Immunology (All Topics) Flashcards
Diagnosis and management of immunodeficiencies:
What are the consequences of Phagocyte deficiencies?

Diagnosis and management of immunodeficiencies:
How are Phagocyte deficiencies investigated?

Diagnosis and management of immunodeficiencies:
How are Phagocyte deficiencies managed?

Diagnosis and management of immunodeficiencies:
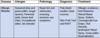
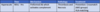
What are the C3, C4 CH50 and AP50 findings in:
- C1q deficiency
- Factor B deficiency
- C9 deficiency
- SLE

Diagnosis and management of immunodeficiencies:
What are the consequences of Complement deficiencies?

Diagnosis and management of immunodeficiencies:
How are complement deficiencies diagnosed?

Diagnosis and management of immunodeficiencies:
How are complement deficiencies treated?

Diagnosis and management of immunodeficiencies:
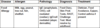
What are the features of T Cell Deficiency vs Antibody deficiency (or CD 4 T cell deficiency)?

Diagnosis and management of immunodeficiencies:
How are Lymphocyte deficiencies diagnosed?

Diagnosis and management of immunodeficiencies:
How are Lymphocyte deficiencies managed?

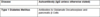
Type I Hypersensitivity disorders:
What is/are the definition of, symptoms and epidemiology of Type 1 hypersensitivity disorders?

Type I Hypersensitivity disorders:
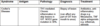
What is the allergen, pathology, diagnosis and treatment of Atopic Dermatitis (infantile eczema)?

Type I Hypersensitivity disorders:
What is the allergen, pathology, diagnosis and treatment of Food Allergy?
Type I Hypersensitivity disorders:
What is the allergen, pathology, diagnosis and treatment of Oral Allergy Syndrome?

Type I Hypersensitivity disorders:
What is the allergen, pathology, diagnosis and treatment of Latex Food Syndrome?

Type I Hypersensitivity disorders:
What is the allergen, pathology, diagnosis and treatment of Allergic Rhinitis?
Type I Hypersensitivity disorders:
What is the allergen, pathology, diagnosis and treatment of Acute Urticaria?

Type I Hypersensitivity disorders:
What is/are the definition and management of Anaphylaxis?

Type I Hypersensitivity disorders:
What are the features of the skin prick test?

Type I Hypersensitivity disorders:
What are the features of the Quantitative specific IgE putative allergen (RAST)?

Type I Hypersensitivity disorders:
What are the features of the component resolved diagnostics?

Type I Hypersensitivity disorders:
What are the features of the Challenge test?

Type I Hypersensitivity disorders:
What should be measured during an acute anaphylaxis episode?

Type II Hypersensitivity disorders:
What is the definition of Type II Hypersensitivity disorders?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Haemolytic Disease of the Newborn?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Autoimmune haemolytic anaemia?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Autoimmune Thrombocytopenic purpura?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Goodpasture’s syndrome?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Pemphigus Vulgaris?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Grave’s Disease?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Myasthenia Gravis?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Acute Rheumatic Fever?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Pernicious Anaemia?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Churg-Strauss syndrome?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Wegener’s Granulomatosis (GPA)?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Microscopic Polyangiitis (MPA)?

Type II Hypersensitivity disorders:
What is the antigen, pathology, diagnosis and treatment for Chronic Urticaria?

Type III Hypersensitivity Disorders:
What is the definition of Type III Hypersensitivity disorder?

Type III Hypersensitivity Disorders:
What is the antigen, pathology, diagnosis and treatment for Mixed Essential Cryoglobulinaemia?

Type III Hypersensitivity Disorders:
What is the antigen, pathology, diagnosis and treatment for Serum Sickness?

Type III Hypersensitivity Disorders:
What is the antigen, pathology, diagnosis and treatment for Polyarteritis Nodosa (PAN)?

Type III Hypersensitivity Disorders:
What is the antigen, pathology, diagnosis and treatment for Systemic Lupus Erythematosus (SLE)?

Type IV Hypersensitivity Disorders:
What is the definition of Type IV Hypersensitivity disorder?

Type IV Hypersensitivity Disorders:
What is the antigen, pathology, diagnosis and treatment for Type 1 Diabetes Mellitus?

Type IV Hypersensitivity Disorders:
What is the antigen, pathology, diagnosis and treatment for Multiple Sclerosis?

Type IV Hypersensitivity Disorders:
What is the antigen, pathology, diagnosis and treatment for Contact Dermatitis?

Type IV Hypersensitivity Disorders:
What is the antigen, pathology, diagnosis and treatment for Mantoux Test?

Type IV Hypersensitivity Disorders:
What is the antigen, pathology, diagnosis and treatment for Crohn’s Disease?
Type IV Hypersensitivity Disorders:
What is the antigen, pathology, diagnosis and treatment for Rheumatoid Arthritis?

HLA Associations:
What is the susceptibility allele and risk factor increase for:
- Ankylosing spondylitis
- Goodpasture’s syndrome
- Grave’s Disease
- Systemic Lupus Eyrthematosis (SLE)
- Type I Diabetes
- Rheumatoid Arthritis

HLA Associations:
What are PTPN22 and CTLA4 associated with?

Important other diseases:
What is/are the aetiology, symptoms, investigations and complications for Limited cutaneous scleroderma (CREST Syndrome)?

Important other diseases:
What is/are the aetiology, symptoms, investigations and complications for Diffuse cutaneous scleroderma?

Important other diseases:
What is/are the aetiology, symptoms, investigations and complications for IPEX syndrome?

Important other diseases:
What is/are the aetiology and symptoms of Coeliac Disease?

Important other diseases:
What are the investigations for Coeliac Disease?

Important other diseases:
What is/are the complications, epidemiology and gold standard investigation for Coeliac Disease?

List of Autoantibodies:
What are the 4 extractable extracelular nuclear antibodies?

List of Autoantibodies:
What are the antibodies for Antiphospholipid Syndrome (Hugh’s Syndrome)?

List of Autoantibodies:
What are the autoantibodies for Autoimmune hepatitis?

List of Autoantibodies:
What are the autoantibodies for Autoimmune haemolytic Anaemia?

List of Autoantibodies:
What are the autoantibodies for Autoimmune Thrombocytopenic Purpura?

List of Autoantibodies:
What are the autoantibodies for Churg-Strauss Syndrome (eGPA)?

List of Autoantibodies:
What are the autoantibodies for Coeliac disease?

List of Autoantibodies:
What are the autoantibodies for Congenital heart block in infants of mothers with SLE?

List of Autoantibodies:
What are the autoantibodies for Dermatitis herpetiformis?

List of Autoantibodies:
What are the autoantibodies for Dermatomyositis?

List of Autoantibodies:
What are the autoantibodies for Diffuse Cutaneous Scleroderma?

List of Autoantibodies:
What are the autoantibodies for Goodpasture’s Syndrome?

List of Autoantibodies:
What are the autoantibodies for Graves Disease?

List of Autoantibodies:
What are the autoantibodies for Hashimoto’s Thyroiditis?

List of Autoantibodies:
What are the autoantibodies for Limited cutaneous scleroderma (CREST)?

List of Autoantibodies:
What are the autoantibodies for Microscopic Polyangiitis (MPA)?

List of Autoantibodies:
What are the autoantibodies for Mixed connective tissue disease?
List of Autoantibodies:
What are the autoantibodies for Myasthenia Gravis?

List of Autoantibodies:
What are the autoantibodies for Pernicious anaemia?

List of Autoantibodies:
What are the autoantibodies for Polymyositis?

List of Autoantibodies:
What are the autoantibodies for Primary biliary cirrhosis?

List of Autoantibodies:
What are the autoantibodies for Rheumatoid Arthritis?

List of Autoantibodies:
What are the autoantibodies for Sjogren’s syndrome?

List of Autoantibodies:
What are the autoantibodies for Systemic Lupus Erythematosis?

List of Autoantibodies:
What are the autoantibodies for Type 1 Diabetes Militus?
List of Autoantibodies:
What are the autoantibodies for Wegener’s Granulomatosis (GPA)?

Boosting immune response:
Outline the broad classification of Immune Modulation therapies

Boosting immune response:
Outline the features of Human Normal Immunoglobulin therapy

Boosting immune response:
Outline the features of Specific Immunoglobulin

Boosting immune response:
Outline the features of Recombinant Cytokines

Boosting immune response:
Outline the features of Blocking immune checkpoints

Immunosuppressive therapies:
Outline the features of injection site reactions

Immunosuppressive therapies:
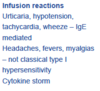
Outline the features of infusion reactions
Immunosuppressive therapies:
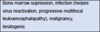
Outline the types of immunosuppressive therapies

Immunosuppressive therapies:
Outline the process of Allergen Desensitization

Immunosuppressant Drugs:
What is the mode of action for Prednisolone?

Immunosuppressant Drugs:
What are the indications for Prednisolone?

Immunosuppressant Drugs:
What are the side effects of Prednisolone?

Immunosuppressant Drugs:
What is the mode of action for Cyclophosphamide?

Immunosuppressant Drugs:
What are the indications for Cyclophosphamide?

Immunosuppressant Drugs:
What are the side effects of Cyclophosphamide?

Immunosuppressant Drugs:
What is the mode of action for Mycophenolate Mofetil?

Immunosuppressant Drugs:
What are the indication for Mycophenolate Mofetil?

Immunosuppressant Drugs:
What are the side effects of Mycophenolate Mofetil?
Immunosuppressant Drugs:
What is the mode of action for Azathioprine?

Immunosuppressant Drugs:
What are the indications for Azathioprine?

Immunosuppressant Drugs:
What are the side effects of Azathioprine?

Immunosuppressant Drugs:
What is the mode of action for Methotrexate?

Immunosuppressant Drugs:
What are the indications for Methotrexate?

Immunosuppressant Drugs:
What are the side effects of Methotrexate?

Immunosuppressant Drugs:
What is the mode of action for Plasmapheresis?

Immunosuppressant Drugs:
What are the indications for Plasmapheresis?

Immunosuppressant Drugs:
What are the main types of immunosuppressant drugs?
-
Corticosteriods:
- Prednisolone
-
Antiproliferative Agents: “CAMM”
- Cyclophosphamide
- Azathioprine
- Myclophosphamide
- Methotrexate
- Plasmapheresis
-
Inhibitors of cell signalling: “TTACS”
- Tacrolimus
- Tofacinib
- Apremilast
- Cyclosporin
- Sirolimus
-
Agents directed at cell surface antigens: “ADAMANT BER”
- Abatacept
- Daclizumab
- Anti thymocyte
- Muromonab CD3
- Alemtuzumab
- Natalizumab
- Tocilizumab
- Basiliximab
- Efalizumab
- Rituximab
-
Agents directed at cytokines “GAUDIES C”:
- Golimumab
- Adalimumab
- Ustekinumab
- Denosumab
- Infliximab
- Etanercept
- Secukinumab
- Certolizumab
Immunosuppressant Drugs:
What are the side effects of Plasmapheresis?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Tacrolimus and Cyclosporine?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Sirolimus, Tofacitinib and Apremilast?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Basiliximab?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Abatacept?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Rituximab?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Natalizumab?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Tocilizumab?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Muromonab-CD3?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Anti-thymocyte globulin (ATG)?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Daclizumab?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Efalizumab?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Infliximab, Adalimumab, Certolizumab and Golimumab?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Etanercept?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Ustekinumab?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Secukinumab?
Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Denosumab?

Immunosuppressant Drugs:
What is/are the mode of action, indications and side effects of Alemetuzumab?

Transplantation:
What is transplantation rejection and what are its stages?

Transplantation:
Outline the process of immune recognition

Transplantation:
What are the antigens recognised following transplant?

Transplantation:
What are the 2 types of recognition in transplant?

Activation and Effector Function:
What is activation and effector function?

Activation and Effector Function:
What are the phases of immune response to transplant?

Activation and Effector Function:
What is the T Cell function in transplant rejection?

Activation and Effector Function:
What is acute vascular rejection?

Activation and Effector Function - Types of Transplant Rejection:
What is the time, mechanism pathology and treatment for Hyperacute Rejection?
Activation and Effector Function - Types of Transplant Rejection:
What is the time, mechanism pathology and treatment for Acute-Cellular Rejection?

Activation and Effector Function - Types of Transplant Rejection:
What is the time, mechanism pathology and treatment for Acute- Antibody Mediated Rejection?

Activation and Effector Function - Types of Transplant Rejection:
What is the time, mechanism pathology and treatment for Chronic Rejection?

Activation and Effector Function - Types of Transplant Rejection:
What is the time, mechanism pathology and treatment for Graft versus Host Disease (GvHD)?

Matching:
How are antigenic differences between donors and recipients reduced?

Matching:
What immune agents are given before a transplant?

Matching:
What immune agents are given after transplant and give some examples?

Matching:
What are used to treat episodes of acute transplant rejection?

Haemopoietic stem cell transplantation (HSCT):
Outline the aetiology, symptoms and treatment of Haemopoietic stem cell transplantation (HSCT)

Haemopoietic stem cell transplantation (HSCT):
What is an isograft, allograft, xenograft and split graft?

Haemopoietic stem cell transplantation (HSCT):
What are the infection related post transplant complications?

Haemopoietic stem cell transplantation (HSCT):
What are the malignancy related post transplant complications?

Haemopoietic stem cell transplantation (HSCT):
What are the Cardiovascular related post transplant complications?

Haemopoietic stem cell transplantation (HSCT):
What are the sources of Allografts?

Pathogenesis:
What is the very basic aetiology of HIV?

Epidemiology:
How many people are living with HIV and how many have died from AIDS?

Epidemiology:
How many people are infected with HIV each day?

Epidemiology:
How is HIV transmitted and how does it gain entry to cells?

Pathogenesis:
What is the innate response to HIV?

Pathogenesis:
What is the adaptive response to HIV?

Pathogenesis:
How does HIV damage the immune response?

Life cycle:
What is the life cycle of HIV?

Natural history:
What is the natural history of HIV?

Natural history:
Outline the changes in Mucosal CD4 T cells, CD4 T cell counts in blood, Viremia and Immune activation in HIV over weeks, years and months.

Diagnosis:
What is the screening test and confirmation test for HIV?

Diagnosis:
What investigations happen after diagnosis?

Treatment:
What is the current treatment of HIV?

Treatment:
What is HIV treatment in Pregnancy?

Treatment:
What are the limitations of HAART?

Treatment:
Outline the treatment diagram for HIV

HIV Treatment:
What are the examples and side effects of Fusion inhibitors?

HIV Treatment:
What are the examples and side effects of Attachment inhibitors?

HIV Treatment:
What are the examples and side effects of Nucleoside Reverse Transcriptase inhibitors (NRTI)?

HIV Treatment:
What are the examples and side effects of Non-NRTI?

HIV Treatment:
What are the examples and side effects of Integration inhibitors?

HIV Treatment:
What are the examples and side effects of Protease inhibitors?

HIV Treatment:
What are the examples and side effects of Nucleotide RTI?

Vaccination:
Outline the schedule of childhood vaccination
- D = Diphtheria
- T = Tetanus
- aP = acellular Pertussis (whooping cough)
- IPV = Inactivated Polio
- HiB = Haemophilus influenza type b
- MMR = Measles, mumps
- rubella PCV = Pneumococcal conjugate vaccine
- Men C = Meningitis C
- R = rotavirus gastroenteritis (oral)
- HPV = Human papilloma virus type 16,18 (3 injections at 1,3,6 months)

Vaccination:
Who are at risk individuals?

Vaccination:
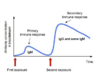
What is the progression of antibody concentration in first and second exposures?
Vaccination:
What does vaccination rely on?

Vaccination:
What is herd immunity?

Vaccination:
What are Antigen Presenting Cells (APCs)?

Vaccination:
What are the locations, antigens, cytokines and memory types of Central and Effector memory cells?

Vaccination:
What do CCR7, CCL19, CCL21 and CD62L do?

Vaccination:
What antigens do T Memory cells have and what do they bind to?

Vaccination:
What are the features of B Memory Cells?

Vaccination:
Outline the T helper cell response

Vaccination:
What are the features of the perfect vaccination?
1

Vaccination:
What is the progression of a vaccine?

Vaccination:
What are the different routes of admission of vaccines?

Vaccination:
Which cells mediate the response to Influenza and TB vaccines?

Vaccination:
What are the ways to ensure a good response to generate effective memory?

Vaccination:
What are the Cancer Vaccines?

Vaccination:
What are the Alzheimer’s disease Vaccines?

Vaccination:
Why don’t vaccinations for effectively in the elderly?

Vaccination:
What are the indications for bone marrow transplantation?

Types of Vaccine:
What are the advantages of live vaccines?

Types of Vaccine:
What are the disadvantages of live vaccines?

Types of Vaccine:
What are the examples of live vaccines?

Types of Vaccine:
What are the advantages of inactivated vaccines?

Types of Vaccine:
What are the disadvantages of inactivated vaccines?

Types of Vaccine:
What are the examples of inactivated vaccines?

Types of Vaccine:
What is the definition of a DNA vaccine?

Types of Vaccine:
What are the advantages of DNA vaccines?

Types of Vaccine:
What are the disadvantages of DNA vaccines?

Types of Vaccine:
What are the examples of DNA vaccines?

Types of Vaccine:
What types of vaccines can HIV patients not have and which ones are okay?

Vaccination:
What is the definition of a Vaccine Adjutant?

Vaccination:
What is the action of Depot adjuvant?

Vaccination:
What is the action of ALUM adjuvant?
Vaccination:
What is the action of CpG adjuvant?
Vaccination:
What is the action of Complete Freund’s adjuvant?

Vaccination:
What is the action of ISCOMS (Immune Stimulating Complex) adjuvant?

Vaccination:
What is the action of Interleukin 2 adjuvant?

Vaccination:
What are the passive vaccines?

Vaccination:
What is the Mantoux test?

Vaccination:
- Who are at risk groups?
- Which Vaccinations are needed for travel?
- Who needs the BCG? Who needs T/IP vaccine?
- Who needs DTaP/IPV vaccine?
- Who needs Shingles vaccine?
Primary Immune Deficiencies:
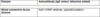
What are the CD4, CD8, B Cell, IgM and IgG changes in:
- SCID
- Di George
- BLS

Primary Immune Deficiencies:
What are the CD4, CD8, B Cell, IgM, IgG and IgA changes in:
- SCID
- Brutons
- Hyper IgM
- Selective IgA Deficiency
- CVID

Primary Immune Deficiencies:
What are the Neutrophil count, Leukocyte adhesion markers, Nitroblue test of oxidative killing (NBT) and pus findings in:
- Kostmann syndrome
- Leukocyte adhesion deficiency
- Chronic Granulomatous disease

Primary Immune Deficiencies:
What are the features, disease and disease characteristics of External epithelia deficiencies?

Primary Immune Deficiencies:
What are the features, disease and disease characteristics of Mucosal surfaces deficiencies?

Primary Immune Deficiencies:
What are the features, disease and disease characteristics of Commensal bacteria deficiencies?

Primary Immune Deficiencies:
What are the features and disease characteristics of Reticular dysgenesis?

Primary Immune Deficiencies:
What are the features and disease characteristics of Kostmann syndrome?

Primary Immune Deficiencies:
What are the features and disease characteristics of Cyclic neutropenia?

Primary Immune Deficiencies:
What are the features and disease characteristics of Leukocyte adhesion deficiency?

Primary Immune Deficiencies:
What are the features, disease and disease characteristics of Phagocytosis deficiencies?

Primary Immune Deficiencies:
What are the features and disease characteristics of Chronic granulomatous disease? Including:
- Absent respiratory burst
- Excessive inflammation

Primary Immune Deficiencies:
What are the features and disease characteristics of Chronic granulomatous disease? Including:
- Symptoms
- Investigations performed

Primary Immune Deficiencies:
What are the features, disease and disease characteristics of Recruitment of other cell deficiencies?

Primary Immune Deficiencies:
What are the features, disease and disease characteristics of Alternative Pathway deficiencies?

Primary Immune Deficiencies:
What are the features and disease characteristics of Deficiencies in early classical Pathway (C1/2/4)?
Include:
- Aetiolgy
- Depoisition sites

Primary Immune Deficiencies:
What are the features and disease characteristics of Secondary Classical Pathway deficiencies?

Primary Immune Deficiencies:
What are the features, disease and disease characteristics of Mannose binding lectin deficiencies?

Primary Immune Deficiencies:
What are the features and disease characteristics of C3 Deficiencies?

Primary Immune Deficiencies:
What are the features and disease characteristics of Secondary C3 deficiencies?
Don’t confuse with secondary Classical pathway deficiencies, which are caused by active lupus depleting the complement

Primary Immune Deficiencies:
What are the features, disease and disease characteristics of terminal common pathway deficiencies?

Primary Immune Deficiencies:
What are the features, disease and disease characteristics of Haem stem cell deficiencies?

Primary Immune Deficiencies:
What are the features and disease characteristics of SCID?
Include:
- Clinical presentation
- Family history

Primary Immune Deficiencies:
What are the features and disease characteristics of X-linked SCID? Include:
- Epidemiology
- Genetics

Primary Immune Deficiencies:
What are the features and disease characteristics of DiGeorge syndrome?

Primary Immune Deficiencies:
What is the clinical presentation of Bare lymphocyte Type II syndrome?

Primary Immune Deficiencies:
What is the aetiology of Bare lymphocyte Type II syndrome?

Primary Immune Deficiencies:
What are the features and disease characteristics of Bruton’s X-linked hypogammaglobulinemia?

Primary Immune Deficiencies:
What are the features and disease characteristics of Hyper IgM Syndrome? Include:
- Definition
- Genetics

Primary Immune Deficiencies:
What are the features and disease characteristics of Hyper IgM Syndrome? Include:
- Symptoms
- Complications

Primary Immune Deficiencies:
What are the features and disease characteristics of Common variable immune deficiency?

Primary Immune Deficiencies:
What are the features and disease characteristics of Deficiencies in early classical Pathway (C1/2/4)?
Include:
- Complement deficiency
- Clinical phenotype

Primary Immune Deficiencies:
What are the features and disease characteristics of SCID?
Include:
- Associated Pathways
- Effect on Lymphocytes

Primary Immune Deficiencies:
What are the features and disease characteristics of X-linked SCID? Include:
- Phenotype

Primary Immune Deficiencies:
What is are the subclasses of Primary immune deficiencies?
“BACKLIT CHAMP R”
- B Lymphocyte Maturation
- Alternative pathway
- Classical pathway
- Killing
- Lymphoid progenitors
- Immune barriers
- Terminal common pathway/T Cell maturation/T Cell acitvation
- C3
- HAem stem cells
- Mannose binding lectin/Mobilisation of Phagocytes
- Phagocytosis
- Recruitment of other cells
Primary Immune Deficiencies:
What is are the subclasses of Primary immune deficiencies affecting Immune barriers?
Immune barriers:
- External epithelia
- Mucosal surfaces
- Commmensal Bacteria
Primary Immune Deficiencies:
What is are the subclasses of Primary immune deficiencies affecting:
- Mobilisation of Pagocytes
- T Cell activation and effector functions
- T Cell maturation
- B Lymphocyte Maturation
Mobilisation of Phagocytes:
- Production of neutrophils
- Neutrophil maturation
- Migration to site of infection
T Cell activation and effector functions:
- Cytokine release
- T/B Cell communication
T Cell Maturation:
- Thymus
- Positive and negative selection
- Exposure of mature T cells to periphery
B Lymphocyte Maturation:
- Pro B Cells
- Class switching
Important other diseases:
What is/are the epidemiology and symptoms of Sjogren’s Syndrome?

Important other diseases:
What is/are the assocaited antibodies and investigations for Sjogren’s Syndrome?



