality clinically present? - 2
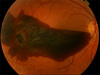
- [suddennonpainful uL vision ∆ (hazy|red hue|COMPLETE LOSS)]
- Floaters also seen with [Torn Retinal Detachment]
dx = Vitreous Hemorrhage

When can you mandate parents against their will to accept treatment for a [non emergent ailment] for their child?
PARENTS CAN NOT REFUSE TX for any F.A.T. conditions!!
🔎F.A.T.. = FATAL Although Treatable
PARENTS CAN NOT REFUSE ANY TX THAT IS LIFE SAVING 911 | non911
_________________
If pt [nonrmergent ailment] is a [treatable & FATAL condition (i.e. Cancer)] – PARENTS CAN NOT REFUSE THAT LIFE SAVING TX → M.D. can obtain a court order to give tx
________________
PARENTS ARE NOT ALLOWED TO REFUSE TX for treatable LIFE SAVING TREATMENT FOR THEIR CHILD (EVEN IF BASIS IS RELIGIOUS)
Describe ophthalmoscopy findings for Diabetic Retinopathy-3
- microaneurysms = simple type
- retinal edema = simple type
- newly formed vessels if malignant type
low tone hearing loss = [⬜ sensorineural | conductive] hearing loss
conductive

Glaucoma

📖
cp for Acute Closed angle Glaucoma - 3
- PAINFUL Red eye uL
- Fixed Dilated pupil
- Cloudy Cornea
_________________
“Closed angle needs OPMAT .. STAT!”

Prognosis for [Acute Closed angle Glaucoma]

Permanent Vision Loss within 2-5 hrs of onset!

_________________
“Closed angle needs OPMAT .. STAT!”
Identify finding

[(Zoster Ophthalmicus)Dendriform Corneal Ulcer]
________________
dx = Zoster Ophthalmicus





[Closed angle Glaucoma] accounts for ⬜% of cases, presents [⬜ gradually | abruptly] , and is a medical Emergency!
What is the etx for [Closed angle Glaucoma]? -4
_________________
AKA: [Acute Glaucoma or angle-closure Glaucoma]
10% ; abruptly
⭐{[ aLi: CL❌SES 1st](idiopathic vs iris hypoxia) ➜ [ aTic: CL❌SES 2nd] = [TMAD❌]}⭐
_________________
1) centralIris and lens stick together= aLi closes 1st
2) → rapid ⇪ IOP pushes peripheralIris against Cornea
3) → CLOSING off aTic 2nd → [RAPID ⇪ ⇪ ⇪ IOP]
4) [RAPID ⇪ ⇪ ⇪ IOP] → [RAPID optic n damage] → Blindnesswithin 2-5h of onset⚠️!
_________________
“Closed angle needs OPMAT .. STAT!”
🟢=Open / ❌=closed

🔎aLi = angle between Lens and Iris
_________________
🔎[aTic : angle at iris ⼀{TMAD} ⼀cornea] | [TMAD: Trabecular Meshwork AqueousHumor Drain]
[Open angle Glaucoma] accounts for ⬜% of cases, and presents [⬜ gradually | abruptly]
What is the etx for [Open angle Glaucoma]? -3
65% ; gradually
* * *
⭐[ **aLi**: 🟢]. [ **aTic**: 🟢]. [**TMAD**: ❌].⭐
\_\_\_\_\_\_\_\_\_\_\_\_\_\_\_\_\_
1. idiopathic vs [TMAD❌<sub>(Trabecular Meshwork Aqueous<sub>Humor</sub> Drain ❌bstruction)</sub>]
2. → [*gradually slow* ⇪ IOP] → [*gradual slow* loss of <sup>(peripheral 1st)</sup>sight over years]
3. aTic not affected = remains open
\_\_\_\_\_\_\_\_\_\_\_\_\_\_\_\_\_
| 🟢=Open / ❌=closed
## Footnote
*🔎**aLi** = **a**ngle <sub>between</sub> **L**ens and **I**ris*
\_\_\_\_\_\_\_\_\_\_\_\_\_\_\_\_\_
🔎[**aTic** : **a**ngle <sub>at </sub>**i**ris ⼀{**_T_**_MAD}_ ⼀**c**ornea] | [TMAD: Trabecular Meshwork Aqueous<sub>Humor</sub> Drain]
definition
Astigmatism
abnormally curved cornea that causes different refractive power at different axes
definition
PresByopia
age-related ⬇︎lens elasticity → [⬇︎accommodation (near-vision)]
👣often needs reading glasses
risk factors (8)
cataracts

- age
- smoking
- EtOH
- CTS
- [DM (sorbitol)]
- trauma
- excessive sunlight
- infection
- galactosemia / galactokinase deficiency

Latanoprost
MOA
_________________
Indication
[PGF2αProstaglandin analog ] = ⇪ outflow of aq humor
_________________
Glaucoma
📝side effect = darkens /causes iris “browning”
Physiological action of GH in children (5)
Linear Growth of
- long bones(primary determinant of adolescent growth spurt)
- cartilage
- muscle
- organ systems
+ [Blood Glucose promoter]
Physiological Action of GH in Adults (3)
- Catabolic for Fat
- Anabolic for Muscle & Bone
- Blood Glucose Promoter (INC Blood Glucose)

Effects of GH are mostly mediated by _____, which is released from the ____ in response to ___
Effects of GH are mostly mediated by IGF1, which is released from the liver in response to GH
[GHRH → GH —> IGF1]
In addition to Musculoskeletal changes, what other changes occur in Adults with GH deficiency (3)
- Hyperlipidemia
- Cardiac Muscle Atrophy
- [Fatigue / Depression / Malaise]

Adult onset GH deficiency is typically due to what?
Pituitary problem

Drugs for GH deficiency (4)
[SERMorelinGHRH]
_________________
SOMAtrem
SOMAtropin
_________________
mecaSERMin
Name a Synthetic GHRH
sermoRELin
Name 2 [Recombinant HumanGH]
- Somatropin
- Somatrem
What is Mecasermin?
Recombinant IGF1
Somatropin Indication (5)
SPAWN
- Pediatric growth failure (associated w/GH/chronic Renal Failure/Prader Willi/Turner)
- No idea: Idiopathic short stature (>2.25 SD below mean height)
- Adult GH deficiency
- Wasting in AIDS pts
- Short Bowel Syndrome in pts receiving nutritional support (it INC SA for digestion)
Structure of Somatropin
identical to native hGH
(Somatropin = Synthetic GH structurally identical to native hGH)
Mecasermin Indication
Pediatric IGF1 deficiency from [Laron GH receptor Dwarfism] vs. [Ab against GH]

Octreotide [Drug Class and MOA]
Somatostatin Analogue (45x more potent and long lasting) –> blocks GH secretion

Octreotide Indications (4)
- Pitutiary microadenoma
- Carcinoid Crisis (flushing/diarrhea/Cyanosis)
- Secretory Diarrhea 2° to VIP tumors
- Acute GI Bleeding
Name the Gonadotropins (4) and what their MOA is
Replaces FSH and LH
- Menotrophins (FSH and LH)
- hCG
- Urofollitropin (FSH from menopausal women urine)
- Follitropin
Gonadotropins Indication (3)
- Ovulation in [women with hypOgonadotropic hypOgonadism] vs. IVF
- PCOS/Obesity
- Infertility in [Men with hypogonadotropic hypOgonadism]
How does GnRH🟢 or [ short half lifeGnRH analog] affect gonadal axis?
Stimulates Gonadotroph cells to make/secrete LH & FSH

[ LONG half lifeGnRH analog] MOA
Desensitizes GnRH receptors and inhibits FSH and LH release
Biphasic Effect of [GnRH analogs]
GnRH➿
1st: short1/2 life = FLARE effect = Transient (7-10 days) FLARE (INC) in gonadal hormone levels from agonist effect
2nd: LONG1/2 life-lasting suppresion of Gonadotropins and gonadal hormones from inhibition
{GnRH➿ = GnRH analogs}
Goserelin Indication (8)
[specific = aef ]
1. androgen dependent Prostate CA] adjunct
2. endometriosis
3. fibroids_Uterine
________+_________
[ALL = BOPIA]
4. Breast CA
5. Ovarian CA
6. PCOS
7. Infertility
8. Amenorrhea
{GnRH➿ = GnRH analogs}

{[Goserelin GnRH➿] indication} = {[specific[a|e|f ]] + [GENERALBOPIA]}
Leuprolide Indication (10)
aefcr
1. [androgen dependent Prostate CA] adjunct
2. endometriosis
3. fibroids_uterine
4. central precocious puberty
5. [reproductive IVF(keeps LH surge low → multi-oocyte maturation) ]
________+_________
[ALL = BOPIA]
4. Breast CA
5. Ovarian CA
6. PCOS
7. Infertility
8. Amenorrhea
{GnRH➿ = GnRH analogs}

{[Leuprolide GnRH🟢] indication} = {[specific[a|e|f |c|r ]] + [GENERALBOPIA]}
List the 3 [GnRH🟥]
“Don’t Block me from getting my Rolex”
- Ganirelix
- Cetrorelix
- Abarelix
These are Dose-Dependent

How is administration between [GnRH synthetic analogs] and [GnRH R Blockers] different (2)
- [GnRH R Blockers] produce immediate Blocking effect = Duration of Admin is shorter during IVF
- [GnRH R Blockers] don’t produce Flare Effect
Drugs given during [Follicular Proliferative Phase] during IVF (3)
- Gonadotropin injection is given 3 days after menses to immediately start developing Follicles.
- {[_LONG_1/2GnRH analogs] or [GnRH R Blockers]} are given to prevent premature LH surge
Physiologic Actions of Prolactin (4)
- Mammogenesis
- Milk production
- Milk secretion
- [Inhibits GnRH secretion → Suppresses Ovulation]

Hyperprolactinemia Tx (3)
and why
- Bromocriptine
- Cabergoline
- Pergolide
These are [D2-dopamine🟢] (Dopamine blocks [Lactotrope_PROLACTIN] secretion)

Bromocriptine Indication (5)
- Pituitary Prolactinoma
- PMS
- Acromegaly (Use High Doses and only if tumor secretes both Prolactin & GH)
- Parkinson’s Dz
- Type2DM



