CNS Blood Supply COPY Flashcards
What proportion of CO is received by brain?
What proportion of O2 does it use?
17%
20%
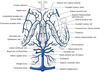
Describe the intracranial course of the carotid artery
Enters the skull in the middle cranial fossa beside the dorsum sellae of the sphenoid.
Carotid siphon- anterior, superior at medial ACP, enters subarachnoid space and courses posteriorly below optic nerve turning upwards lateral to optic chiasm
Divides into terminal branches below anterior perforated substance

Which artery supplies the neurohypophysis?
Inferior hypophyseal

What do the superior hypophyseal arteries supply?
Enter the median eminence of the hypothalamus.
Break up into capillary loops into which hypothalamic releasing factors gain access.
The capillary loops drain through small hypophyseal portal veins into the capillaries of the anterior lobe.

Where is the ophthalmic artery given off?
Immediately after the ICA enters the subarachnoid space
What structures are supplied by the ophthalmic artery?
Eye and other orbital contents
Frontal area of the scalp
Frontal and ethmoid paranasal sinuses
Parts of the nose
What are the branches of the ophthalmic artery?
DR MCLESSI
D: dorsal nasal artery
R: (central) retinal artery
M: muscular artery
C: ciliary arteries (long, short and anterior)
L: lacrimal artery
E: ethmoidal arteries (anterior and posterior)
S: supraorbital artery
S: supratrochlear artery (frontal artery)
I: internal palpebral artery

Which of the branches of the ophthalmic artery supply the nose?
Anterior and posterior ethmoidal
Passage of the anterior choroidal artery
Posterior- along optic tract, choroid fissue at medial edge of temporal lobe
Branches to optic tract, uncus, amygdala, hippocampus, globus pallidus, lateral geniculate body and ventral part of the internal capsule.
Terminal branches→ choroid plexus in temporal horn anastomosing with posterior choroidal

Neurological deficit with ICA occlusion
Blindness of ipsilateral eye
Loss of contralateral half of visual field.
Contralateral hemiplegia and hemianopia with global aphasia
Neurological deficit with anterior choroidal occlusion
Contralateral hemiplegia and sensory abnormalities (internal capsule)
Contralateral homonymous heminaopia
Passage of MCA
Runs deep in the lateral sulcus between the frontal and temporal lobes


What branch of the ACA is given off just proximal to the AComm?
Medial striate artery (recurrent artery of Heubner)

What is supplied by the recurrent artery of Heubner?
aka Medial striate artery
Penetrates the anterior perforated substance to supply the ventral part of the head of the caudate nucleus, the adjacent part of the putamen and the anterior limb and genu of the internal capsule

Branches of the ACA
Ascends in the longitudinal fissure and bends backwards around the genu of the corpus callosum.
Supplies medial part of the orbital sufrace of frontal lobe including the olfactory bulb and tract.
Continues along the upper surface of the corpus callosum as the pericallosal artery and a large branch, the callosmarginal artery follows the cingulate sulcus.

Why does a unilateral MCA lesion cause no loss of hearing even though the auditory cortex is including in the MCA territory?
Due to the bilateral cortical projection.
Why does a lesion in the internal capsule not cause aphasia?
Because the connections of the language areas with the contralateral hemisphere are intact.
Features of anterior cerebral artery occlusion
Contralateral paralysis of leg and perineum.
May have urinary incontinence caused by inadequate perineal sensation.
May also have contralateral facial weakness due to corticofugal fibres.
Infarction of olfactory lobe may cause anosmia.
Mental confusion and dysphasia may result ?due to loss of function in the prefrontal cortex, cingulate gyrus and SMA
How does the vertebral artery enter the subarachnoid sapce?
Pierces the atlanto-occpital membrane then the arachnoid and dura mater at the foramen magenum
Whence does the single anterior spinal artery arise?
From a contribution from each vertebral artery.
From what do the posterior spinal arteries arise
Either as a branch of the vertebral or PICA.
Passage of PICA
Irregular course between medulla and cerebellum.
Branches of PICA
Distributed to posterior parts of the cerebellar hemisphere, inferior vermis, central nuclei of cerebellum and choroid plexus of the fourth ventricle.
There are also important medullary branches to the dorsolateral medulla
Under which layer of meninges do the CNS arteries lie?
Subarachnoid
Where do the vertebral arteries unite?
Pontomedullary junction
What structures are supplied by PCA?
Midbrain
Occipital lobe
Where does the anterior spinal artery originate?
Anterior to the medulla from two contributory branches of the vertebral artery.
Structures supplied by PICA
Lateral medulla
Posteroinferior cerebellum

What proportion of SC is supplied by ASA?
Anterior 2/3rds
How do segmental arteries enter the SC?
Via the spinal nerves, divide into anterior and posterior radicular arteries passing down the ventral and dorsal spinal roots.
How many posterior spinal arteries are there?
What is their origin?
2
Vertebral arteries or from PICA
What are 3 important contributory arterial systems to the segmental supply of the spinal cord?
Deep cervical artery
Intercostal
Lumbar
What is the most important contributory artery to the anterior spinal artery?
Artery of Adamkiewicz/Great Medullary Artery (direct supply from the aorta).
Mostly on left.
What are the two watershed zones of the spinal cord supplied by the anterior spinal artery?
What is the clinical significance of this?
T4
L1
These are the most common areas to infarct in the compromise of anterior spinal arterial supply.
What is the watershed zone of the posterior spinal arteries?
T1-3.
Origin of AICA
Variable, arises from basilar or vetrebral
Structures supplied by AICA
Anteroinferior cerebellum
Lateral pons

Which artery supplies the middle ear?
Origin?
Labyrinthine artery
Basilar or from AICA

SCA supplies
Superior cerebellum.
Portion of midbrain.

Where does the internal carotid pierce dura mater to enter the subarachnoid space?
Medial to anterior clinoid process

Ophthalmic artery branches
DR MCLESSI
First and second last branches of the mnemonic are the terminal branches
Dorsal nasal artery
Retinal artery
Muscular artery
Cilliary arteres (long, short and anterior)
Lacrimal artery
Ethmoidal arteries (anterior and posterior)
Supraorbital artery
Supratrochlear artery
Internal palpebral artery

Which blood vessel is the most common site for Berry aneurysm?
AComm
C1 carotid
Cervical portion
From the carotid bifurcation to the carotid foramen of the skull base
No branches

C2 carotid
Petrous portion
From the carotid foramen to the posterior edge of the foramen lacerum in the carotid canal.
One branch:
Caroticotympanic artery
[vidian artery occasionally]

Branches of the second carotid segment
Petrous portion
Caroticotympanic and vidian
C3 carotid
Lacerum segment
Small portion where the ICA passes over the foramen lacerum
C4 carotid
Cavernous segment
From the foramen lacerum (petrolingual ligament) to the anterior clinoid process
Multiple branches including
Meningohypophyseal trunk
Inferolateral trunk.
Medial trunk or McConnell’s artery goes to the capsule of the pituitary gland.
Branches of the fourth segment of the carotid
Cavernous segment
Meningohypophyseal trunk
Inferolateral trunk
McConnel’s capsular artery
(small capsular arteries to the wall of the cavernous sinus)

Branches of the meningohypophyseal trunk
Tentorial artery (AKA Bernasconi and Cassinari artery)
Dorsal meningeal artery
Inferior hypophyseal artery

Bernasconi and Cassinari artery
Tentorial artery
Branch of the meningohypophyseal trunk (D)

McConnell’s artery
They arise from the medial wall of the cavernous ICA distal to both the meningohypophyseal trunk and the inferolateral trunk.

C5 carotid
Clinoid segment
Between the proximal and distal dural rings

Branches of the external carotid
Superior thyroid
Ascending pharyngeal
Lingual
Facial
Occipital
Posterior auricular
Maxillary
Superficial temporal
C6 carotid
Ophthalmic segment
From the distal dural ring to the PComm
Two important branches:
Ophthalmic
Superior hypophyseal

Important branches of the sixth segment of the internal carotid
Ophthalmic segment
Ophthalmic artery
Superior hypophyseal artery
C7 carotid
Communicating segment
From the PComm artery to the bifurcation of the ICA into the ACA and the MCA
Branches are
PComm
Anterior choroidal

Branches of the 7th segment of the carotid
PComm
Anterior choroidal
Classification of the ACA
Can be grossly divided into precommunicating and postcommunicating segments based on its relation to the AComm
Can also be divided into 5 segments
A1 ACA
From the bifurcation to the AComm

A2 ACA
From the AComm to the junction of the rostrum and genu of the corpus callosum
Recurrent artery of Heubner may arise from either the junction of A1/2 or from A1 or A2
A2 segment normally gives off the frontopolar and the orbitofrontal artery

A3 of the ACA
Travels around the genu of the corpus callosum and becomes A4 after turning sharply.
Highly variable branches including the callosomarginal which may divide into the anterior, middle and posterior internal frontal arteries. These 3 arteries may also arise directly from the A3 segment.
The pericallosal artery may also arise from the segment or be a direct continuation of the ACA

A4/5 segments of ACA
Run over the body of the corpus callosum
Separated from each other via a vertical line running over the callosal surface
A4 gives off the paralobular central artery.
A5 gives off superior and inferior internal parietal arteries.

M1 of the MCA
The sphenoidal or horizontal segment
From the origin of the MCA to the bifurcation into a superior and inferior trunk.
Lateral lenticulostriate arteries arise from this segment

M2 of the MCA
Insular segment
Runs in the depth of the Sylvian fissure from its bifurcation.

M3 of the MCA
Opercular segment
From the depths of the Sylvian fissure on its posterior segment to the surface

M4 of the MCA
Cortical segment
Starts at the surface of the Sylvian fissure and gives off multiple branches travelling to the cortical surfaces of the cerebral hemispheres.

V1 of the vertebral artery
Subclavian to C6 transverse foramina
V2 of the vertebral artery
Vertebral segment
From C6 to C2
V3 of the vertebral artery
Extradural segment, from C2 to the foramen magnum
V4 of the vertebral artery
Intradural segment
From its entry to the dura of the foramen magnum to its unification with the contralateral vertebral artery and formation of the basilar
Branches of basilar
AICA
Labyrinthine
Pontine
SCA
P1 of the PCA
Precommunicating
From the bifurcation of the basilar to the junction of the PComm
Gives off multiple perforators to the diencephalon and anterolateral midbrain.

P2 of the PCA
Ambient segment
From PComm to posterior edge of the midbrain.
Lateral posterior choroidal artery and thalamogeniculate arteries

P3 of PCA
Quadrigeminal segment
From the posterior edge of the midbrain to the calcarine anterior limit of the calcarine fissure.
Posterior temporal artery, Parieto-occipital and calcarine artery, Posterior pericallosal artery

Two main superficial veins of the cranium
Superior vein of Trolard
Inferior vein of Labbe
Vein of Trolard
Drains from Sylvian fissure to SSS

Vein of Labbe
Drains from Sylvian fissure to transverse sinus
What are the major deep veins
Internal cerebral vein
Vein of Galen
Basal vein of Rosenthal

Internal cerebral vein
Receives the thalamostriate vein at the foramen of Monro and the septal vein
Basal vein of Rosenthal
Drains the base of the brain from the anterior perforated substance to the internal cerebral vein
Joins to form the vein of Galen

Vein of Galen
Formed by the internal cerebral and basal vein of Rosenthal
Joins with ISS to form straight sinus
Function of BBB
Stabilises internal environment of CNS
Protects CNS from endogenous and exogenous toxins and bacteria
Maintains concentration of neurotransmitters
Types of capillaries
Continuous (tight)
Fenestrated
Sinusoidal

What are the special features of the endothelial cells of neurovascular capillaries
Tight junctions between cells
Demonstrate very low levels of transcellular vesicular transport
No fenestrations
P-glycoproteins (ATP dependent pumps that pump lipid-soluble toxins out of CNS)
Basement membrane (contains pericytes)
Astrocyte foot processes against BM release substances which stimulate endothelial cells to produce occludins and other factors that promote type junctions
What substances cannot cross BBB?
Plasma proteins or plasma protein-bound substances
Highly charged molecules/polar/water-soluble molecules
Toxic substances
Which substances can cross the BBB?
Small molecules
Non-polar/lipid soluble molecules
Specific facilitative transporters (e.g. for glucose)
Which glucose transporters are present in CNS capillaries?
GLUT-1
(independent of insulin)
Components of the blood-CSF barrier?
Fenestrated endothelial cells without tight junctions.
BM of endothelial cells
BM of ependymal cells
Specialised ependymal cells (choroidal epithelial cells) which possess tight junctions

Under which circumstances is BBB disrupted?
Physiological:
Circumventricular organs
Neonates
Pathological:
Trauma
Inflammation/infection
Irradiation
Neoplasm
Hypertensive encephalopathy
High altitude (hypoxia can damage BBB)
All cause vasogenic oedema
What is bounded superiorly by the anterior commissure and inferiorly by the optic chiasm?
Lamina terminalis of the third ventricle
What are the periventricular organs?
Sensory:
Vascular organ of lamina terminalis (OVLT)
Area postrema
Subfornical organ
Median eminence
Secretory:
Posterior pituitary
Subcommissural organ
Pineal gland

What is the embryological significance of the lamina terminalis?
Derives from cranial neuropore
What is the arrangement of capillary endothelial lining at the periventricular organs?
Fenestrated (except subcommissural)
Why is the BBB broken in the median eminence?
To allow carriage of regulatory peptides from hypothalamus to pituitary
Why is the BBB broken at the OVLT?
Senses presence of peptides in blood including AngII and IL-1
Contains osmoreceptors
Interacts with supra-optic nucleus promoting the release of ADH

Function of subfornical organ?
Contains neurones sensitive to AngII
Acts as thirst centre and centre for regulation of fluid balance.
Connected with OVLT
Why is BBB broken at pineal gland
To allow secretion of melatonin into blood
Function of subcommissural organ?
Not clearly established
No fenestrated capillaries
In other species secretes glycoproteins into the ventricular system to form Resiner’s fibres/threads which keep the system open. ?Aetiology of congenital cerebral aqueduct stenosis

Location of area postrema
Two centres
Lower portion of floor of fourth ventricle
Function of area postrema
Emetogenic substances
Connected with dorsal nucleus of vagus and nucleus of tractus solitarius which together are called the dorsal vagal triangle
Known as chemoreceptor trigger zone
At what point is the PCA joined by the PComm?
The lateral margin of the interpeduncular cistern.
Structures supplied by the PCA?
Posterior part of the cerebral hemispheres
Thalamus
Midbrain
Other deep structures including the choroid plexus and walls as lateral and third ventricles
P1 Segment of PCA
Precommunicating segments
Extends from the basilar bifurcation to the junction with the PCommA
What is meant by a fetal P1 configuration
In which the P1 has a smaller diameter than the PComA and the PCA arises predominantly from the carotid artery
In what proportion of hemispheres is a fetal PComm arrangement found?
1/3rd of hemispheres
Relationship of the oculomotor to PCommA
Passes below and slightly lateral to the PComA if a normal configuration is present.
If a fetal pattern is present, P1 is longer and the nerve courses beneath or medial to the communicating artery

What are the 4 constant branches of P1?
Thalamoperforating artery (enters the brain through the posterior perforated substance)
Medial posterior choroidal artery
Branch to quadrigeminal plate
Rami to the cerebral peduncle and mesencephalic tegmentum.
Extent of the P2 segment
Begins at the PCommA
Lies within the crural and ambient cisterns, terminating laterally to the posterior edge of the midbrain.
Divided into an anterior and posterior part
Anterior part of P2
P2A or crural/peduncular segment as it courses around the cerebral peduncle in the crural cistern
Posterior part of P2
P2P or ambient/lateral mesencephalic segment because it courses lateral to the midbrain in the ambient cistern
Passage of P2A
Begins at PCommA and courses between the cerebral peduncle and uncus that forms the medial and lateral walls of the crural cistern and inferior to the optic tract and basal vein that crosses the roof of the cistern to enter the proximal portion of the ambient cistern

Passage of P2P
Commences at the posterior edge of the cerebral peduncle at the junction of the crural and ambient cisterns.
Passes between the lateral midbrain and the parahippocampal and dentate gyri which form the medial and lateral wallls of the ambient cistern below the optic tract, basal vein and geniculate bodies.

P3 Segment
Quadrigeminal segment
Proceeds posteriorly from the posterior edge of the lateral surface of the midbrain and ambient cistern to reach the lateral part of the quadrigeminal cistern and ends at the anterior limit of the calcarine fissure.

What is the quadrigeminal point
The point where the PCAs from each side are nearest is referred to as the collicular or quadrigeminal point.
P4 Segment
Includes the cortical branches.
Begins at the anterior end of the calcarine sulcus
What are the 3 categories of PCA branches
Central perforating branches to the di and mesencephalon
Ventricular branches to the choroid plexus and walls of the lateral and third ventricles and adjacent structures
Cerebral branches to the cortex and splenium of the corpus callosum
Perforating branches of the PCA
Divided into direct and circumflex arteries
Direct:
Thalamoperforating arteries (P1)
Thalamogeniculate and peduncular perforating arteries (P2)

Circumflex arteries of the PCA
Encircle the brainstem for a variable distance before entering the diencephalon and mesencephalon and divided into long and short groups dependent on how far they course around the brainstem.
Through which transverse foramen of the cervical vertebra does the vertebral artery pass?
C1-6
How many segments of the vertebral artery are there?
4 segments
Extent of V1
Prevertebral.
From its origin at the subclavian artery to C6
Extent of V2
Vertebral segment
Runs within the transverse foramen from C6 to C2
Extent of V3
Extradural segment
From C2 to the foramen magnum
Extent of V4?
From the entry into the dura of the foramen magnum until its jucntion with the contralateral vertebral artery where it forms the basilar.
What are the collateral branches of the vertebral arteries?
Anterior meningeal artery
Posterior meningeal artery
Posterior spinal artery
Branches of the vertebral artery
ASA
PICA
Features of the anterior spinal artery?
Formed from two branches oiginating from each of the VAs prior to their union as the basilar artery.
Runs in the surface of the anterior median fissure of the spinal cord, supplies blood to the anterior 2/3rds.
Features of PICA
Supplies the posterolateral medulla, the fourthh ventricle and the posteroinferior cerebellar hemispheres

Level of termination of the basilar artery?
Interpeduncular cistern
Branches of the basilar
AICA
Labyrinthine
Pontine
SCA
Number of segments of PCA?
4 segments
Extent of P1
Pre-communicating segment
From the bifurcation of the basilar artery to the junction of PComm
Gives off multiple perforators to the thalamus, hypothalamus, subthalamus and the anterolateral segment of the midbrain.

Extent of P2
Ambient segment
From the junction of the PComm to the posterior edge of the midbrain.
Some of the PCA branches at this segment are the lateral posterior choroidal artery and thalamogeniculate arteries.

Extent of the P3 segment
Quadrigeminal segment
From the posterior edge of the midbrain to the anterior limit of the calcarine fissure.
The branches of this segment supply the posteroinferior temporal lobe (posterior temporal artery)
Occipital lobe (parieto-occipital artery and calcarine artery
And the posterior segment of the corpus callosum (posterior pericallosal artery)

Extent of P4 segment
Terminal segment
Anatomy of Alexia without Agraphia
Cerebral hemispheric infarction
Left occipital region plus splenium of the corpus callosum.
Due to infarction of Callosal branches
Pure word blindness, can write but not read
Alexia without agraphia
Signs and symptoms of alexia without agraphia
Can write but not read
May have contralateral homonymous hemianopia
Balint Syndrome
Oculomotor ataxia
Bilateral loss of voluntary but not reflex eye movements
Bilateral optic ataxia- poor visual-motor coordination
Asimultagnosia- inability to understand visual objects
Anatomy of Balint syndrome
Bilateral parietal occpital lobe infarct due to bilateral PCA stroke
Claude Syndrome
Ipsilateral CN3
Contralateral ataxia of arm and leg.
Marked ataxia differentiates from Benedikt’s
Anatomy of Claude syndrome
Contralateral ataxia due to infarction of midbrain tegmentum secondary to PCA occlusion.
May also have ipsilateral oculomotor palsy with contralateral tremor and ataxia
Anton Syndrome
Cortical blindness
Bilateral visual loss
Unawareness or denial of blindness

Anatomy of Anton syndrome
Bilateral PCA occlusion or top of basilar occlusion
Due to bilateral occipital lobe involvement
Unilateral Occpital PCA stroke
Conralateral homonymous heminaopia with macular sparing
Due to infarction of occipital and infero-medial temporal lobes
Dejerine Roussy Syndrome
Thalamic pain syndrome
Due to thalamoperforator branch infarction
Causes hemisensory loss- all modalities then development of intractable hemi-body pain

Weber Syndrome
Basal midbrain stroke
Contralateral weakness of arm and leg due to corticospinal tract involvelent
Ipsilateral CN3 palsy

Benedikt syndrome
Paramedian midbrain syndrome
Ipsilateral CN3 palsy
Cerebellar ataxia with choreoathetotic movements (red nucleus)
May involve contralateral hemiparesis due to involvement of corticospinal tract.

Artery of Davidoff and Scheter
The artery of Davidoff and Schechter (ADS) is a dural branch that arises from the posterior cerebral artery and supplies the falcotentorial junction. It is usually not identified on angiography except when enlarged in the setting of dural AVFs, meningiomas, or, rarely, cerebellar tumours

Normal CBF
50ml/100g/min
Vertebral artery dominance
Left side 50%
Right side 25%
Non-dominance 25%
The left vertebral artery arises from the aorta in what proportion of patients?
5%
What proportion of the population have a hypoplastic vertebral artery?
40%
Structures supplied by superior thyroid artery
Larynx and upper thyroid
Anastomoses with the thyrocervical trunk
Structures supplied by and anastomoses:
Ascending pharyngeal
Nasopharynx, oropharynx and middle ear
CNs IX-XI
Meninges
Vertebral artery branches
Structures supplied by and anastomoses:
Lingual artery
Tongue and floor of mouth
Structures supplied by and anastomoses:
Facial artery
Face, palate, lips
Angular branch of the facial artery anastomoses with the orbital branch of the ophthalmic

Structures supplied by and anastomoses:
Occipital artery
Posterior scalp, upper cervical musculature, posterior fossa and meninges
Anastomoses with the vertebral artery
Structures supplied by and anastomoses:
Posterior auricular artery
Pinna, EAC, scalp
Structures supplied by and anastomoses:
Superficial temporal
Scalp and ear
Structures supplied by and anastomoses:
Maxillary
Deep face
Gives off MMA and accessory meningeal
Anastomoses with inferolateral trunk, ophthalmic and petrous carotid via ethmoidal and vidian branches
Subsegmentation of the intracavernous ICA
Ascending portion (entrance into the cranium to the genu)
Posterior genu (between C5 and C3 segments)
Horizontal portion (between the genu)
Anterior genu
Remainder of intracavernous ICA segment
Location of the cervical ICA
Larger than ECA
Located in the lateral pharyngeal space
Initially posterolateral to the ECA but becomes medial to enter the carotid canal anteromedial to the IJV

Location of the petrous ICA
Enters the caroid canal of petrous temporal bone
Lies behind the eustachian tube

Segments of petrous ICA
Vertical sgment (10mm)
Horiztonal (20mm), exits the petrous apex superior to the foramen filled lacerum
Caroticotympanic artery
Embryonic hyoid artery remnant
Arises near the genu of the petrous ICA passes superiorly
When aberrant can cause retrotympanic pulsatile mass
Anastomoses with inferior tympanic artery (ECA)
Supplies middle and inner ear

MHT branches
Italian artery (tentorial)
Inferior hypophyseal
Dorsal meningeal

Structures supplied by:
Tentorial artery
Tentorium
Structures supplied by:
Inferior hypophyseal artery
Neurohypophysis

Structures supplied by:
Dorsal meningeal artery
CN VI and clivus

Structures supplied by:
Inferolateral trunk
Inferolateral cavernous sinus wall, tentorium, CN III, IV, VI, V ganglion
Anastomoses with the maxillary artery and MMA

Medial trunk of cavernous sinus
Present in 28% of the population
Anterior capsular artery- medially over sellar roof
Inferior capsular artery- inferomedially to the sellar floor
Supplies anterior and inferior pituitary
Ophthalmic artery branches
DR MCLESSI
D: dorsal nasal artery
R: (central) retinal artery
M: muscular artery
C: ciliary arteries (long, short and anterior)
L: lacrimal artery
E: ethmoidal arteries (anterior and posterior)
S: supraorbital artery
S: supratrochlear artery (frontal artery)
I: internal palpebral artery
Aneurysms of ophthalmic artery
Arise from the superior wall of the ICA distal to the OA origin, project superiorly and may abut the CN II
Structures supplied by the superior hypophyseal artery
Adenohypophysis and the infundibulum
Tuber cinereum
Inferior surface of the optic chiasm and CN II
Course of the SHA
Arises from the posteromedial ophthalmic ICA beneath CN II

SHA aneurysms
Project inferiorly and medially
Course of PCommA
Arises from the posterior wall of the ICA and passes posterolaterally above CN III to join the P1 segment of PCA

Structures supplied by PComm
Posterior hypothalamus
Anterior thalamus
STN
Posterior limb of internal capsule via seven perforators that are equally distributed along the vessel length and course superomedially to their targets
PComm Aneurysms
Normally arise from the posterior wall of the ICA immediately distal to the PComm origin and point towards CNIII
PComm is typically inferomedial to the aneurysm and the anterior choroidal artery is superior lateral
What proportion of population has variant PComm?
Categories of PComm variation
50%
Absent or hypoplastic
Fetal
Infundibulum
What proportion of the population have an absent or hypoplastic PComm?
30%
What proportion of population have fetal PComm
20%
(PComm A same diameter as P1)
PComm infundibulum
Funnel-shaped dilatation of the PComm <2mm

PComm arising from dome of a pyramidal dilatation
Differentiated from aneurysm does which does not come off tip
Structures supplied by the medial proximal striate branches of A1
1-12 perforators
Optic nerve and chiasm
Anterior hypothalamus
Septum pellucidum
Anterior commissure
Pillars of the fornix and the anteroinferior striatum
NB Medial DISTAL lenticulostriate artery= recurrent artery of Heubner
AComm perforators
2 or more arise from the AComm to supply:
Infundibulum
Chiasm
Subcallosal area
Preoptic hypothalamus
Include the subcallosal artery and medial artery of the corpus callosum

AComm aneurysms
Usually arise at the point where the dominant A1 bifurcates and point towards the contralateral side
Branches of A2
Heubner (A1)
Orbitofrontal artery
Frontopolar artery
Anterior internal frontal artery

Branches of A3
Callosomarginal artery
Pericallosal artery
Middle internal frontal artery
Posterior internal frontal artery
Paracentral artery
Superior parietal artery
Inferior parietal artery

What proportion of the population have an MCA bifurcation
50%
What proportion of the population have an MCA trifurcation
25%
Branches of M1
Uncal artery
Temporopolar artery
Anterior temporal artery
Lateral lenticulostriate arteries

Structures supplied by the callosomarginal artery
Cingulate gyrus and paracentral lobule
Second most common ACA site for aneurysms?
Junction of the pericallosal artery with callosomarginal
Aneurysms usually point distally
Structures supplied by pericallosal artery
Medial parietal cortex and precuneus
Structures supplied by middle internal frontal artery
Medial frontal cortex
Structures supplied by posterior internal frontal artery
Medial posterior frontal cortex
Structures supplied by paracentral artery?
Medial cortex around the central sulcus
Structures supplied by superior parietal artery
Medial superior parietal lobe
Structures supplied by inferior parietal artery
Medial inferior parietal lobe
Features of the uncal artery
More frequently arises from the distal ICA than proximal M1
Supplies uncus and underlying white matter
Structures supplied by temporopolar artery?
Anterior pole of superior, middle and inferior temporal gyri

Structures supplied by anterior temporal artery?
Anterior pole of the superior, middle and inferior temporal gyri

Structures supplied by lateral lenticulostriate arteries
2-15 perforators from M1
Substantia innominata
Anterior commissure
Putamen
Globus pallidus
Superior half of internal capsule
Head and body of caudate
Branches of the superior trunk of M2
Orbitofrontal branch
Prefrontal branch
Precentral branch
Central branch
Anterior parietal branch

Structures supplied by
Orbitofrontal branch of the superior trunk of M2

Orbital portion of middle and inferior frontal gyri and the inferior pars orbitalis

Structures supplied by
Prefrontal branch

Branch of superior M2 trunk
Superior pars orbitalis
Pars triangularis
Anterior pars opercularis
Most of the middle frontal gyrus

Structures supplied by
Precentral branch

Posterior pars opercularis
Middle frontal gyrus and inferior and middle portions of the precentral gyrus

Structures supplied by
Central branch

Superior trunk M2
Superior postcentral gyrus, upper central sulcus, anterior part of the inferior parietal lobule and the anteroinferior region of the superior parietal lobule

Structures supplied by
Anterior parietal branch

M2 superior trunk
Superior parietal lobule

Branches of the inferior trunk of M2

Posterior parietal branch
Angular branch
Temporo-occipital branch
Posterotemporal branch
Middle temporal branch

Structures supplied by the posterior parietal branch of inferior trunk of M2

Posterosuperior and inferior parietal lobule and inferior supramarginal gyrus

Structures supplied by angular branch of the inferior M2 trunk

Posterior aspect of the superior temporal gyrus
Portions of the supramarginal and angular gyri and the superior aspect of the lateral occipital gyrus

What is the largest cortical branch of the MCA?

Angular branch

Structures supplied by the temporo-occipital branch of inferior M2 trunk

Posterior half of the superior temporal gyrus, the posterior extreme of the middle and inferior temporal gyri
Inferior lateral occipital gyrus

Structures supplied by the posterotemporal branch of inferior M2 trunk

Middle and posterior portion of the superior temporal gyrus
Posterior 1/3 of middle temporal gyrus
Posterior extreme of the inferior temporal gyrus

Structures supplied by the middle temporal branch of inferior M2 trunk

Superior temporal gyrus near the level of the pars trianagularis and pars opercularis
Central part of the middle temporal gyrus
Middle and posterior parts of the inferior temporal gyrus

P1 branches
Posterior thalamoperforator
Medial posterior choroidal arteries
Meningeal branches
Passage of posterior thalamoperforators
From basilar and P1
Pass through the posterior perforated substance behind the mamillary bodies to supply the thalamus, hypothalamus, subthalamus and midbrain
Structures supplied by the medial posterior choroidal arteries
Travels anteromedially along the roof of the third ventricle
Supplies the midbrain tectum, posterior thalamus, pineal gland and tela choroidea of the third ventricle

Structures supplied by meningeal branches of P1
Tentorium and falx
Branches of P2 segment
Lateral posterior choroidal
Thalamogeniculate
Cortical branches
Lateral posterior choroidal artery
Main branch of P2
Courses over the pulvinar and through the choroidal fissure
Supplies the posterior portion of the thalamus and choroid plexus (temporal horn and atrium)

Thalamogeniculate branches
Supply MGN, LGN, pulvinar
Superior colliculus
Crus cerebri
Structures supplied by cortical branches of P2
Inferior temporal artery
P3 branches
Posterior temporal artery
Internal occipital artery
Parieto-occipital artery
Calcarine artery
Posterior pericallosal artery

Posterior temporal artery
P3 branch
Posterior temporal lobe
Occipitotemporal and lingual gyri
Anterior temporal artery branch travels to the inferior temporal lobe to supply the inferior cortex
Anastomoses with MCA

Parieto-occipital artery
P3 branch
Located in the parieto-occipital sulcus
Supplies the posterior 1/3rd of the medial hemispheres
Cuneus
Precuneus
Superior occipital gyrus and precentral and superior parietal lobules
Anastomoses with ACA

Calcarine artery
P3
Located in calcarine sulcus
Supplies the occipital pole and visual cortex
Posterior pericallosal artery
P3
Supplies splenium of the corpus callosum

Origin of Anterior choroidal artery
Arises from the posteromedial surface of the ICA immediately distal to the origin of the PCommA
Course of the anterior choroidal
Cisternal (ambient)
and
Intraventricular segments
Enters the choroidal fissure at the plexal point- temporal horn of the lateral ventricle

Where does the anterior choroidal artery enter the lateral ventricle?
At the plexal point (AKA inferior choroidal point)
Structures supplied by the anterior choroidal artery
Via perforators
Choroid of the lateral ventricles (esp temporal horn)
Hippocampus, amygdala, uncus
GP, caudate tail, putamen
VL nucleus of the thalamus
Posterior limb of the internal capsule
Inferior optic chiasm, optic tract, LGN, optic radiation

Historical significance of anterior choroidal artery
Previously sacrificed to treat Parkinson’s disease.
Likely reduced tremor due to reduction in blood supply to the VL thalamus
What proportion of individuals have a complete CoW
25%
Categories of penetrating arteries of the CoW
Anteromedial
Anterolateral
Posteromedial
Posterolateral

Anteromedial perforators
Arise from ACA and AComm including RAH
Enter the anterior perforated substance to supply anterior hypothalamus, preoptic nucleus and supraoptic nucleus
Posteromedial perforators
Arise from proximal PCA and PCommA
Supply the hypophysis, infundibulum and tuberal hypothalamus
Thalamoperforating arteries which supply the mammillary bodies, subthalamus and midbrain
Anterolateral perforators
Striate arteries from proximal MCA and recurrent artery of Heubner
Enter the anterior perforated substance
Supply the head of caudate, lateral GP, putamen, claustrum, IC and EC
Posterolateral perforators
Arise from PCA (thalamogeniculate arteries)
Supply caudal thalamus (geniculate bodies, pulvinar, lateral nucleus and lateral ventral nucleus)
In what proportion of patients does the vertebral artery enter the foramen transversarium at C6?
90%
Anastomoses of the vertebral
ECA
Thyrocervical
Costocervical
Branches of the vertebral
Extracranial:
- Segmental spinal branches
- Muscular branch
- Meningeal branch
Anterior and posterior spinal arteries
PICA
Muscular branch of vertebral artery
Anastomoses with muscular branch of ECA (ascending pharyngeal, thyrocervical and costocervical)

Meningeal branches of vertebral
Anterior meningeal branch-> FM dura
Posterior meningeal branch-> falx and post fossa dura
Blood supply of the falx cerebelli
2 vertebral, 2 ECA
Posterior meningeal branches
PICA
Occipital
Ascending pharyngeal
Structures supplied by posterior spinal arteries at the cervicomedullary junction
Gracile and cuneate fasciculi
Inferior cerebellar peduncle
Structures supplied by the anterior spinal artery at the level of the cervicomedullary junction?
Pyramid
Medial lemniscus
MLF
Olive
Vagal and hypoglossal nuclei
What proportion of vertebral arteries terminate as the PICA
1-25%
Structures supplied by PICA
Choroid of fourth
Posterior lateral medulla
Tonsils
Vermis
Posteroinferior cerebellar hemispheres
Relation of AICA to CNs
Crosses CN VI and the cerebellopontine angle cistern to the IAC
Passes anterior and inferior to CNs VII and VIII
Branches of AICA
Internal auditory artery
Recurrent perforating artery
Subarcuate artery

Blood supply:
Striatum
Mainly lenticulostriate arteries of MCA
Rostrally- recurrent artery of Heubner
Caudally: Ant Choroidal
Blood supply:
IC
Anterior limb: ACA (RAH, MCA lateral lenticulostriate)
Genu: ICA perforators, MCA lenticulostiate
Posterior limb: Ant choroidal and PComm

Blood supply:
Thalamus
PCA by way of perforators: thalamoperforators, thalmogeniculate arteries, medial posterior choroidal arteries
Rostrally: PComm A (anterior thalamoperforating arteries)
[and basilar bifurcation perforators)

Diploic veins
Communicate with the scalp, meningeal veins and dural sinuses
Meningeal veins
Epidural vessels of the dura which follow meningeal arteries and drain into dural sinuses or into the extracranial pterygoid venous plexus
What proportion of people have a dominant right transverse sinus
60%
ISS drains predominantly into?
Left transverse sinus

Venous phase DSA
- Septal vein.
- Anterior caudate vein.
- Terminal vein.
- Thalamostriate vein.
- Atrial vein.
- Basal vein of Rosenthal.
- Vein of Galen.
- Internal cerebral vein.
- Venous angle.

Superficial middle cerebral veins
Course along sylvian fissure
Drain into cavernous sinus or superior Trolard (Top) or Labbe (lower)
Vein of Trolard
Drains from Sylvian fissure to SSS
Vein of Labbe
Drains from Sylvian fissure to transverse sinus
Internal cerebral veins
Location
Tela choroidea in the roof of the third ventricle
Extend from the foramen of Monro, over the thalamus and posteriorly to the quadrigeminal cistern where they unite to form the vein of Galen

Formation of the internal cerebral veins
Formed by the union of the:
Thalamostriate
Choroidal
Septal
Epithalamic
Lateral ventricular

Basal vein of Rosenthal
Drains the anterior and medial temporal lobe
Passes posterosuperiorly through the ambient cistern
Joins the internal cerebral vein to form the vein of Galen

Vein of Galen formation
Receives both internal cerebral veins
Basal veins of Rosenthal
Occipital veins
Posterior callosal vein
Travels under the splenium and merges with the inferior sagittal sinus to form the straight sinus
What are the ICA-ECA anastomoses?
Ascending pharyngeal-> VA
Ascending pharyngeal -> ICA via petrous and cavernous branches
Facial artery-> ICA via the angular branch of facial artery to orbital branch of ophthalmic
Occipital artery-> vertebral
Posterior auricular artery-> ICA via the stylomastoid artery
Maxillary artery-> ICA
What are the maxillary artery to ICA anastomoses?
MMA to ethmoidal branch of ophthalmic
Temporal branches to ophthalmic
Infraorbital artery to ophthalmic
Artery of foramen rotundum to ILT
Accessory meningeal artery to ILT
Vidian artery to petrous ICA
Pharyngeal artery to cavernous ICA
MMA to primitive hyoid branch of the ICA

Primitive hyoid branch of the ICA
Known as persistent stapedial artery
When present, the foramen spinosum is small or absent with an enlarged geniculate fossa

What are the persistent fetal carotid-basilar and carotid-vertebral anastomoses?
Persistent trigeminal
Persistent acoustic
Persistent hypoglossal
Proatlantal intersegmental
Rate of primitive trigeminal artery persistence
0.5% of angiograms
Connections of primitive trigeminal artery
Connects cavernous ICA with embryonic dorsal longitudinal neural arteries
Arises from ICA just proximal to the cavernous sinus meningohypophyseal trunk
Curves medially to join the basilar between the SCA and AIC

Associations of primitive trigeminal artery
Associated with hypoplastic PCommA and basilar and vertebral arteries proximal to anastomosis
Increased frequency of AVMs and aneurysms (25%)
Connections of the persistent otic artery
Connects petrous ICA via internal auditory meatus to the basilar artery
Connects petrous ICA with embryonic dorsal longitudinal neural arteries
Very rare

Which is the first fetal carotid-basilar communication to involute?
Otic
What is the second most frequent persistent fetal circulation?
Primitive hypoglossal
Rate of persistent primitive hypoglossal
0.3%
Connections of primitive hypoglossal?
Connects cervical ICA with embryonic dorsal longitudinal arteries
Arises from the cervical ICA and connects to the basilar artery through the hypoglossal canal

Associations with persistent hypoglossal arteries
Typically bilateral hypoplastic vertebral arteries thus this may be the main supply to the brain stem and cerebellum
Proatlantal intersegmental artery
Connects ECA or cervical ICA with embryonic dorsal longitudinal neural arteries
Suboccipital anastomosis between cervical ICA and vertebral artery
Courses between the arch of C1 and the occiput

Features of spinal radicular ateries
Derived from segmental vessels from the aorta which include the ascending cervical, deep cervical, intercostal, lumbar and sacral arteries
Pass through the intervertebral foramina to divide into anterior and posterior radicular arteries
What happens to the anterior and posterior divisions of the spinal segmental arteries?
Anterior ramus of the segmental artery supplies the cord whilst the posterior ramus supplies the DRG and nerve roots via anterior and posterior radicular branches.

Where does the artery of Adamkiewicz arise?
75% from T9-12
80% arise from the left

Outline the blood supply to spinal cord segments
In each segment, the anterior spinal artery gives off several sulcal arteries that course posteriorly in the anterior median fissure.
Typically each artery enters one half of the SC to supply the anterior, base of posterior and anterior and lateral funiculi (2/3rds total) in that half
Paired posterior spinal arteries provide supply to the posterior 1/3rd including the posterior horn and funiculus
All three spinal arteries contribute numerous anastomosing vasocorona on the pial surface which in turn send branches to the peripheries.

Posterior spinal artery supplies
Posterior one-third of the spinal cord
Anterior spinal artery
Supplies anterior two-thirds of the SC
Joint at the medulla to enter the anterior median fissure as a single artery (anterior median spinal artery)
Anterior radicular spinal arteries
2-17 arteries: cervical 6, thoracic 2-4, lumbar 1-2
Artery of Adamkiewicz
Posterior radicular arteries
10-23 arteries
Divide at the posterolateral spinal cord surface and joins the paired posterior spinal arteries
Posterior arterial system of the spinal cord
Paired posterior spinal arteries form a leptomeningeal peirmedullary network that anastomoses with the anterior system, most prominently at the conus where the anastomotic loop is located
Blood from the posterior medullary arteries flows centripetally in the perforating branches from the leptomeningeal system to the posterior columns and horns

Anterior arterial system of the spine
Single midline artery that feeds into the anterior medullary artery in the anterior median fissure
Flows centrifugally via penetrating branches to the anterior and intermediate gray and via pial radial network to anterior and lateral WM
Blood supply of cervical SC
Vertebral artery
PICA
Ascending cervical artery (thyrocervical trunk)
Deep cervical (costocervical)
Blood supply of the thoracic SC
Thyrocervical and costocervical trunk
Intercostal artery (T3-11)
Subcostal artery (T12)
Bloody supply to the lumbar SC
Lumbar artery (aorta L4-5)
Blood supply to sacral SC
Lateral sacral artery (IIA) supplies sacral neural elements
Middle sacral artery
The aorta and iliac arteries send branches to the thoracolumbar spine
Where is the SC most vulnerable to ischaemia?
At transitional regions where the arterial supply is derived from more than one source
T1-4
and
L1
Also vulnerable are areas between the anterior and posterior medullary arteries (between the intermiedate and dorsal horns and lateral and posterior fasciculi)
Describe the venous drainage of the SC
Highly variable
Both anterior and posterior spinal veins lie adjacent to the spinal arteries which eventually drain into the intervertebral veins exiting the SC via intervertebral foramina
Anterior and posterior radicular vein
Rhotons microsurgical segments of the supraclinoidal ICA
Ophthalmic segment
Communicating segment
Choroidal segment
Anterior falx artery
Arises from the anterior ethmoidal branch of the ophthalmic artery and perforates the cribriform plate
Ascending in the falx parallel to the inner table of the skull

Endoscopic landmarks for ethmoidal arteries

AEA passes through foramen 24mm posterior to anterior lacrimal ridge
PEA 12mm from anterior foramen
Optic canal 6mm posterior to the PEA
In what proportion is the CoW intact?
18%
Routes for venous drainage of cavernous sinus dAVFs
6 routes
SOV + IOV-> ocular symptoms
Inferior petrosal sinus-> basilar/ptyergoid plexus-> bruit and CN deficit
Superior petrosal sinus-> bruit
Sphenoparietal sinus-> superficial middle vein and cortical reflux with haemorrhage
Cerebellar drainage into petrous vein -> ataxia and haemorrhage
Deep drainage into middle cerebral and uncal vein-> haemorrhage


Persistent hypoglossal artery
What is the venous complex that surrounds the petrous segment of the ICA/
ICA venous plexus of Rektorzik
It is believed that the plexus serves to dampen arterial pulsations of the carotid artery, thereby reducing osseous transmission of sound to the cochlea
The plexus appears thickest between the carotid and the point closest to the cochlea, supporting this hypothesis
Gibo classification of Carotid
C1-4
Cervical
Petrous
Cavernous
Supraclinoid
Median prosencephalic vein of Markowski
A precursor to the vein of Galen
Before birth, its anterior portion regresses with the formation of the internal cerebral veins and its posterior portion persists as the vein of Galen

Veins of Breschet
Diploic intraosseous veins

Sinus of Breschet
Sphenoparietal venous sinus

Vein of Vesalius
Sphenoidal emissary foramen gives passage to a small vein (vein of Vesalius) that connects the pterygoid plexus with the cavernous sinus. The importance of this passage lies in the fact that an infected thrombus from an extracranial source may reach the cavernous sinus

Petro-occipital vein of Trolard
The inferior petro-occipital vein is located immediately inferior to the petro-occipital suture and provides a communication between the internal carotid artery venous plexus of Rektorzik, or less commonly the cavernous sinus, anteromedially and the jugular bulb, or less commonly the inferior petrosal sinus, posterolaterally

Hypoglossal plexus of Trolard
The venous plexus of hypoglossal canal ( also known as plexus venosus canalis nervi hypoglossi (TA), circellus venosus hypoglossi and rete canalis hypoglossi– is a small venous plexus around the hypoglossal nerve that connects with the occipital sinus, the inferior petrosal sinus and the internal jugular vein.
Vein of Dandy
Superior petrosal vein
usually formed by the convergence of multiple tributaries to form a single large vein that empties into the superior petrosal sinus.





Superior M2 syndrome
Contralateral paralysis of face and arm
Contralateral sensory loss
Expressive dysphasia
Inferior M2 syndrome
Contralateral HH
Receptive dysphasia
Impaired 2 point discrimination
Artery of Salmon
A muscular branch from the third segment of the vertebral artery in the suboccipital triangle
Supplies blood to the suboccipital muscles
Found in 48%
(A)

Artery of Wollschlaeger and Wollschlaeger
Branch of the superior cerebellar artery and becomes enlarged and elongated in vascular tumours and tentorial vascular malformations
(B)

Which vessel is C?

Artery of Davidoff/Schecter
Arteria termatica of Wilder
Formation of one artery from the fusion of A2, AKA azygos artery of the pericallosal artery
F

Etymology azygos
Zygos means yoked or paired
i.e. unpaired
Structures A-G

A- Meningohypophyseal trunk
B- Lateral tentorial artery
C- Marginal tentorial artery of Bernasconi-Cassinari
D- Inferior hypophyseal artery
E- Hypophyseal branches
F- Inferior clival branch

Structures H-P

H- Lateral branch of lateral clival
I- medial branch of medial clival artery
J- jugular branches of ascending pharyngeal
K- Clival branches of Ascending pharyngeal
L- Petrosquamosal branches
M- foramen lacerum branch of the middle meningeal artery
O- Occipital artery
P- basilar.

Which vessel runs alongside superior petrosal sinus
Lateral branch of lateral clival artery
Which vessel runs alongside inferior petrosal sinus
Medial branch of lateral clival artery
MHT on MR/CT or angio
Discernible MHT usually means some kind of pathology
Would not normally see on 1.5T
If MHT visible, consider proceeding to DSA ?dAVF if no other cause identified,
What is denoted by the arrow

On MR T1 post contrast there is a hyperintense petroclival homogenously enhancing extra-axial lesion- likely meningioma
The arrow demonstrates the pathologically hypertrophied MHT branch supplying tumour.

Red- inferior hypophyseal
White- pituitary blush
Purple- marginal tentorial
Blue- ILT


Large vessel traversing pituitary fossa= primitive maxillary artery which arise in the context of carotid agenesis involving petrous segment
Can be reconstituted via contralateral through primitive maxillary anastomosis (fetal inferior hypophyseal arteries)
Vascular territory

PICA
Vascular territory

AICA
Vascular territory

SCA
Vascular territory






Vascular territory
































Sylvian point
Most posterior M2 branch
Marks anterior margin of atrium
Inferior choroidal point
Location where anterior choroidal enters the temporal horn of the lateral ventricle (posterior to the posterior aspect of uncus)

In which medial temporal lobe sulcus does the anterior choroidal artery run?
Arises medial to semilunar gyrus and runs in semiannular sulcus before entering the temporal horn of lateral ventricle at the inferior choroidal point

Relationship of SCA to 3,4,5
Runs below 3 + 4 and above 5
It may have two trunks- superior and inferior

Maxillary artery anatomy
Overview
Origin behind the neck of the mandible
Divided into three portions by relation to lateral pterygoid
First- mandibular (posterior to lateral pterygoid, 5 branches)
Second- pterygoid/muscular (within lateral pterygoid, 5 branches)
Third- pterygopalatine (anterior to lateral pterygoid, 6 including terminal branch)

Maxillary artery branches
First part
Mandibular
Deep auricular- squamotympanic fissure
Anterior tympanic artery- squamotympanic fissure
MMA- foramen spinosum
Accessory meningeal artery- foramen ovale
Inferior alveolar artery (artery to mylohyoid)- mandibular foramen

Maxillary artery branches
Second part
Muscular/pterygoid part
Anterior, middle and posterior deep temporal branches
Pterygoid
Masseteric
Buccinator

Maxillary artery branches
Third part
Pterygopalatine
Posterior superior alveolar artery
Infraorbital artery (infraorbital fissure)
Artery of pterygoid canal
Pharyngeal artery (palatovaginal canal)
Greater palatine artery
Sphenopalatine artery (sphenopalatine foramen)

FV=
Tranmsmit

FV= foramen vesalius
Transmits sphenoidal emmissary veins (vein of Vesalius) from pterygoid plexus to cavernous sinus.
Components of Rhoton’s neurovascular complex
Brainstem
Cerebellar pedcunles
Fissures
Arteries
Cerebellar surfaces
Components of Rhoton’s neurovascular complex
Fissures between brainstem and cerebellum
Cerebellomesencephalic
Cerebellopontine
Cerebellomedullary
Components of Rhoton’s neurovascular complex
Cerebellar surfaces
Tentorial
Petrosal
Suboccipital
Upper neurovascular complex
SCA
Midbrain
Cerebellomesencephalic fissure
Superior cerebellar peducnle
Tentorial cerebellar surface
III, IV, V

Relationship of SCA to upper neurovascular complex
SCA arises in front of the midbrain
Passes below 3,4 and above 5
Reaches cerebellomesencephalic fissure where it runs over the superior peduncle and supplies tentorial surface of cerebellum
Middle neurovascular complex
AICA
Pons
Middle cerebellar peduncle
Cerebellopontine fissure
Petrosal cerebellar surface
6, 7, 8

Lower neruovascular complex
PICA
Medulla
Inferior cerebellar peduncle
Cerebellomedullary fissure
Suboccipital cerebellar surface
9, 10, 11, 12

Origin and course of SCA
Arises anterior to midbrain below CN3 (occasionally can arise from proximal PCA and pass over CN3)
Dips caudally and encircles brainstem near pontomesencephalic junction, passing below trochlear nerve and above trigeminal
Proximal portion courses close to the tenorial edge, distal below the tentorium
Enters cerebellomesencephalic fissure where it gives off the precerebellar arteries which supply deep cerebellar white matter and dentate nucleus
Division of SCA
Divides into a rostral and caudal trunk
Structures supplied by rostral trunk of SCA
Vermian and paravermian areas
Structures supplied by the caudal trunk of SCA
Hemispheric suboccipital surface
Segments of SCA

4 segments
Anterior pontomesencephalic
Lateral pontomesencephalic
Cerebellomesencephalic
Cortical
Each may be composed of one or more trunks
SCA- anterior pontomesencephalic segment
Located between dorsum sella and upper brainstem
Begins at SCA origin and extends below CN3 to the anterolateral margin of brainstem
Lateral part is medial to the anterior half of the free tentorial edge.

SCA- lateral pontomesencephalic segment
Second segment
Begins at the anterolateral margin of brainstem
Frequently dips caudally onto the lateral side of upper pons
Caudal loop projects to root entry zone of trigeminal at midpontine level.
Trochlear passes above midportion of this segment.
Caudal loop usually carries it below the tentorial edge.
Terminates at the anterior margin of cerebellomesencephalic fissure
Basal vein and PCA above and parallel.

SCA- cerebellomesencephalic segment
Third part
Courses within cerebellomesencephalic fissure
SCA enters the shallowest part of the fissure above the trigeminal root entry zone and course medial to the tentorial edge.
Fissure progressively deepens- deepest in midline behind superior medullary velum.
SCA loops deeply and then passes upwards to the anterior edge of the tentorium.

SCA- cortical segment
Fourth and final segment
Includes branches distal to the cerebellomesencephalic fissure that pass under the tentorial edge and is distributed to the tentorial surface and if marginal branch present to the upper part of the petrosal surface.

Segments of AICA
Four
Anterior pontine segment
Lateral pontine segment
Flocculopeduncular segment
Cortical segment

AICA- anterior pontine segment
First segment
Located between clivus and belly of pons
Ends at the level of a line drawn through the long axis of the inferior olive and extending upwards on the pons
May be in contact with rootlets of abducens

AICA- lateral pontine segment
Second segment
Begins at the anterolateral margin of the pons and passes through the CPA in relation to CN 7 + 8, intimately related to the IAM, lateral recess and choroid protruding from the foramen of Luschke
Subdivisions of lateral pontine segment of AICA
Premeatal
Meatal
Postmeatal
Based on relation to the porus acousticus
Nerve-related branches of the lateral pontine segment of AICA
Labyrinth artery- CN VII, VIII, vestibulocochlear labyrinth
Recurrent perforating arteries
Subarcuate artery
AICA- Flocculopeduncular segment
Begins where artery passes flocculus to reach middle cerebellar peduncle and CP fissure
May be hidden beneath flocculus or lips of cerebellopontine fissure
AICA- cortical segment
Fourth and final part
Supplies predominantly the petrosal surface
PICA segments
5 segments
Anterior medullary
Lateral medullary
Tonsillomedullary
Telovelotonsillar
Cortical

PICA- Anterior medullary segment
First segment
Begins at PICA origin and extends past the hypoglossal rootlets to the level of a rostrocaudal line through the most prominent part of the inferior olive
If PICA arises lateral to the medulla then does not have an anterior medullary segment.
Usually passes posteriorly around or between hypoglossal rootlets

PICA- Lateral medullary segment
Begins at the most prominent portion of inferior olive and ends at the level of origin of IX, X, XI rootlets

PICA- Tonsillomedullary segment
Third segment
Begins where PICA passes posteriorly to IX, X, XI rootlets and extends medially along the posterior aspect of medulla near caudal half of tonsil
Ends where artery ascends to midlevel of medial tonsillar surface
Loop passing near the lower part of tonsil= caudal loop, can dip below the level of FM

Relationship of the caudal loop of tonsillomedullary segment of PICA and cerebellar peduncle
Generally ends above or around the level of the caudal pole of the tonsil.
Cranial to the foramen magnum generally
PICA- telovelotonsillar segment
Begins at the midportion of PICA’s ascent along the medial surface of tonsil towards the roof of fourth
Ends where PICA exits fissures between vermis, tonsil and hemisphere to reach suboccipital hemispheres
Forms cranial loop in most which is caudal to fastigium between cerebral tonsil below and tela choroidea and posterior medullary velum above
Gives rise to branches supplying tela choroidea and choroid plexus of fourth

PICA- Cortical segment
Fifth and final segment
Beigns where trunks and branches leave groove between vermis medially and tonsil and hemisphere laterally
Includes terminal cortical branches
PICA bifurcation occurs near origin of this segment.
Subclavian artery branches
VIT CD
Vertebral
Internal thoracic
Thyrocervical
Costocervical
Dorsal scapular

Thyrocervical trunk branches
ISTA
I: inferior thyroid artery
S: suprascapular artery
T: transverse cervical artery
A: ascending cervical artery

Costocervical trunk branches
SD
Supreme intercostal
Deep cervical artery

Post-AComm clipping
Patient presenting with anterograde and retrograde amnesia, cognitive disturbance and confabulation

Subcallosal artery infarct
Perforator from AComm complex
Goblet sign

Capsular artery of McConnell
Difference between duplicated and accessory MCA
Duplicated- second MCA arises from ICA
Accessory- second MCA from ACA
Describe the vascular territories of the thalamus
Four vascular territories
Chiefly supplied by small perforating end-arteries from the PCA
Anterior: polar arteries, PComm
Paramedian: thalamoperforating branches from the P1 segment of the PCA (either unilateral or bilateral)
Lateral: Thalamogeniculate artery from P2
Posterior: Medial posterior choroidal artery or posterior branch of lateral posterior choroidal artery
May also receive additional blood supply form the anterior choroidal artery

Draw the blood supply of the thalamus

What constitutesthe carotid siphon
The lower half of the S is formed predominantly by the intracavernous portion
Upper half by the supraclinoid portion
Why is the anterior choroidal seen before PComm when exposing the carotid above the ophthalmic artery?
AChA seen first even though it is more distal as:
C6/7 passes upwards posterolateral placing AChA origin lateral from the midline
AChA commonly arise further laterally from the posterior wall
AChA pursues a more lateral course
Infundibular arteries
Group of arteries originating from PComm and distributed to the infundibulum
Fewer in number than superior hypophyseal arteries
Which hypophyseal vessel supplies the anterior pituitary and stalk?
Superior hypophyseal
What proportion of ophthalmic arteries arise within the cavernous sinus
8%
Location of ophthalmic artery origin
Below optic nerve in supraclinoid region
Above dural roof of cavernous sinus
Pass anterolaterally below optic nerve to enter optic canal
What can be done to improve ophthalmic artery exposure?
Removal of anterior clinoid process and roof of the optic canal
Incising falciform process (a thin fold of dura that extends medially from ACP)
Premamillary artery
AKA Anterior thalamoperforator/ Polar arteries
Largest branch arising from PComm
Enters floor of third in front of mamillary body
Supplies posterior hypothalamus, anterior thalamus, posteiror limb of IC and subthalamus
Segments of anterior choroidal
Cisternal
Plexal
Cisternal segment of AChA
Origin to the choroidal fissure
Divided at the anterior margin into a proximal and distal segment
Plexal segment of AChA
One or more branches that pass through choroidal fissure to branch and enter the choroid plexus of the temporal horn
Basis of AChA clipping for Parkinsonism
Coopers tore the AChA whilst performing a pedunculotomy and had to clip it and terminate the operation
There was a disappearance of tremor and rigidity with preservation of voluntary motor function
Thought to be due to ischaemic necrosis of GP
Coopers technique of AChA clipping for Parkinsonism
2 clips, one at origin and one 1.5cm from origin distal to pallidal branches
Distal clip thought to prevent retrogade filling
Coopers AChA clipping outcomes
Good relief of tremor and rigidity
20% morbidity, 6% mortality
Hemiplegia, partial aphasia, HH
Several patients developed memory loss and confusion
Not uncommon for patients to remain somnolent for up to 10 days
M1 and M2 boundary
M1 becomes M2 at the genu
The M1 can be subdivided into a pre and post bifurcation part
Boundary of M2 and M3
M2 starts at the genu where the MCA passes over the limen insula
Terminates at the circular sulcus of insula
Boundary of M3 and M4
M3 segment begins at circular surface of insula and ends at the surface of the Sylvian fissure
What proportion of lenticulostriate perforators are prebifurcation
Around 80%
Remainder are post bifurcation
Few may arise from proximal M2
The earlier the bifurcation, the higher the number of post-bifurcation lenticulostriates
Divisions of lenticulostriate arteries
Medial- tends not to branch before entering anterior perforated substance
Intermediate- complex arborised array with one large feeder
Lateral
What proportion of MCAs bifgurcate
80%
What proportion of MCAs trifurcate
12$
Categorisation of MCA bifurfcations
Equal bifurcation
Superior trunk dominant
Inferior trunk dominant
Based on diameter and size of cortical area supplied
How to differentiate between accessory MCA and recurrent artery of Heubner?
The recurrent artery of Heubner enters the anterior perforated substance
Accessory MCA sends branches to but courses laterally to anterior perforated substance
Sensorimotor hempiplegia
Without receptive dysphasia
Superior trunk occlusion
Receptive aphasia in absence of hemiplegia
Inferior MCA trunk occlusion
Pericallosal artery vs Callosomarginal
Pericallosal arises at the ACommA
Callosomarginal arises from pericallosal to course along cingulate sulcus, can arise just distal to AComm or at any site along pericallosal
Pericallosal origin is not the junction with callosomarginal branch as the callosomarginal is variably present
What is the only anaotmic variant tat correlates with loation of cerebral aneurysm?
A1 hypoplasia, found in 85% of AComm aneurysm
Most common site in the CoW for hypoplasia
Crural monoplegia
Lower limb monoplegia
Short pericallosal artery
Short arteries arising from pericallosal artery and perforating directly into corpus callosum
Can also supply septum, anterior pillars of fornix and commissure
Long pericallosal arteries
Long vessels also arising from pericallosal and course parallel between it and the surface of the corpus callosum
Precallosal artery
Infrequently occuring Acomm or A2 branch that passes upwards like a long callosal artery between pericallosal and lamina terminalis sending branches to anterior diencephalon


