scrotum Flashcards
(102 cards)
At __ weeks of gestation female and male embryo appear identical
7-8
•
Testes develop from area near where the ____ develop, and about the same time
•
kidneys
____ month the testes descend through inguinal canal into the scrotum
•
8th – 9th
________ is the condition when 1 or both testes don’t reach the scrotum. Occasionally a testicle may remain undescended and will need to be surgically brought down where it will be sutured into the scrotum.
This procedure is called_______.
Cryptorchidism
ORCHIOPEXY
Between the 3rd and 9th month of pregnancy the testes descend from the____ area (medial to the mesonephros, remember this tissue? It is the second fetal kidney) into the future scrotum. The descend is due to a combination of ______________.
lumbar
growth processes and hormonal influences
The_______ also plays a decisive role in testis descent. When does it develop?
Cranially it has its origin at the testis and inserts in the region of the genital swelling (future scrotum).
At the same time, at the inguinal canal along the lower gubernaculum, an evagination of the peritoneum arises, the vaginal process, on which the testes will slide through the inguinal canal.
gubernaculum testis
IT develops in the 7th week from the lower gubernaculum, after the mesonephros has atrophied.
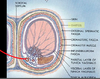
testicular development at 2 months. label.

- Gubernaculum testis 2. Penis 3. Inguinal canal
- Testis 5. Peritoneal cavity 6. Deferent duct
what is the arrow pointing to?

parietal peritoneal lining. (it pulls the lining down as it descends)
In this diagram, the beginning of the formation of the vaginal process is visible. It enters with the testis into the inguinal canal. Shown in blue is the gubernaculum that becomes increasingly shorter.
Between the____ and ____ month of pregnancy the testes remain near the inguinal canal in order to pass through it. The vaginal process lengthens while the gubernaculum shortens, thereby drawing the testis, the deferent duct and its vessels on both sides downwards
3rd and 7th

In the____ month of pregnancy (but also sometimes only after birth) the testes reach the scrotum. The vaginal process forms now a serous bilaminar structure on the front side of the testis.
9th

serous bilaminar
The parietal layer: lines the scrotal sac The visceral layer: surrounds the testicle
serous memebrane
This type of tissue creates a____ in the scrotum or_____ within the abd. of pleural fluid within the thorax.
scrotum lining – a serous membrane (or serosa) is a smooth membrane consisting of a thin layer of cells which secrete serous fluid.
hydrocele, ascites
process vaginalis
canal created by descent

bare area
no visceral tunica vaginalis (lymphatics, nerves, veins and sperm exit this area)

testes are _____ in fetal life.
retroperitoneal
scrotum
sac of skin continuous w/ the abdomen
•
_____muscles within scrotal wall; controls the contraction of the scrotal skin. The contraction of the skin will drawl the testes closer to the body.
Dartos
causes skin to pucker, regulating temperature. autosomal ( we can’t control it) but can be a problem (caused by nerves, temp) you get a lousy image then on US
the scrotum sac is divided into 2 halves by the ____. ____ divides the scrotum into a rt and lt hemishere
septum
median raphe
what does each hemiscrotum contain?
A testis
An epididymis
A portion of spermatic cord
A vas deferens (ductus deferens) (makes sperm)
what can you see here? why?

Median Raphe
•
Scrotal wall is inflamed but the median raphe is clearly seen separating the two hemiscrotums.
notice the lobules in the testes. what do they contain?

seminiferous tublues (place sperm is made)
what is the testes endocrine function?
what type of cells are found here?
testosterone
Sertoli cells: provide nourishment to the sperm cells
–
Leydig Cells: These cells are in the intestinal space and secrete the male sex hormone testosterone
Cross section of a Seminiferous tubules

what are the testes exocrine functions?

spermatozoa (germ cell) via- Seminiferous tubules
–
spermatogonium cells develop into sperm
–
primitive sperms cells are peripheral
–
immature sperm cells at the lumen
–
once in the lumen sperm travel to the epididymis to mature

what is the tete testes
–
Within the mediastinum still beneath the tunica albuginea
–
Connects seminiferous tubules to epididymis


















































