Histopathology of the gut Flashcards
(41 cards)
What cells line lumen of the oesophagus?
- non keratinising stratified squamous epithelium

In Barrett’s Oesophagus the cells lining the lumen at the distal end of the oesophagus undergo metaplasia, which is the replacement of one cell type to another from the basal cells due to a stimulus. The normal non keratinising stratified squamous epithelium of the lower oesophagus undego metaplasia and become what type of cell and why this type of cell?
- columnar cells
- more equipped to protection of organ such as in the intestines

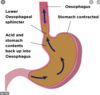
In Barrett’s Oesophagus the cells lining the lumen at the distal end of the oesophagus undergo metaplasia, which is the replacement of one cell type to another from the basal cells due to a stimulus. The normal non keratinising stratified squamous epithelium of the lower oesophagus undego metaplasia and become columnar cells. What is the pathological cause of this?
- acid from stomach causes oesophagitis
- long standing gastro-oesophageal reflux disease
In the image below of the oesophagus we can see where metaplasia has occured and there has been a switch from non keratinising stratified squamous epithelium to column cells. Which number in the image below related to squamous and columnar cells?

1 = columnar cells
2 = non keratinising stratified squamous epithelium
In the image below we can see a healthy Oesophageal- gastric junction (OGJ) and a OGJ in a patient with Barrett’s Oesophagus. Between A and B, which is the healtht and which is the Barrett’s Oesophagus?
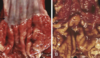
- A = normal
- B = Barrett’s Oesophagus
What is the single most important risk factor for Oesophageal adenocarcinoma?
- Barrette oesophagus
What are the 2 most common clinical presentations of Barretts oesophagus?
- heartburn
- dysphagia (difficulty swallowing)
What is the normal development of Barrettes Oesophagus from squamous cells?
- reflux of gastric contents into the lower oesophagus
- reflux oesophagitis
- metaplasia of squamous epithelium to columnar cells
What is the normal development of squamous cells to Barrettes Oesophagus and then onto Adenocarcinoma?
- squamous epithelium exposed to gastric acid
- reflux disease/oesophagitis
- metaplasia causing Barrettes Oesophagus
- low grade dysplasia
- high grade dysplasia
- adenocarcinoma

Patients with Barrettes Oesophagus undergo regular screening. Why is this?
- biopsies of oesophagus are taken
- screen for dysplasia
What is coeliac disease?
- disease where GIT is sensitive to gluten (specifically gliadin)
- immune-mediated disorder
- causes ucosal lesion of the small intestine and impaired nutrient absorption
- improves on withdrawal of gluten
Coeliac disease is associated with the genes that code for 2 human leukocyte antigens (HLA). What are these genes?
- HLA-DQ2
- HLA-DQ8
In coeliac disease where are biopsies generally taken from?
- duodenum or proximal jejunum

What are the most common histopathological presentation of coeliac disease?
- villi atrophy
- increase inflammatory cells in lamina propria
- increased number of intraepithelial lymphocytes
- elongated and hyperplastic crypts

Diagnosis of ceoliac disease is based on clinical, histological and serological findings. What are the clinical symptoms patients present with?
- sensitivity to gluten
- diarrohoea
- flatulence
- weight loss
- fatigue
Diagnosis of ceoliac disease is based on clinical, histological and serological findings. What are the 4 histological features that will be present on patients biopsies?
1 - atrophy or loss of villi
2 -increased number of intraepithelial lymphocytes
3 - crypts – Elongated and hyperplastic
4 - lamina propria shows increased chronic inflammatory cells
Diagnosis of ceoliac disease is based on clinical, histological and serological findings. What is a key sign of this diease if you remove gluten?
- everything improves
Diagnosis of ceoliac disease is based on clinical, histological and serological findings. What is the serology (study of bodily fluids) diagnosis of celiacs?
- anti tissue transglutaminase (TTG)
- anti-endomysial antibodies
Patients with ceoliacs disease is at risk of complications. What are some of the complications associated with this disease?
- anaemia
- osteoporosis
- primary biliary cirrhosis
- Non-Hodkins lymphoma - Enteropathy-associated T-cell lymphoma
- adenocarcinoma of the small intestine
What are the 2 types of inflammatory bowel disease?
1 - Ulcerative colitis
2 - Crohn’s disease

Who does inflammatory bowel disease affect?
- common in early 20s
Is inflammatory bowel disease a constant disease or is it intermittent?
- chronic, relapsing inflammatory condition
Where crohns and ulcerative colitis (UC) generally affect in the GIT?
- crohns = anywhere
- UC = large bowel only
In crohns disease what do the histopathologists do with biopsies of the the whole GIT?
- macroscopic examination
- from outer to inner side of bowel wall
- disease is intramural (affecting whole wall)






