Chemical Pathology (All Topics) Flashcards
Fluid balance:
What is:
- The % of body water content
- Ratio of intracellular: extracellular fluid
What are the main types of Extracellular fluid?

Fluid balance:
What is the best analogy for why body cells need a high sodium environment?

Fluid balance:
What is there difference between Osmolality and Osmolarity?

Fluid balance:
What are the Physiological and Pathological determinants of Serum Osmolarity?

Fluid balance:
How is Osmolarity Calculated?

Fluid balance:
How can the difference between Osmolality and Osmolarity be useful?

Sodium:
How is true hyponatraemia defined using serum osmolality?
What is TURP syndrome?

Sodium:
What are the subclassifications of Hyponatraemia and what are their causes?

Sodium:
How can hydration status and Urinary Sodium be used to distinguish true Hyonatraemia?

Sodium:
How does Cirrhosis cause Hyponatraemia?

Sodium:
What is the danger of rapid correction of Hyponatraemia?
What are the possible causes of Hyponatraemia post surgery?

Sodium:
What is the laboratory criteria for Syndrome of Inappropriate ADH (SIADH)?

Sodium:
What are the causes of Syndrome of Inappropriate ADH (SIADH)?

Sodium:
- What is the normal range for blood Sodium?
- How much is freely exchangeable?
- How are serum levels maintained?
- What are ECT levels dependent on?

Sodium:
- What is the definition of Hyponatraemia?
- How should it be treated?
- What different symptoms are caused at different Sodium levels?

Sodium:
What is the treatment for Syndrome of Inappropriate ADH (SIADH)?

Sodium:
What is the definition of Hypernatraemia?

Sodium:
What are the causes of Hypovolaemic Hypernatraemia?

Sodium:
What are the causes of Euvolaemic Hypernatraemia?

Sodium:
What are the causes of Hypervolaemic Hypernatraemia?

Diabetes Insipidus:
What are the clinical features of Diabetes Insipidus?

Diabetes Insipidus:
What is Cranial Diabetes Insipidus?

Diabetes Insipidus:
What is Nephrogenic Diabetes Insipidus?

Diabetes Insipidus:
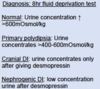
How is Diabetes Insipidus diagnosed?