L51. Larynx and Laryngopharynx Flashcards
Define the vertical borders of the larynx
Starts from epiglottis and continues to the top of trachea (lower border of cricoid cartilage/C6)
Describe the shape and structure of the larynx
The larynx is a tube that is supported by a system of cartilages giving it its 3D shape.
It is open posteriorly at the superior part to the pharynx called the LARYNGEAL INLET that allows air to come in and out of the airways

What are the main skeletal structures making up the larynx [4]?
- Hyoid Bone
- Epiglottis
- Thyroid Cartilage
- Cricoid Cartilage

Describe the thyroid cartilage of the larynx
- Anteriorly, it has an angle (sharp projection sticking out and is palpable in the midline) called laryngeal prominence or adams apple.
- It has laminae laterally
- It has large projections that point upwards and downwards off the posterior aspect.
- It is open posteriorly for the laryngeal inlet (communication between pharynx and airways)

Describe the cricoid cartilage
A completely closed ring of cartilage that encricles the whole top of the trachea.
It has a short anterior arch and tall posterior laminae

What are the membranes connecting the major structures of the larynx?
- Thyrohyoid membrane connecting the hyoid bone to the thyroid cartilage
- Cricothyroid membrane connecting the inferior aspect of the thryoid bone to the superior aspect of the cricoid cartilage

What is important about the posteriolateral aspect of the superior part of the cricoid cartilage?
It has small cartilages called Arytenoid cartilages which are pyramidal in shape.
- Each one has two major processes that project towards the front and midline
- Vocal processes anteromedially that attach to vocal ligamants
- Muscular processes laterally for muscle attachment.

Describe the movements of the arytenoid cartilages
They have 2 major movements:
They swivel on an axis that runs straight down through the middle of the cartilages
- Can slide towards each other on the lamina of the cricoid cartilation (contributes to closing the vocal ligaments)
- Can slide away from each other
Where is the epiglottic cartilage, what is the major function?
It projects/originates from posterior aspect of the angle of the cricoid cartilage (anteriorly) and fans out to a top projection that sits behind posterior third of the tongue and hyoid bone.
It is very important as the tongue and food bolus physically push the epiglottis down during swallowing to project laryngeal inlet

Where do the vocal ligaments arise and attach to?
They run from the tips of the two vocal processes of the arytenoid cartilages posteriorly and project anteriorly through the midline towards the posterior aspect of the angle of the thyroid cartilage.

Describe the formation of the vestibular (false) and vocal (true) cords
A mucosa lines the epiglottis and it runs down on the internal wall of the lamina of the thyroid cartilage.
It hits a membrane along the path (don’t need to know this membrane) and produces a vestibular fold just above the vocal ligament and that projects outwards toward the thyroid cartilage
The mucosa then runs down the thyroid cartilage and then folds back up over the top of the vocal ligament forming the vocal cords and then continues down in the airways

How is the vestibular fold involved in phonation?
It is not
It lies superior to the true sound producing vocal cords and helps to close the glottis during swallowing
What position to the vocal cords need to be in, in order to produce phonation?
Vocal ligaments need to be adducted for phonation and abducted for breathing
When they are adducted towards each other in the midline they push against each other and vibrate to create the sound

How are various different types of sounds produced if there is only the adduction/abduction swivel action of the arytenoid cartilages?
The various sounds are altered by related structures like the mouth and oral cavity, nasal cavity and muscles.
What causes the arytenoid cartilages to move and thus what causes the vocal cords to move?
Movement of the ligaments and alteration of the postition of the vocal cords in and out requires the intrinsic muscles of the larynx to have action mostly on the arytenoid cartilages and on other muscles to produce movement of the vocal ligaments
What are the major intrinsic muscles of the larynx?
- Posterior cricoarytenoid
- Lateral cricoarytenoid
- Transverse and oblique arytenoids
- Cricothyroid
- Vocalis

What are the intrinsic muscles of the larynx that are involved in abduction of the vocal cords? (ie. breathing)
Posterior cricoarytenoid
Damage to this muscle is determinental as it is the only muscle that is responsible for opening the tube to air flow

What are the intrinsic muscles of the larynx that are involved in adduction of the vocal cords? (ie. basic phonation)
The Lateral cricoarytenoid muscle

Describe the role of the cricothyroid muscle
Attaches to the inside lamina of the thyroid cartilage.
It pulls the back end of thyroid cartilage forward (angle moves forward) stretching ligaments causing higher frequency fibration = higher pitched sounds

Describe the role of the cricothyroid and Vocalis muscles
Shortens the vocal ligament (loose) and vibrate with lower frequency

What are the 2 main nerves that supply the intrinsic muscles of the larynx?
All of the intrinsic muscles are ultimately all supplied by branches of the vagus nerve.
Except for the cricothyroid muscle (which is innervated by a branch of the superior laryngeal nerve: from external laryngeal nerve)
What is the major branch of the vagus nerve that supplies the majority of the intrinsic muscles of the larynx?
The recurrent laryngeal nerves that are given off from the vagus nerve (left hooking around the ligamentum arteriosum and the right hooking under the subclavian artery)
What happens to motor innervation of the muscles when there is damage to the recurrent laryngeal nerve?
Causes problems adduction and abduction so ligament is immobilised and can’t move to midline
- Ligaments can’t vibrate against each other = hoarse voice (inappropriate vibration)
- Stridor caused by the effort in producing sound due to large energy to cause vocal ligament to flap
What happens when there is damage to the external laryngeal nerve (which supplies the cricothyroid muscle)?
Difficulty with production of high pitch sounds as the muscle isn’t able to pull the vocal cords and lengthen them. The patient will still be able to produce sound and breath
What nerves supply the sensory innervation to the mucosa of the larynx?
What are the important reflexes that these nerves are involved in?
Inferior laryngeal and the Inferior laryngeal, which are still branches off the recurrent laryngeal nerve
They provide the sensory to mucosa below the vocal ligament. They are important for coughing and gag reflex
The larynx is a very vascular region. Describe the blood supply
Blood supply comes from thyroid vessels above and thyroid vessels from below supplying blood to the thyroid gland (on top of the trachea) and gives off little branches going to the larynx itself

What is the difference between a tracheotomy and a cricothyroid membrane puncture. What are the considerations of doing the two?
A tracheotomy is cutting into the trachea. You need to cut through the inferior thyroid vessels in the area of the trachea for a tracheotomy. Cutting of the vessels causes bleeding directly into the airways (drowns the person). However if it is not an emergency situation, it is a bigger area and good access.
Cricothyroid membrane is the area where there isn’t a lot of vasculature in the midline below the level of the vocal ligaments. So it is a good place to go in emergencies
Consider path of intubation tube for artificial ventilation

What is the area behind the larynx?
The laryngopharynx
The epiglottis doesn’t form a perfect seal around the larynx. What helps to compensate for this?
The larynx moves up as you swallow (meeting the epiglottis above forming the tight seal)
Fluids don’t normally go through the larynx through the main tube. Why is this and how does the fluid enter the oesophagus?
Fluids don’t have the weight to push the epiglottis, so they drain into the piriform recess which are little grooves (channels) out and around epiglottis
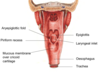
What are the main components of the laryngopharynx? Label the following diagram:

Describe the sensory innervation to the pharynx
The entire pharynx is mainly supplied by pharyngeal branches coming of the glossopharyngeal nerve (CN IX).
This innervation is reinforced by some branches of the trigeminal nerve (pharyngeal branches of the maxillary nerve) superiorly and the branches of the vagus nerve inferiorly – internal laryngeal nerve (mucosa above the vocal ligaments)

Give examples of referred pain from different parts of the larynx to different parts of the face (nerve distribution)
Eg. The middle ear mucosa also innervated by the glossopharyngeal nerve. Middle ear infections can have pain referring to the palatine tonsils in the oropharynx
What is the major motor nerve supply to the pharynx?
- Mostly from pharyngeal branches of Vagus (CN X)
- Except for Stylopharyngeus muscle which is supplied by CN IX
What are the pharyngeal branches of the vagus nerve responsible for in terms of important reflexes?
Swallowing and Efferent arc of gag reflex
Describe the steps in the deglutition (swallowing) process [8 steps]
- Bolus shaped and pushed by tongue to palate.
- Soft palate descends and palatal arches are approximated to grip and push the bolus into the oropharynx.
- Soft palate elevated and tightened to prevent bolus entering nasal cavity.
- Larynx and pharynx elevated to bring bolus closer to oesophagus.
- Laryngeal inlet closed to prevent bolus from entering the trachea.
- Bolus is pushed down the oropharynx and over the epiglottis.
- Bolus forced down through laryngopharynx and into oesophagus.
- Larynx depressed to return to normal position (mainly by elastic recoil).


