1 ⼀NEUROLOGY I Flashcards
(265 cards)
identify






A: MIOS seen in Younger pts indicates ⬜
B: MIOS seen in OLDER pts indicates ⬜
C: What is the purpose of the MLF
[MIOS-MLF Internuclear Ophthalmoplegia Syndrome]
1) Younger pts= Multiple Sclerosis
2) Older pts= [Pontine a. lacunar stroke]
________________
MLF coordinates CN3 with CN6
________________
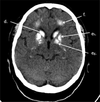
Image: Left MIOS

CP for [MIOS-MLF Internuclear Ophthalmoplegia Syndrome] (3)
[MIOS-MLF Internuclear Ophthalmoplegia Syndrome]
*[Impaired ADDuction of affected eye]
+
[Normal ADDuction of affected eye during [near reflex convergence]
+
*[Nystagmus of UNaffected eye when attempting to ABduct]👣
Image: L MIOS

👣{(2/2 [Abducens CN6] overfiring in an attempt to stimulate [Oculomotor CN3]}
1st line tx for Heat Stroke is ⬜, which should be used to ⬇︎core body temperature by ⬜C/min .
Describe it
________________
List 3 adjunct Heat Stroke therapies
[augmentation of EVAPORATIVE COOLING] ; [0.2C/min]
(naked pt is sprayed with tepid (warm) water mist or pt is covered in wet sheet – while large fans circulate air ➜ ⇪ evaporative heat loss)
________________
ice water lavage / ice packs / cold IVF
3 main causes of pinpoint pupils

- Opiate OD
- Pontine lesion destroying sympathetic fibers
- Cholinergic eyedrops for Glaucoma

3 Main causes of Spinal Cord Compression

- DJD Disc Herniation (Smoking risk factor)
- [Epidural Staph a. Abscess (think IV drug user vs DM)]
- Tumor (Prostate/Renal/Lung/Breast/Multiple Myeloma mets)

Dx = MRI, Positive Straight Leg, Classic S/S
DJD=Degenerative Joint Disease
6 major causes of Syncope
MVC BSD
- ⬇︎ Cardiac Output (Valvular Dz/HOCM/Pulm HTN/PE/Tamponade/myxoma/aFib)
- Bradyarrhythmia (SA Node dysfunction/AV Block)
- [VANS - Vasovagal Autonomic Neurocardiogenic Syncope]
- Dehydration
- Stroke
- Metabolic (⬇︎Glucose vs ⬇︎Na+)
OBTAIN ECHOS ON ANY PT WITH SUSPICIOUS SYNCOPE!
A patient taking metoclopramide develops involuntary next flexion known as ⬜
Tx? (2)
[Torticollis Dystonia] ; [Benztropine IV 🆚 Diphenhydramine IV]
A pt complains of inabilty to recognize previously known faces
What is this called? ; Where is the lesion?
[ProsoPagnosia visual agnosia] ; BL Temporo-Occipital

a. Tx for PostFall syndrome (2)
_________________
b. What is PostFall syndrome?
a.
-URGENT PHYSICAL THERAPY(to ⇪ mobility which ➜ ⇪ functionality)
-URGENT BEHAVIORAL THERAPY(to improve thinking/behavior about falls)
_________________
b. maladaptive fear of falling after a fall that ➜ restricted mobility ➜ functional decline in the elderly
Describe the 4 main sx for [Brown Sequard Syndrome]
1.[DCP: Ipsilateral 2TVP loss]
2.[LateralCST: Ipsilateral [UMN (Weak MESH)]
3.[STT: Contralateral Pain/Temp loss 2 LEVELS BELOW ORIGINAL LESION]
4.[+/- Horner’s MAP](if hemisection is above T1 since this → oculosympathetic pathway damage)
|💡 Brown Sequard = SpinalHemisection

🖊2TVP-2point/Touch/Vibration/[Position Proprioreception]
Causes of [Brown Sequard Syndrome] - 3
- [(Extramedullary Tumor]
- Trauma
- [DJD Disc Hernation (Smoking risk factor)]

A: Describe Opsoclonus-Myoclonus Syndrome
B: What Childhood tumor is it associated with?
A: [Non-Rhythmic Conjugate Eye mvmnts] with myoclonus= “Dancing Eyes and Feet”
B: Neuroblastoma (onset 2 y/o)
Arises from Neural crest

PCiiH [Pseudotumor Cerebri Idiopathic Intracranial HTN] Dx - 3
1st: [CT to r/o space occupying lesion]
➜ 2nd: [Lumbar Puncture with opening pressure >250 mmH20 (from ⬇︎Arachnoid villi CSF absorption)]
3rd: [MRI +/- MRV revealing BL tortuous Optic N]
* _________________*
* This HA will make you go Blind!*

⊕Papilledema is a ctx to Lumbar puncture
When is ⊕Papilledema not a ctx to Lumbar puncture? Explain

[PCiiH (Pseudotumor Cerebri Idiopathic Intracranial HTN)];
As long as there are no signs of obstructive/noncommunicating hydrocephalus or mass, then it is ok
LP with CSF opening pressure > 250 mmH20 = PCIIH

[Pseudotumor Cerebri Idiopathic Intracranial HTN] Clinical Presentation - 4
PCiiH girls like to VAPE
- [Vision ∆ +/- papilledema]
- [Abducens CN6 palsy]
- Pulsatile Tinnitus
- [Eye-blinding HA (worst at sleeping times) & with head position ∆]
* This HA will make you go Blind!*

What is Wallerian Degeneration?
Degeneration of Axons after trauma, but in the setting of [preserved perineurium and epineurium] which later acts as scaffolding to allow axonal sprouting and regeneration within the PNS

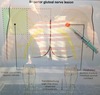
Describe the Lacunar Syndrome CP

👀
lenticulostriate vessels perfuse [BTiC]
1A: {[Basal GangliaSubthalamic nc] → [CTLHemiballismus & involuntary writhing]}
1B: {[ThalamuSVPL]→[CTL Sensory Stroke]}
1C: {[internal CapsulePOST limb/Corona Radiata]-→ [CTLMotor stroke(ataxia|clumsy hand-dysarthria)]}

👀Lacunar Stroke= [Thrombotic HTN Arteriolosclerosis & Thrombotic microatheromas] of lenticulostriate vessels (BTiC) –> [cystic infarcts < 15 mm] –> Lacunar Syndrome
VPL=VentroPosteroLateral nc
List the n. roots associated with Common Peroneal n.
L4-S2
foot is dropPED (Peroneal Everts & Dorsiflexes)
- Commonly caused by L5 Radiculopathy*
- Dx: Knee MRI vs EMG*

List the n. roots associated with Tibial n.
L4-S3 (Three)
can’t walk on TIPtoes (Tibial Inverts & Plantarflexes)
Commonly caused by L5 Radiculopathy

What are the functions of the Common Peroneal n. -2
L4-S2
foot is dropPED (Peroneal Everts & Dorsiflexes)
_________________
🔬 Commonly caused by L5 Radiculopathy
🩺 Knee MRI vs EMG

What are the functions of the Tibial n. (2)
L4-S3 (Three)
can’t walk on TIPtoes (Tibial Inverts & Plantarflexes)
Commonly caused by L5 Radiculopathy