Soft Tissue Infection 01-20, 24 Flashcards
A 41-year-old woman who is a dentist comes to the office because she has had intense burning and pruritus of the dominant index finger for the past 6 days. The patient reports a small vesicular rash on the finger that has since progressed to form a small blister. She has had intermittent fever and malaise. Which of the following is the most appropriate management?
A) Incision and drainage of the bullae
B) Intravenous administration of cefazolin
C) Oral administration of acyclovir
D) Topical application of silver sulfadiazine
E) Observation only
The correct response is Option E.
The patient has a history and physical findings consistent with herpetic whitlow. This is a viral infection caused by herpes simplex virus and is more common in medical and dental personnel. Tzank smear or antibody titers can confirm a diagnosis but are unnecessary in the management of this patient. Treatment is primarily nonoperative and involves observation, as the course of the illness is self limiting with resolution in 1 to 3 weeks. Intravenous antibiotics would not treat this viral infection. Incision and drainage is unnecessary and may lead to a bacterial superinfection or systemic dissemination of herpes simplex virus. Acyclovir or valacyclovir may shorten the duration of symptoms, but must be started within 2 to 3 days of onset. Topical application of an antimicrobial would provide no benefit in this case. Surgical drainage of the bullae should not be performed because it may increase the risk of spreading the herpes virus and may also lead to bacterial superinfection.
A 23-year-old man presents with painful, red swelling over the dorsum of the right middle finger metacarpophalangeal (MCP) joint 3 days after he punched someone in the face during a bar fight. The patient reports decreasing range of motion of the hand and inability to grasp objects. He was previously seen in the emergency department the night of the injury and x-ray studies were negative for fracture or foreign body. Which of the following is the most likely causative organism?
A) Clostridium perfringens
B) Eikenella corrodens
C) Pasteurella multocida
D) Pseudomonas aeruginosa
E) Staphylococcus epidermidis
The correct response is Option B.
Eikenella corrodens is an anaerobic organism present in human oral flora and has been associated with human bite wounds. Group A Streptococcus is also a common pathogen in a fight bite injury like the one this patient has.
This patient has most likely sustained a “fight bite,” which results from tooth penetration of the metacarpophalangeal (MCP) joint after striking someone in the mouth with a clenched fist. These injuries can often be underappreciated, as the underlying defect in the extensor hood and joint capsule may not be seen on examination when the fingers are extended during examination in an emergency department. The joint can become contaminated with oral flora. Penetrating injury with high bacterial load can result in a septic joint and lead to destruction of cartilage and osteomyelitis. Recreation of the flexed fist position may help in lining up the structures and assist in identification of the injury. Treatment is aggressive antibiotic therapy and surgical exploration with irrigation and debridement of the joint to remove debris.
Clostridium perfringens is a gram-negative rod associated with gas gangrene, which results in subcutaneous crepitus and can be rapidly progressive. Pasteurella multocida is a gram-negative anaerobic bacterium most commonly associated with cat bite infections. Pseudomonas aeruginosa is a gram-negative rod that can be associated with diabetic wound infections. And Staphylococcus epidermidis is a gram-positive cocci present on the skin. It has been associated with implant infections. None of these pathogens are as likely to be present in a fight bite as Eikenella corrodens.
A 30-year-old woman with type 1 diabetes mellitus presents with fever, nasal obstruction and drainage, and swelling of the left eye. Nasal endoscopy shows blackish secretions and necrosis of the inferior turbinate and adjacent nasal mucosal tissues. Which of the following is the most likely diagnosis?
A) Candidiasis
B) Epiglottitis
C) Mastoiditis
D) Mucormycosis
E) Necrotizing fasciitis
The correct response is Option D.
Infections of the head and neck should not be ignored, as many of them can evolve into life-threatening emergencies, some of them very quickly. Rhinocerebral mucormycosis is a rare opportunistic infection of the nasal cavity and sinuses that can rapidly spread to the orbits and brain by erosion of bone and invasion of blood vessels. Mucormycosis is caused by saprophytic fungi, and usually affects individuals with diabetes mellitus and those who are immunocompromised. The mainstay of treatment includes reversal of immunosuppression when possible, systemic antifungals, and surgical debridement. Timely treatment is critical and usually dependent on rapid diagnosis by history and physical examination, imaging, and intraoperative biopsy with frozen section pathology, since waiting for cultures causes unnecessary delay in severe cases. Mucormycosis can also present in the oral cavity, lungs, ears, and other sites less commonly.
Epiglottitis is an infection of the supraglottic region causing inflammation and swelling of the epiglottis. It is most commonly caused by Haemophilus influenzae type b and has become rare since the introduction of the vaccine against this bacteria. Swelling of the epiglottis can cause airway obstruction. Mastoiditis is infection of the mastoid air cells, which are in continuity with the middle ear. The mastoid process behind the ear is also usually swollen and tender. Infections usually start from untreated otitis media. Risks include spreading to the surrounding structures, including the brain. Necrotizing fasciitis is a soft tissue infection that rapidly spreads through the subcutaneous fat and fascia with necrosis of the overlying skin. In the head and neck, the infection is usually spread from infection of the teeth or pharynx. The plaque-like infection of candidiaisis does not present in this fashion.
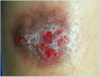
An otherwise healthy 23-year-old man is brought to the emergency department after a motor vehicle-pedestrian collision causing compartment syndrome, myonecrosis, and need for radical resection of devitalized tissue of the right thigh. He is hemodynamically stable. A photograph taken two days after his first debridement is shown. Which of the following is the most appropriate next step in management?
A) Bilaminate neodermal reconstruction
B) Free contralateral anterolateral thigh flap
C) Negative pressure wound therapy
D) Skin grafting
E) Surgical debridement

The correct response is Option E.
Given the obvious devitalized tissue in the associated photograph, the most appropriate next step would be further debridement. This is an often overlooked, but still critical, cornerstone to reconstruction, because without it, complication rates from infection are significantly increased.
Debridement involves the removal of nonviable or contaminated tissue that impedes normal tissue growth. It renews the wound and surrounding tissue to promote normal healing by removing infection, biofilm, and senescent cells.
Different debridement options are available, including mechanical, biologic, technical, and surgical methods. In this acute scenario with an otherwise healthy patient and a large amount of devitalized tissue, surgical debridement is the most appropriate choice.
All other modalities/choices are not appropriate until the wound bed is stabilized. Negative pressure wound therapy may be used in conjunction with debridement, but is not a replacement for it.
A 28-year-old woman comes to the office for evaluation of excessive sweating and odor. She reports that she has a long history of heavy perspiration, mainly from the axillary and groin area. Which of the following glands contributes to her excessive and malodorous sweating?
A) Apocrine
B) Eccrine
C) Holocrine
D) Merocrine
E) Sebaceous
The correct response is Option A.
Apocrine glands are associated with sweat production and when mixed with bacteria produce body odor, which can be malodorous. There are two types of sweat glands, eccrine and apocrine. Eccrine glands are located throughout the body and secrete primarily water and salt. Apocrine glands are located in hair-bearing areas such as the axilla and groin and secrete watery fluid that is higher in protein.
There are three types of exocrine secretion. Merocrine glands secrete via exocytosis and no part of the glands is damaged or lost. Eccrine glands are a type of merocrine gland. Apocrine glands secrete via membrane budding and loss of cytoplasm. The mammary glands are a type of apocrine gland. Finally, holocrine glands secrete via membrane rupture, which destroys the cell. Examples include sebaceous glands, which contain remnants of dead cells, as well as meibomian glands of the eyelids.
Hyperhidrosis describes excessive sweating through the eccrine glands where there is an increase in number and size of these glands. Osmidrosis, or bromhidrosis, involves excess secretion of the apocrine glands combined with bacterial proliferation with corynebacterium. Enzymatic breakdown of the glandular secretions results in the malodor.
A 21-year-old man comes to the emergency department 10 days after undergoing a septorhinoplasty, with new-onset fever, malaise, throat pain and a painful skin rash. He recently completed a course of amoxicillin and clavulanate potassium (Augmentin). Temperature is 39.1°C (102.4°F), blood pressure is 75/40 mmHg, and heart rate is 140 bpm. Physical examination shows multiple cutaneous blisters involving the face and entire trunk (45% total body surface area [TBSA]). Intraoral examination shows mucosal erythema and erosions. Nasal examination shows nasal septal splints that were placed at the time of surgery. The patient is admitted to the hospital. Biopsy of the skin rash shows full-thickness epidermal necrosis with dermal edema and sparse dermal infiltrates. Which of the following is the most likely diagnosis?
A) Acute generalized exanthematous pustulosis
B) Drug reaction with eosinophilia and systemic symptoms
C) Stevens-Johnson syndrome
D) Toxic epidermal necrolysis
E) Toxic shock syndrome
The correct response is Option D.
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are in the spectrum of the same disease process, characterized by a severe drug-induced immune reaction. The drug or its metabolite acts as a hapten and provides antigenic stimulation for a T-cell–mediated delayed hypersensitivity reaction. The list of offending medications is extensive and includes antibiotics, anticonvulsants and NSAIDs. Onset is within the first 8 weeks of starting the medication, and is characterized by fever, mucositis and a painful generalized vesiculobullous rash. Histology of skin specimens reveals keratinocyte apoptosis, full-thickness necrosis of the epidermis, and minimal dermal inflammation. Mucosal inflammation can involve any mucosal surface. Cutaneous involvement consists of blisters and erosions, with skin separation. Application of shear forces on the skin results in separation of the epidermis (Nikolsky sign). Skin separation of less than 10% of total body surface area is classified as SJS, greater than 30% of total body surface area as TEN, and 10 to 30% of total body surface area as SJS-TEN overlap. Multisystem organ dysfunction can occur. Treatment is supportive, with the best outcomes in patients treated early in a burn center. Intravenous corticosteroids are usually given, although their use is controversial. Mortality is 1 to 5% in SJS and 25 to 40% in TEN. Survivors are often left with skin scarring, mucosal strictures, and ocular complications.
Toxic shock syndrome (TSS) is caused by toxin-producing strains of Staphylococcus aureus and Streptococcus pyogenes. The toxin acts as a super antigen and causes widespread immune stimulation. Staphylococcal Toxic Shock Syndrome can occur after surgical or traumatic skin break or from colonization of a foreign body. Onset is within 48 hours of surgery and consists of influenza-like symptoms, fevers, and shock. Multisystem organ failure can occur. Skin desquamation usually occurs 2 to 3 weeks later. Treatment consists of source control, antibiotic therapy, and in some cases, immunoglobulins.
Acute generalized exanthematous pustulosis (AGEP) is a T-cell–mediated cutaneous drug reaction. Onset is usually within 48 hours and consists of fever, leukocytosis, and a rash consisting of many small sterile non-follicular pustules distributed predominantly on the trunk and intertriginous areas. Mucous membrane involvement is uncommon and occurs mostly in the lips and buccal mucosa. Internal organ involvement occurs in a minority of cases but can lead to multisystem organ dysfunction. Histology shows intracorneal, sub-corneal, and intraepidermal pustules and a dermal neutrophilic and eosinophilic infiltrate. Treatment is discontinuation of the offending drug, after which the condition quickly resolves. Prognosis is excellent.
Drug reaction with eosinophilia and systemic symptoms (DRESS) is a severe drug reaction of unclear pathogenesis that is characterized by fever, hematological abnormalities (leukocytosis, eosinophilia), and internal organ dysfunction. Onset is typically 2 to 8 weeks after drug exposure. Antiepileptics are most commonly implicated, although a variety of drugs, including antibiotics, can be the causative agent. Cutaneous involvement consists of a morbilliform rash. Mucosal involvement is frequent. Facial edema can be severe. Blood leukocytes are markedly elevated, with 30% of cases having eosinophilia. Multisystem organ dysfunction can occur. Histopathology reveals a perivascular lymphocytic infiltrate in the papillary dermis and dermal edema with extravasated erythrocytes and eosinophils. Treatment consists of cessation of the offending drug, systemic glucocorticoids and supportive care.
A 27-year-old man comes to the emergency department for evaluation after being involved in an altercation earlier in the evening during which he sustained multiple injuries to his right hand. Physical examination shows a deep laceration over his right index and long finger metacarpophalangeal (MCP) joints. There is no evidence of tendon or neurovascular injury. The wound is debrided at bedside, packed with moistened gauze, and placed in a sterile dressing. Prior to discharge, the patient should be provided with prophylactic antibiotic coverage for which of the following microorganisms?
A) Eikenella
B) Flavobacterium
C) Mycobacterium
D) Pasteurella
E) Vibrio
The correct response is Option A.
It is important to recognize dorsal hand lacerations as a possible site for serious infection, especially in the context of altercations where a “fight bite” might have occurred. In some cases, patients may be apprehensive to admit to the source of their injury, and in these cases, physicians should err on the side of caution and provide antibiotic prophylaxis. The primary bacteria isolated from human bite wounds is Eikenella. Pasteurella is commonly found in wounds resulting from the bites of dogs, cats, or farm animals. Flavobacterium is associated with bites from freshwater fish. Mycobacterium can be seen in bites from bears and ferrets. Vibrio is associated with shark bite wounds and other marine injuries.
A 40-year-old man presents to the emergency department because of the infection shown. Medical history includes type 2 diabetes mellitus, hypertension, kidney transplantation 5 years ago, and a 10 pack-year history of smoking (former smoker). Temperature is 39.7°C (103.5°F) and blood pressure is 80/45 mmHg, white blood cell count is 25,000/μL. He is transferred to the surgical intensive care unit for fluid resuscitation and intravenous antibiotics prior to operative debridement in six hours. Which of the following is the strongest risk factor for mortality in this patient?
A) Age
B) Delay in operative debridement
C) History of kidney transplantation
D) History of smoking
E) Type 2 diabetes mellitus

The correct response is Option B.
Necrotizing fasciitis is a rapidly progressive soft-tissue infection. Patients usually present with systemic sepsis, fever, high leukocytosis (higher than 25,000), skin findings of edema with blue discoloration, weeping blisters and cellulitis. The more severe cases can present with multisystem organ failure and altered mental status. Polymicrobial infections are most common. Streptococcal species are isolated in more than 60% of polymicrobial infections. Other organisms identified include Staphylococcus aureus, Escherichia coli, Pseudomonas, Enterobacter, Klebsiella, Proteus, Bacteroides, Clostridium, and Peptostreptococcus.
Multiple studies have reported a mortality rate of approximately 20% from necrotizing fasciitis. Mortality is directly proportional to time of intervention. Delayed surgical debridement has been shown to significantly increase the mortality risk. After diagnostic delay, the most common pitfall in treatment is inadequacy and delay in surgical debridement.
Type 2 diabetes mellitus is incorrect. Comorbid conditions such as diabetes, vascular disease and venous insufficiency are very common in these patients. Diabetes specifically is associated with higher morbidity and mortality. Studies have shown that patients with diabetes have a higher chance of a negative outcome compared to patients without diabetes. However, it has not been shown to be the most severe risk factor associated with mortality.
Smoking is incorrect. Smoking is a risk factor for delayed healing, but there are no studies that show smoking alone to be a risk factor in the progression of necrotizing fasciitis.
After delay of operative debridement, immunosuppression is the second most significant risk factor for mortality. Patients with solid organ transplantation or undergoing treatment for hematologic malignancies are most at risk. Age has been reported as another risk factor of mortality in patients with necrotizing fasciitis. Studies have shown that extremes of age, younger than 1 year or older than 60 years, were associated with mortality, but age is not the strongest risk factor among the others reported.
A 59-year-old man with type 2 diabetes mellitus comes to the office because he has had swelling, pain, and decreased function of the right small finger after he injured it slightly 2 weeks ago. The patient reports similar symptoms of the right thumb, although it sustained no inciting injury. Examination of both digits shows signs and symptoms of pyogenic flexor tenosynovitis. In addition to washing out the respective tendon sheaths, exploration of which of the following additional sites is necessary?
A) First web space
B) Flexor carpi radialis tendon sheath
C) Hypothenar compartment
D) Ring finger flexor tendon sheath
E) Space of Parona
The correct response is Option E.
Infectious flexor tenosynovitis can spread from the tendon sheath of the fifth digit to the flexor tendon sheath of the thumb by way of the space of Parona: the potential space in the volar wrist, deep to the flexor tendons but superficial to the pronator quadratus muscle. In this area, the proximal extent of the tendon sheaths of both the small finger and the thumb are in close proximity. This has been termed the “horseshoe abscess” of the upper extremity.
Which of the following time frames for onset most accurately reflects the CDC’s definition of surgical site infection?
A) Within 3 days of surgery or within 30 days of prosthetic implant placement
B) Within 7 days of surgery or within 3 months of prosthetic implant placement
C) Within 14 days of surgery or within 6 months of prosthetic implant placement
D) Within 21 days of surgery or within 9 months of prosthetic implant placement
E) Within 30 days of surgery or within 1 year of prosthetic implant placement
The correct response is Option E.
The CDC defines a surgical site infection as an infection that occurs at the incision site or within the organ or space operated on within 30 days after surgery or within 1 year if a prosthetic implant is placed. Infection requires at least one of the following:
Purulent drainage from the surgical site
Organisms isolated from an aseptically obtained culture of fluid or tissue at the surgical site
Spontaneous dehiscence of a deep incision or deliberate opening of the incision by a surgeon when the patient has at least one of the following signs or symptoms: fever (greater than 100.4°F [38.0°C]), localized pain or tenderness, localized swelling, redness, or heat, unless site is culture-negative
An abscess or other evidence of infection involving the incision or operative site that is found on direct examination, during reoperation, or by histopathologic or radiologic examination
Diagnosis of a surgical site infection by a surgeon or attending physician
A 30-year-old Florida fisherman comes to the emergency department 24 hours after cutting his palm with a fish-scaling knife. Blood pressure is 90/50 mmHg and heart rate is 120 bpm. Physical examination shows severe swelling of the hand, hemorrhagic bullae of the hand, and erythema to the mid forearm. X-ray study shows no gas within the soft tissues. A Gram stain of drainage from a bulla reveals gram-negative bacilli. Which of the following infectious agents is the most likely cause of the patient’s symptoms?
A) Clostridium perfringens
B) Mycobacterium marinum
C) Pseudomonas aeruginosa
D) Staphylococcus aureus
E) Vibrio vulnificus
The correct response is Option E.
The patient described has necrotizing fasciitis and sepsis. Vibrio vulnificus is a gram-negative bacillus, a cause of necrotizing fasciitis, and is commonly associated with warm saltwater environments (Florida). It also tends to present with hemorrhagic bullae. Staphylococcus aureus is a gram-positive coccus, is not associated with watery environments, and is more commonly associated with pustules rather than hemorrhagic bullae. Clostridium perfringens is a gas-forming, gram-positive bacillus, and is associated with marine sediment. Pseudomonas aeruginosa, also a gram-negative bacillus, although associated with moist environments, is more typically associated with less aggressive soft-tissue infections. Mycobacterium marinum is also associated with watery environments, but tends to affect aquarium owners with an indolent granulomatous process.
A 53-year-old woman undergoes bilateral mastectomy and autologous breast reconstruction. Four days postoperatively, the patient reports moderate abdominal discomfort and multiple episodes of diarrhea. Vital signs are within normal range. Physical examination shows a mildly distended abdomen. Stool sample is positive for Clostridium difficile toxin. Treatment with which of the following drugs is most appropriate first-line treatment in this patient?
A) Fidaxomicin
B) Metronidazole
C) Rifaximin
D) Teicoplanin
E) Vancomycin
The correct response is Option B.
Oral metronidazole is the most appropriate treatment for this patient with a mild/moderate form of Clostridium difficile infection.
Oral vancomycin is recommended for treatment of those with severe disease, or with mild/moderate disease who did not respond to metronidazole.
Patients who cannot tolerate oral medications (eg, postoperative ileus) or who have an intestinal diversion (eg, ileostomy) can be treated with intravenous metronidazole or with vancomycin enemas. Vancomycin is not excreted into the colon and therefore should not be given intravenously to treat C. difficile infection.
Oral fidaxomicin has been shown to be as effective as oral vancomycin in the treatment of C. difficile infections. Although further clinical experience is still needed, this drug has been associated with increased cure rate in patients receiving concomitant antibiotics and decreased infection recurrence when compared to vancomycin.
Teicoplanin and rifaximin are not generally recommended for treatment of C. difficile, although isolated reports of successful therapy can be found in the literature.
A 30-year-old man with AIDS is evaluated for a 6-week history of painless but increasing swelling of the flexor surfaces of the right wrist. Physical examination shows limited motion of the wrist and positive Phalen and Tinel signs. At the time of surgical exploration, rice bodies are present in the flexor tenosynovium. Which of the following is the most likely diagnosis in this patient?
A) Aspergillus fumigatus
B) Mycobacterium tuberculosis
C) Nocardia asteroides
D) Sporothrix schenckii
E) Vibrio vulnificus
The correct response is Option B.
Rice bodies are pathognomonic for tuberculosis.
Ziehl-Neelsen staining confirms the presence of acid-fast bacilli. All Mycobacterium and Nocardia species are potentially acid-fast. Many of these organisms are fastidious, so false-negative results are common. Surgeons should obtain multiple tissue samples and alert the laboratory that a diagnosis of tuberculosis is suspected. M. tuberculosis is traditionally cultured in Löwenstein-Jensen culture medium under specific temperature conditions 37.0°C (98.6°F). Histologic examination of specimens shows a granulomatous inflammatory process with the central portion of the granulomas appearing caseated.
If a mycobacterial infection is suspected, a Mantoux test should be performed. The test involves purified protein derivative injection into the dermis and evaluation of the cutaneous site after 48 to 72 hours.
M. tuberculosis should be considered in all immunocompromised patients. The other organisms can all be seen in hand infections in immunocompromised patients but do not produce rice bodies.
A 28-year-old, right-hand–dominant woman is brought to the emergency department 18 hours after sustaining a cat bite to the dorsum of the hand proximal to the fifth metacarpophalangeal (MCP) joint. Which of the following organisms is most likely to be cultured from this abscess?
A) Eikenella corrodens
B) Group A Streptococcus
C) Methicillin-resistant Staphylococcus aureus
D) Pasteurella multocida
E) Pseudomonas aeruginosa
The correct response is Option D.
Pasteurella multocida is a small, gram-negative coccobacillus that is frequently associated with infections caused by dog and/or cat bites. Local findings are consistent with infection including erythema, warmth, pain and tenderness, and fluctuance or purulent discharge. Delayed treatment may result in chronic deep-space infection and/or osteomyelitis. Treatment involves starting penicillin combined with local wound care as well as surgical incision and debridement if needed.
Methicillin-resistant Staphylococcus aureus (MRSA) is becoming more common in community-acquired hand infections, but is not typically associated with dog or cat bites. Eikenella corrodens is more commonly associated with infections occurring after human bites. Pseudomonas infection is often seen as a nosocomial infection that is very resistant to antibiotics. Group A Streptococcus is a common bacterial infection associated with strep throat.
A healthy 5-year-old boy is evaluated after he is bitten on the hand by a dog. He has an allergy to penicillin. Which of the following prophylactic antibiotic regimens is most appropriate to prescribe?
A) Amoxicillin and clindamycin
B) Ciprofloxacin and metronidazole
C) Clindamycin only
D) Doxycycline and metronidazole
E) Trimethoprim-sulfamethoxazole and clindamycin
The correct response is Option E.
The most appropriate prophylactic regimen to prescribe in this clinical scenario is trimethoprim-sulfamethoxazole and clindamycin.
Dog bites to the hand are potentially dangerous bites that could lead to serious hand infections. The common microorganisms that cause infections in such bites are Pasteurella species, anaerobes, Staphylococcus aureus, and Streptococcus. The ideal antibiotic would have been amoxicillin-clavulanic acid, which covers most of these microorganisms. However, the child is allergic to penicillin, and, therefore, this drug is contraindicated. Another good option would have been amoxicillin and clindamycin (for the anaerobic coverage). However, for the same reason described above, it too cannot be used. Tetracyclines are contraindicated in children under 8 years of age owing to the ill effects on growing teeth and bones. Quinolones are also contraindicated in children under 18 years of age owing to their harmful effects on cartilage and joints. Although this is debatable, currently the use of quinolones in children is restricted by the Food and Drug Administration to certain specific conditions (cystic fibrosis, multidrug-resistant urinary tract infection, and inhalational anthrax). Clindamycin alone does not adequately cover most of the organisms involved, including Pasteurella, which is gram-negative.
A 34-year-old woman comes to the emergency department 5 days after sustaining a cat bite to the left index finger. A photograph is shown. Medical history includes diabetes mellitus type 1. Physical examination shows punctures to the dorsum and volar surfaces of the proximal phalanx, mild fusiform swelling of the digit with tenderness over the flexor tendon sheath, pain with passive extension, and partially flexed posture of the digit. The symptoms have worsened over the past 3 days. Temperature is 99°F (37.2°C). Which of the following is the most appropriate next step in management?
A) Incision and drainage of the puncture sites
B) Inpatient intravenous antibiotics
C) Irrigation of the flexor sheath
D) Outpatient oral antibiotics
E) Splinting immobilization and elevation

The correct response is Option C.
The most appropriate option for this patient is to proceed to the operating room for decompression/drainage of the flexor tendon sheath. This patient has all four of Kanavel’s signs, specifically pain on passive extension, fusiform swelling, flexor tendon sheath tenderness, and flexion of the affected digit. These point towards a diagnosis of flexor tenosynovitis, with the cause being the cat bite she sustained several days prior. Although cat bites only reflect 5% of all animal bites, they represent 76% of all infected bites, thought to be because of the morphology of their long teeth, which simulate a deep puncture wound.
Outcomes studies demonstrate that because of this patient’s diabetes, she is at risk for a poor outcome, specifically the need for amputation and/or decreased total active motion. Other risk factors that can lead to these outcomes include age greater than 43 years, presence of subcutaneous purulence, digital ischemia, and polymicrobial infection. Given that she is at risk and that she has all four Kanavel’s signs, any intervention that is more conservative than operative decompression and drainage may lead to suboptimal outcomes.
Administration of antibiotics (orally or intravenously) is not a substitute for drainage of the flexor sheath, especially in a case that presents more than 48 hours out from initiation of symptoms. Drainage in the emergency department is not as optimal as in the operating room given that the infection may limit efficacy of local anesthesia as well as the need for possible conversion to an open drainage procedure if closed catheter irrigation is insufficient.

A 60-year-old woman who works as a nurse in the intensive care unit (ICU) is scheduled for cardiac bypass surgery. Because she has taken care of many patients with methicillin-resistant Staphylococcus aureus infection, she is interested in topical agents for decolonization. Which of the following regimens is most appropriate for this patient?
A) Clindamycin
B) Linezolid
C) Mupirocin and chlorhexidine
D) Trimethoprim-sulfamethoxazole
E) Vancomycin
The correct response is Option C.
The currently accepted decolonization protocol from the Infectious Diseases Society of America is a combination of topical nasal mupirocin ointment and a chlorhexidine body wash for 5 days. The most robust data for decolonization are in the cardiac surgery literature; the Society of Thoracic Surgeons guidelines recommend routine prophylaxis for all patients undergoing cardiac surgery. These guidelines are based on studies that show a decreased rate of sternal wound infections.
The carriage rate of methicillin-resistant Staphylococcus aureus for health care workers is approximately 5% based on large review studies. As a substantial portion of cases originate from nasal colonization, routine screening and decolonization are recommended in areas where the carriage rate exceeds 10% (Centers for Disease Control and Prevention recommendation).
The other antibiotics listed are reserved for the treatment of infection rather than as part of a decontamination protocol.
A 15-year-old girl has two draining nodules of axillary hidradenitis suppurativa. Each lesion is approximately 10 mm in diameter. The remaining axillary skin shows no abnormalities. After a 6-week course of oral doxycycline and topical mupirocin, the lesions drain less but are still present. Which of the following is the most appropriate treatment for this patient?
A) Complete axillary excision and skin grafting
B) Excision and closure
C) Incision and drainage
D) Intravenous antibiotics
E) Kenalog injection
The correct response is Option B.
This young patient has limited, focal disease that has failed medical management. Local excision is useful for isolated, scattered individual, or linear lesions. More extensive disease that occupies a significant portion of the skin area may be better treated by complete axillary excision. In this younger patient with limited disease, direct excision of the affected areas is a less morbid approach. Negative pressure wound therapy and skin grafts may be optimal coverage treatments for extensive disease, and some local flaps have been described as well. This stubborn disease originates from the apocrine glands and can often be chronic and disabling. The axillae, groin, perineum, and submammary areas can all be affected. Initial treatments include local care, antibiotics, hygiene, and weight loss. Steroid injections may help in early, small lesions, but have limited effectiveness and are painful. After a 6-week course of antibiotics, this patient is not likely to benefit from more treatment. Only excision of the diseased apocrine glands is likely to be effective. Incision and drainage is a suitable treatment for a closed abscess associated with hidradenitis, but incising this patient’s lesions would not improve her situation.
An otherwise healthy 10-year-old girl is brought for evaluation because of a chronic ulcer of the right leg. The ulcer first appeared 6 months ago when she scraped her leg on a boat dock at her family’s lake house. The wound has increased in size despite treatment with a course of oral antibiotic therapy prescribed by her primary care physician. A photograph is shown. On evaluation today, the patient is afebrile and has no systemic signs of infection. Which of the following organisms is the most likely cause of these findings?
A) Candida tropicalis
B) Group A beta-hemolytic Streptococcus
C) Methicillin-resistant Staphylococcus aureus
D) Mycobacterium marinum
E) Vibrio vulnificus
The correct response is Option D.
The history and presentation are classic for an atypical mycobacterial infection. Unlike bacterial infections, atypical mycobacteria rarely produce systemic signs of infection and often manifest as a nonhealing (sometimes progressive) wound. Given the history of injury on a boat dock, the most likely causative organism is Mycobacterium marinum, an acid-fast bacillus that lives in water environments. This pathogen results in localized granulomas such as the one seen in this patient. Staphylococcus aureus is the most common source of skin infections but typically results in a more pronounced and acute immune reaction with localized redness and purulence. These findings are not present in this patient. Cutaneous infections with Group A beta-hemolytic Streptococcus and Vibrio vulnificus tend to increase rapidly and are often accompanied by severe systemic response (i.e., necrotizing fasciitis). Candida tropicalis is a fungus that is often part of normal skin flora. It is related to Candida albicans and can produce opportunistic internal infections in susceptible individuals.
A 46-year-old woman comes to the emergency department because of a 5-day history of profound physical deterioration, nausea, and vomiting. She underwent breast reconstruction 3 weeks ago. Medical history includes delayed right latissimus dorsi tissue expansion breast reconstruction 1 year after completing radiation therapy. She has no other comorbidities. Physical examination shows erythematous rash involving and extending beyond the surgical sites. There are no notable fluid collections and the surgical wounds are not draining. Temperature is 103.5°F (39.7°C) and blood pressure is 90/50 mmHg. Laboratory studies show:
Intraoperative cultures of the explored surgical sites are most likely to grow which of the following organisms?
A) Bacteroides
B) Clostridium
C) Enterobacter
D) Pseudomonas
E) Streptococcus
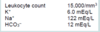
The correct response is Option E.
The Centers for Disease Control and Prevention support criteria indicate that toxic shock syndrome may be diagnosed when patients present with a temperature exceeding 102°F (38.9°C), multisystems organ failure, rash, and/or multiple constitution symptoms.
Exotoxin1 and exfoliative toxin-producing Staphylococcus aureus are the most common pathogen, but enterotoxin A, B, and C, producing Streptococcus pyogenes infections, yield a worse prognosis. Blood cultures may be negative for the causitive organism.
Although Clostridium, Enterobactor, Pseudomonas, and Bacteroides species are polymicrobial species associated with necrotozing fasciitis, the description of this otherwise healthy patient is not consistent with its typical presentation of discolored blistered skin and crepitus.
A 45-year-old man is brought to the emergency department with a Gustilo IIIB tibial fracture that he sustained falling off a tractor in a pasture. Medical history shows no drug allergies. Administration of which of the following antibiotics is most appropriate in this patient?
A) Amoxicillin
B) Ceftriaxone
C) Ciprofloxacin
D) Clindamycin
E) Vancomycin
The correct response is Option B.
The most appropriate antibiotic prophylaxis for this patient with a Gustilo grade III fracture is a third generation cephalosporin. Although much debate exists regarding antibiotic prophylaxis in open tibial fractures, it is generally accepted that antibiotic prophylaxis reduces the rate of infection. When antibiotic prophylaxis is not used, infection occurs in approximately 24% of open fractures. Thus, selecting the appropriate antibiotic, as well as duration, is of utmost importance. Antibiotic prophylaxis should be administered as soon as possible after injury and should be limited to a 72-hour course. In general, broad-spectrum antibiotics and multiple antibiotics should be avoided because they have been shown to increase the risk of nosocomial infections, including pneumonia. Of the antibiotics listed, the most appropriate choice for a patient with no drug allergies is ceftriaxone. Clindamycin and vancomycin should be reserved for cases of true penicillin allergy. Ciprofloxacin alone has been shown to be inferior to prevent infection after open tibial fractures.
A 29-year-old woman is evaluated because of a 2.5-year history of painful, draining lesions from the axillae and groin. Physical examination shows multiple nodules and abscesses. Conservative treatment with loose clothing, topical antibiotics, and antibacterial washes is unsuccessful. These findings are most consistent with which of the following disease processes?
A) Candidal infection of the intertriginous areas
B) Follicular occlusion of the apocrine sweat gland areas
C) Follicular occlusion of the eccrine sweat glands areas
D) Inflammatory and ulcerative skin condition mediated by neutrophils
E) Sexually transmitted infection caused by Klebsiella granulomatis
The correct response is Option B.
Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic inflammatory disease of the skin and subcutaneous structures. Initially presenting as tender, subcutaneous nodules, the disease can advance to cause abscesses and large areas of subcutaneous scarring and draining sinus tracts.
Historically, HS has been thought to originate from the apocrine sweat glands. However, research in recent years has demonstrated that the mechanism is one of follicular occlusion: hair follicles become occluded due to an overproliferation of ductal keratinocytes, rupture, and subsequently re-epithelialize. As this cycle continues, sinus tracts form that house bacteria and cause chronic, painful infections and inflammation that can involve the skin and subcutaneous structures including muscle, fascia, and lymph nodes.
HS lesions typically occur predominately in the apocrine-gland bearing areas of the axillary, inguinal, perianal, and perineal areas. Lesions typically correspond with the “milk-line” pattern of apocrine-related mammary tissue in mammals.
Eccrine, or merocrine, sweat glands are found throughout the body, but their highest concentrations are in the palms and soles. These areas are typically spared by HS.
Follicular pyodermas, including folliculitis, furuncles, and carbuncles, arise primarily from the infection of hair follicles. They do not cause the sinus tracts, comedones, and scarring caused by HS.
Granuloma inguinale is a sexually transmitted infection of the genitalia, perineum, and/or perineal area caused by Klebsiella granulomatis.
Pyoderma gangrenosum is a dermatologic condition mediated by neutrophils that causes skin ulceration and breakdown.
A 5-year-old boy is brought to the emergency department after sustaining a traumatic amputation of the right thumb. Medical history includes an allergy to sulfa drugs. The thumb is successfully replanted, and the patient is admitted for observation. Twenty-four hours postoperatively, venous congestion of the replanted thumb is noted. Leeches are placed to improve congestion. It is suspected that the leeches will be required for several days until venous outflow is reestablished. Administration of which of the following antibiotics is most appropriate?
A) Cefotaxime
B) Ciprofloxacin
C) Clindamycin
D) Tetracycline
E) Trimethoprim-sulfamethoxazole
The correct response is Option A.
Medicinal leeches are still commonly used as an adjunct in the treatment of venous congestion. They secrete a powerful anticoagulant called hirudin that promotes bleeding in the congested tissues until venous outflow can be reestablished. Leeches are also known to harbor the gram-negative bacterium Aeromonas. Because leeches can be exposed to open wounds on the patient for several days during treatment, antibiotic prophylaxis against Aeromonas is recommended.
Ciprofloxacin, tetracycline, trimethoprim-sulfamethoxazole (Bactrim), and third-generation cephalosporins have all been shown to be effective against Aeromonas. However, in the scenario above, all of these antibiotics have a contraindication except cefotaxime, a third-generation cephalosporin.
Ciprofloxacin is contraindicated in children when a suitable alternative exists secondary to the risk of arthropathy and arthrotoxicity. Similarly, the use of tetracycline is relatively contraindicated in children owing to the potential for abnormalities with the teeth, including permanent staining and growth retardation. While Bactrim is often used in children to treat various infections, this child has an allergy to sulfa drugs and should not be given this antibiotic.
Clindamycin does not provide effective antibiotic coverage against Aeromonas.
A 67-year-old man with type 1 diabetes mellitus is evaluated for full-thickness perineal burns sustained by falling onto a space heater. Forty-eight hours after admission, he has onset of fever and tachycardia. Complete blood cell count grows leukocytosis, and wound culture shows gram-negative rods consistent with Pseudomonas. Pending sensitivity report, empiric coverage is initiated. Which of the following antibiotics is clinically CONTRAINDICATED for initial therapy?
A) Ceftazidime
B) Ceftriaxone
C) Ciprofloxacin
D) Imipenem
E) Tigecycline
The correct response is Option E.
Although tigecycline has excellent coverage of most staphylococcal and many gram-negative rod infections, this tetracycline derivative is not effective against pseudomonal infections. Patients with pseudomonal sepsis benefit from double coverage. Furthermore, sensitivities to different antimicrobial agents are quite variable from one health care system to another, so providers must remain vigilant after beginning therapy and change coverage based on lack of clinical response and determination of final sensitivities. An essential component of this patient’s care would be urgent burn wound excision, after he has been resuscitated and empiric antibiotics have been initiated.














