Chapter 3 - Periapical Lesions Flashcards
3 types of pulpitis
Reversible
Irreversible
Chronic Hyperplastic

Chronic Hyperplastic Pulpitis
Inflammation causes the pulpal tissue to bulge up and out into the crown
4 most likely Periapical Pathologies
Periapical Granuloma
Apical periodontal cyst
Periapical Abscess
Bone scar
What is the most common and most likely periapical pathology?
Periapical granuloma
What is the LEAST common periapical pathology?
Bone Scar
Sequelae of Periapical Pathology (4)
Sinus Tract
Osteomyelitis
Condensing Osteitis
Cellulitis

Parulis“Gum Boil”
Intraoral sinus tract exit - on oral mucosa
Osteomyelitis
Chronic or acute infection of the bone - bone marrow
Bacterial infection
Results in:
* Expanding lytic destruction
* Suppuration
* Sequestra Formation - bone pieces floating in the infection

Condensing Osteitis
What is the earliest change in the periodontium resulting from periapical pathology.
Periapical Granuloma
Most common periapical pathosis
Chronically inflamed granulation tissue - nonvital tooth
Usually asymptomatic
Histology - plasma cells and lymphocytes
Phoenix Abscess
Secondary acute inflammatory changes within a periapicla granuloma
Clinical Presentation of Periapical Granuloma
Asymptomatic
Tooth not typically mobile
Usually not sensitive to percussion
Does not respond to thermal or electrical pulp testing
Periapical Granuloma Treatment
Conventional endodontic treatment
Surgical endodontic treatment
Extraction
Periapical Periodontal Cyst
* Periapical cyst or Radicular Cyst*
Inflammatory stimulation of epithelium in the area – Rests of Malassez
Radiograhically –> Slow growth, punched out border
Histology –> Spiderweb pattern, epithelium lined
Patterns:
* Classical
* Lateral Apical Periodontal
* Residual apicl periodontal cyst

Classical Pattern of Periodontal Cyst
Lesion surrounds the root tip

Lateral Apical Periodontal Cyst
Lesion lateral to root tip
Lateral canal

Residual Apical Periodontal Cyst
Toot was extracted but the cyst remains
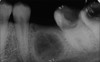
Periapical abscess
Acute inflammatory cells at the apex of a nonvital tooth
Symptomatic or asymptomatic
Histology –> large accumulation of inflammation
Earlies manifestation with widening of the PDL - when pulpal involvement
Periapical abscess treatment
Endo Treatment
Extraction
Pain Killers
Periapical Scar
Defect created by periapical inflammatory lesions may fill with DENSE collagenous tissue
Common – Following surgical endodontic therapy
When facial and lingual cortical plates have been lost
Histology –> Collagen (all pink, no blue), Fibroblasts
RADIO-Translucent

Sequelae or Periapical Pathology (4)
Sinus Tract
Osteomyelitis
Cellulitis
Condensing Osteitis
Sinus Tract
Pus dissects through the bone – destroying the bone
Perforates the cortical plate of bone extending into soft tissue
Follows the path of least resistance
Drains purulent material – may be intermittent drainage
Location of tract depends on involved tooth and path of least resistance

Parulis (Gum boil)
Intraoral sinus tract exiting through oral mucosa
Hole with red halo
Pustule (large pimple)
*Fistula*








