Upper GI Tract Flashcards
(88 cards)
Where does the oesophagus start and end ?
Start-C5
End-T10
Name the 2 Oesophageal sphincters ?
Lower Oesophageal Sphincter-LOS
Upper Oesophageal Sphincter-UOS
What are the 4 anatomical contributions to the Lower Oesophageal Sphincter ?
LOS is more of a physiological sphincter, with a number of contributing anatomical contributions;
1- Distal 3-4cm of oesophagus in abdomen.
2-Diaphragm surrounds the LOS.
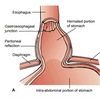
3- Intact Phrenoesophageal ligament.
4-Angle of His.
How does the distal 3-4 cm of the oesophagus being in the abdomen contribute to LOS function?
If you get an increase in intra-abdominal pressure you get an increase in LOS pressure as well.
How does the diaphragm surrounding the LOS contribute to its function ?
The left and right crux act like scissors when the diaphragm contracts, they contract against the sphincter.
What is the role of the phrenoesophageal ligament in the function of the LOS ?
You need to have an intact phrenoesophageal ligament, this is an extension of the inferior diaphragmatic fascia, with two limbs one that goes superiorly and attaches to the lower part of the oesophagus the other goes inferiorly and attaches to the cardia of the stomach, this allows individual movement of the diaphragm during respiration and the oesophagus when you swallow.
What is the structure known as ?
Angle of His, an acute angle between the abdominal oesophagus and the fundus of the stomach, at the oesophago-gastric junction. This prevents reflux disease by the fundus expanding and combressing the oesophagus when someone has had a large meal.
How many stages are there in normal swallowing?
4
What is stage 0 of normal swallowing ?
Oral phase - chewing and saliva prepares bolus, both the oesophageal sphincters are constricted
What is stage 1 of normal swallowing ?
Pharyngeal phase - pharyngeal musculature guides food bolus towards oesophagus, the UOS opens reflexly. The LOS is opened by vasovagal reflex (receptive relaxation reflex).
What is stage 2 of normal swallowing ?
Upper Oesophageal phase - the UOS closes and superior circular muscle rings contract whilst inferior rings dilate, with sequential contractions of longitudinal muscle.
What is stage 3 of normal swallowing ?
Lower oesophageal phase - LOS closes as food passes through.
How do you measure normal swallowing ?
Manometry, this is where a tube is passed throught he nose down the oesophagus that measures pressure of contractions.
What are normal peristaltic waves ?
40mmHg
What is the normal pressure of the LOS ?
20mmHg
What happens to the pressure at the LOS during receptive relaxation ?
Decreases to <5mmHg this is mediated by inhibitory noncholinergic nonadrenergic NCNC neurons of myenteric plexus.
What are 3 causes of functional oesophageal disorders ?
- Absence of a stricture.
- Abnormal oesophageal contraction.
- Failure of protective mechanisms for reflux.
What is an example of Abnormal oesophageal contraction ?
- Hypermotility
- Hypomotility
- Disordered Coordination
What is an example of failure of the protective mechanisms for reflux ?
GastroOesophageal Reflux disease GORD
What term is used for difficulty in swallowing ?
Dysphagia, it is important to localise the dysphagia as well as what type ( to solids or liquids), if it is getting better or worse.
What is the term for pain on swallowing?
Odynophagia
What term describes the return of oesophageal contents from above an obstruction?
Regurgitation, is it functional or mechanical.
What term describes passive return of gastroduodenal contents into the mouth ?
Reflux
Give an example of hypermotility ?
Achalasia