27: Vascular Flashcards
Which vessel is diseased in foot claudication?
Distal superficial femoral artery or popliteal disease
[Symptoms occur one level below occlusion]
[UpToDate: Classic claudication is characterized by leg pain that is consistently reproduced with exercise and relieved with rest. The degree of symptoms of claudication depends upon the severity of stenosis, the collateral circulation, and the vigor of exercise. Patients with claudication can present with buttock, hip, thigh, calf, or foot pain, alone or in combination. The usual relationships between pain location and corresponding anatomic site of arterial occlusive disease can be summarized as follows:
- Buttock and hip: Aortoiliac disease
- Thigh: Aortoiliac or common femoral artery
- Upper two-thirds of the calf: Superficial femoral artery
- Lower one-third of the calf: Popliteal artery
- Foot claudication: Tibial or peroneal artery]

During abdominal aortic aneurysm repair, reimplantation of the inferior mesenteric artery should be performed if the backpressure is below what level?
Less than 40 mmHg (IE poor backbleeding)
[Other reasons for implantation include previous colonic surgery, stenosis at the superior mesenteric artery, or flow to left colon appears inadequate]
[UpToDate: Colonic ischemia is uncommon following elective AAA repair. The adequacy of perfusion to the left colon should always be assessed prior to completion of the case, and the inferior mesenteric artery should be reimplanted if there is any question of bowel viability.
In general, if backbleeding from the orifice of the inferior mesenteric artery (IMA) within the aneurysm sac is vigorous, indicating adequate collateral flow, or the vessel is occluded (no backbleeding), reimplantation of the IMA into the aortic graft is not necessary. In one trial, patients with a confirmed patent IMA were randomly assigned to replantation or ligation. There was no significant difference in the incidence of ischemic colitis between the groups (replanted: 6 patients, ligated: 10 patients). However, in patients with prior colon resection or reduced inflow to one or both internal iliac arteries, reimplantation of the inferior mesenteric artery is appropriate.]
A herald bleed (episode of GI hemorrage, often accompanied by abdominal pain, which may precede by hours to weeks a catastrophic GI hemorrage) with hematemesis and then blood per rectum in a patient with a history of abdominal aortic surgery is worrisome for what?
Aortoenteric fistula
[Graft erodes into 3rd or 4th portion of duodenum near proximal suture line]
[UpToDate: Early diagnosis of aortoenteric fistula (AEF) associated with bleeding relies upon recognition of the typical “herald bleed,” which is an episode of seemingly self-limited gastrointestinal bleeding that precedes a later catastrophic episode of hemorrhage. AEF must be kept in mind as a possible etiology of massive gastrointestinal bleeding in patients with prior aortic interventions, no matter how long since the intervention.
The classic triad of gastrointestinal bleeding, abdominal pain, and palpable mass occurs in only 6% to 12% of patients found to have AEFs. When the etiology of AEF is an abdominal aortic aneurysm (AAA), a mass can be palpated in 25% to 70%. The unreliability of clinical findings underscores the need to maintain a high index of suspicion in all cases of gastrointestinal bleeding, especially upper gastrointestinal tract bleeding. Further complicating the matter is the fact that patients with AAA/aortic intervention can have gastrointestinal bleeding due to other causes.
The very low incidence of this condition in the general population puts AEF low in the differential diagnosis of gastrointestinal bleeding.]

95% of patients with aortic dissection present with what?
Severe hypertension
[UpToDate: Hypertension is present in 70% of type B dissections, but only in 25% to 35% of type A dissections. The presence of hypotension complicating a type B dissection is rare, seen in less than 5% of patients, and usually implies rupture of the aorta. By contrast, hypotension may be present in 25% of dissections that involve the ascending aorta, potentially as a result of aortic valve disruption leading to severe aortic regurgitation and/or extravasation into the pericardial space leading to cardiac tamponade. Malperfusion of brachiocephalic vessels by the dissection may falsely depress brachial cuff pressures, usually by involving the left subclavian artery origin in the type B dissection patient.]

What are pulse volume recordings used for?
Used to find significant occlusion and at what level
[UpToDate: Modern vascular testing machines use air plethysmography to measure volume changes within the limb, in conjunction with segmental limb pressure measurement. The same pressure cuffs are used for each test.
Cuffs are placed and inflated, one at a time, to a constant standard pressure. Volume changes in the limb segment beneath the cuff are reflected as changes in pressure within the cuff, which is detected by a pressure transducer and converted to an electrical signal to produce an analog pressure pulse contour known as a pulse volume recording (PVR).
A normal PVR waveform is composed of a systolic upstroke with a sharp systolic peak followed by a downstroke that contains a prominent dicrotic notch. Alterations in the pulse volume contour and amplitude indicate proximal arterial obstruction. The degree of these changes reflects disease severity. Mild disease is characterized by loss of the dicrotic notch and an outward “bowing” of the downstroke of the waveform. With severe disease, the amplitude of the waveform is blunted. Pulse volume recordings are most useful in detecting disease in calcified vessels which tend to yield falsely elevated pressure measurements.
Since the absolute amplitude of plethysmographic recordings is influenced by cardiac output and vasomotor tone, interpretation of these measurements should be limited to the comparison of one extremity to the other in the same patient and not between patients. The dicrotic notch may be absent in normal arteries in the presence of low resistance, such as after exercise.]

What are the 3 most commonly affected arteries in fibromuscular dysplasia?
- Renal
- Carotid
- Iliac
[UpToDate: The most frequently involved arteries are the renal and internal carotid arteries, followed by the vertebral, visceral, and external iliac arteries.
Patients with fibromuscular dysplasia (FMD) have involvement of the renal arteries approximately 75% to 80% of the time and involvement of the extracranial cerebrovascular arteries (eg, carotid and vertebral arteries) approximately 75% of the time. Approximately two-thirds of patients have multiple arteries involved.
Among adults, FMD is more common among females. In most large series, approximately 90% of cases are in women. There does not appear to be a female predominance among children with FMD.
In the past, it was believed that FMD was a disease of young women. However, older individuals account for a large proportion of affected patients in several cohorts. As an example, in the United States FMD Registry, the mean age at diagnosis was 52 years, with a range of 5 to 86 years.]

Venous ulcers of what size often heal without surgery?
Less than 3cm
What is the treatment for varicose veins?
Sclerotherapy
[UpToDate: Chemical ablation involves the introduction of an irritant agent into the vein, causing endothelial damage by either detergent or osmotic action. Liquid sclerosant preparations are typically used to treat telangiectasias, reticular veins, and small varicose veins. Ultrasound-guided sclerotherapy, with the injection of the sclerosant at the level of refluxing perforator veins, has also been used to treat the associated clusters of varicose veins. This technique has been used with good long-term results and without significant complications, but requires an experienced practitioner. Endovenous techniques can also be used to ablate perforator reflux with the use of special probes.
The choice of ablation method depends upon the size of the varicose veins, their location, and presence or absence of venous reflux. Meta-analyses comparing surgery with minimally invasive therapies (sclerotherapy, radiofrequency ablation, laser ablation) have concluded that minimally invasive therapies appear to be at least as effective as surgical excision, with long-term success rates of 78% to 84%. Postoperative pain is generally less and return to work quicker with minimally invasive therapies, compared with surgery. Minimally invasive procedures are generally associated with fewer complications. In one trial, each of the groups showed significant improvements in quality-of-life scores, and 84.3% of treated patients had improved CEAP clinical category following treatment, although vein closure rates varied at one year (highest at 88.5% for endovenous laser ablation, followed by 88.2% for conventional surgery, and 72.2% for foam sclerotherapy).
A later trial involving 798 participants with primary varicose veins compared the outcomes of foam sclerotherapy, laser, and surgery. Clinical success was similar between the groups, but successful ablation of the main trunks of the saphenous vein was less common for foam sclerotherapy compared with surgery. No significant differences were found for quality of life. The frequency of procedural complications was similar for the foam sclerotherapy and surgery groups (6% and 7%, respectively), but was lower in the laser group (1%). The frequency of serious adverse events (approximately 3%) was similar among the groups. A trial comparing saphenous vein high ligation plus phlebectomy with endovenous laser ablation reported follow-up to five years at which time there were no significant differences in rates of recurrent varicose veins or reoperation.
A review of randomized trials comparing ultrasound-guided foam sclerotherapy with endothermal ablation noted that although anatomical success appeared higher with endothermal ablation, clinical success and patient-reported outcome measures were similar. Morbidity and complication rates were very low and not significantly different. Ultrasound-guided foam sclerotherapy was less expensive than endothermal ablation.]
Late swelling following a lower extremity bypass is concerning for what?
Deep vein thrombosis
[UpToDate: We agree with all major society guidelines which recommend long-term aspirin therapy or clopidogrel for all patients with peripheral artery disease.
The 2012 American College of Chest Physicians (ACCP) guideline on antithrombotic therapy for peripheral artery occlusive disease made the following recommendations for the use of antithrombotic agents in patients undergoing infrainguinal vascular surgery:
- Aspirin therapy (75 to 100 mg/day) should begin preoperatively and continue indefinitely in all patients undergoing infrainguinal bypass (to prevent graft failure) or arterial reconstruction. Clopidogrel (clopidogrel 75 mg daily) is an alternative to aspirin in those who cannot take aspirin.
- In patients undergoing below-knee bypass graft surgery with prosthetic grafts, clopidogrel plus aspirin is recommended for a period of one year. For all other patients single rather than dual antiplatelet therapy should be give.]
What is the 1st branch of the external carotid artery?
Superior thyroid artery
[Wikipedia: As the artery travels upwards, it supplies:
- Superior thyroid artery, arising from its anterior aspect
- Ascending pharyngeal artery - arising from medial, or deep, aspect
- Lingual artery - arising from its anterior aspect
- Facial artery - arise from its anterior aspect
- Occipital artery - arising from its posterior aspect
- Posterior auricular artery - arising from posterior aspect
The external carotid artery terminates as two branches:
- Maxillary artery
- Superficial temporal artery]

What are the indications for repair of descending aortic aneurysm?
- Greater than 5.5 cm if endovascular repair is possible
- Greater than 6.5cm if open repair is needed
[UpToDate: For most patients with asymptomatic TAA, we use the following thresholds as criteria for elective repair.
Descending TAA:
- For most average-sized adults: diameter of 6 to 7 cm
- Patient with high surgical risk: diameter ≥7 cm
- For patients with genetically-mediated conditions (syndromic or nonsyndromic), a lower diameter (eg, 5.0 to 6.0 cm depending on the condition) or aortic size index is suggested as an indicator for repair.
- For smaller patients, including many women, a diameter greater than twice the diameter of the nonaneurysmal aorta (normal segment) or aortic size index can be used.
- Rapid expansion ≥10 mm per year for aneurysms <5 cm in diameter. For patients with associated genetically-mediated conditions, a lower expansion rate (eg, >5 mm/year) is suggested as an indicator for repair.]

What is the treatment for median arcuate ligament syndrome?
- Transect median arcuate ligament
- May need arterial reconstruction
[UpToDate: Surgical treatment is the only option for patients with persistent abdominal pain and demonstrated celiac artery compression on imaging studies, since there are no medical therapies. Surgical options include celiac artery decompression alone or surgical decompression combined with celiac artery angioplasty/stent or vascular reconstruction. Surgical decompression involves division of the fibers of the median arcuate ligament and celiac plexus (celiac ganglionectomy). Laparoscopic and robotic-assisted laparoscopic approaches have been reported. With these techniques, a laparoscopic ultrasound probe can be used to confirm patency of the celiac artery once it has been decompressed. Depending on the results of the procedure, secondary celiac stenting can be performed. Regardless of the approach, decompression of the celiac axis does not always relieve symptoms.
The optimal surgical approach remains debated. Celiac artery reconstruction appears to be more commonly performed during open surgical celiac decompression procedures, but a significant number of patients have relief of their symptoms with decompression alone. In a study that compared open and laparoscopic approaches, the distribution of treatments was as follows:
- Open decompression 279/400 (70%)
- With arterial reconstruction (n = 70)
- Without arterial reconstruction (n = 201)
- Laparoscopic decompression 121/400 (30%)
- With percutaneous mesenteric angioplasty (n = 16)
- With open angioplasty/bypass (n = 2)
Celiac artery decompression can be combined with balloon angioplasty/stenting of the celiac, surgical angioplasty, or interposition grafting using an open (eg, open decompression/angioplasty or bypass) or hybrid approach (eg, laparoscopic decompression, percutaneous angioplasty). A primary percutaneous approach without celiac artery decompression is not an option since the underlying problem is extrinsic compression (not intrinsic disease such as that caused by atherosclerosis).]

Which leg is more commonly involved in deep venous thrombosis?
Left leg (Longer left iliac vein)
Following dissection in the groin, what can you do to identify the lymphatic channels supplying a lymphocele if having trouble locating it?
Inject isosulfan blue dye into the foot
What is the second most common pathogen responsible for a mycotic abdominal aneurysms?
Staphylococcus
[#1 is salmonella]
[UpToDate: Blood cultures are positive in 50% to 85% of cases. Organisms have been isolated from aneurysmal tissue in up to 76% of patients. In one case series, multiple organisms were isolated in 8%, and no pathogen was identified in 25% of cases.
Although bacteriologic patterns continue to evolve over time, the organisms with the greatest affinity for the arterial wall, Staphylococcus spp and Salmonella spp, remain the most common. Staphylococcus aureus is the most common pathogen reported in 28% to 71% of cases. In several reports of infected aneurysms, methicillin-resistant S. aureus (MRSA) predominates. In one series of preexisting aneurysms, Staphylococcus epidermidis was the most prevalent organism. Infected aneurysm due to vancomycin-intermediate S. aureus (VISA) has also been described.
Salmonella is reported in 15% to 24% of cases. The diseased aorta appears to be vulnerable to Salmonella, and this pathogen is frequently isolated in infected aneurysms due to bacteremic seeding of atherosclerotic plaque.
Streptococcus pneumoniae was a frequent etiology of infected aneurysms in the pre-antibiotic era but became rare with the advent of penicillin; however, S. pneumoniae may be reemerging as a cause of infected aneurysms.
Other gram-negative organisms are also associated with bacteremic seeding. In one study, although gram-positive organisms predominated, gram-negative organisms were seen in 35% of cases. In this study, gram-negative infections were associated with a higher incidence of aneurysm rupture (84% vs 10%) and mortality (84% vs 50%) compared with gram-positive organisms.
Less common causes of infected aneurysm include Treponema pallidum and Mycobacterium spp. Syphilis (T. pallidum) once caused up to 50% of infected aneurysms. Tuberculosis is a rare cause of infected aneurysms and is most often due to erosion of periaortic lymph nodes into the aortic wall. One review of cases of infected aneurysm caused by Mycobacterium tuberculosis found only 41 cases between 1945 and 1999.]
What percent of patients with abdominal aortic aneurysm rupture die if they reach the hospital alive?
50%
[UpToDate: The mortality associated with ruptured AAA may be as high as 90% when patients who die at home or upon arrival to the hospital are taken into account. In spite of obvious improvements in pre-hospital care, cardiovascular anesthesia, and critical care, surgical mortality following open repair of ruptured AAA has changed very little, remaining about 30% to 50%. Although endovascular aneurysm repair may improve survival following AAA rupture, this has not been definitively established.]

Diarrhea (especially bloody diarrhea) following an abdominal aortic aneurysm repair is worrisome for what?
Ischemic colitis
[UpToDate: Bowel ischemia can affect the small or large intestine. Acute mesenteric ischemia is rare with infrarenal AAA repair. Colonic ischemia is more likely to occur following open repair of ruptured AAA, for which the incidence is between 7% and 27% compared with 0.6% to 13% for elective AAA repair. The incidence varies greatly depending upon the diagnostic algorithm to detect it. When bowel ischemia complicates AAA repair, mortality is increased.
The majority of patients do not have symptoms and only 30% will have bloody diarrhea. Patients with full thickness ischemia are treated with colon resection. The diagnosis and management of colon ischemia is discussed elsewhere.]
Ankle-brachial index (ABI) can be very inaccurate in patients with which condition?
Diabetes
[This is secondary to incompressibility of vessels. Often have to rely on doppler waveforms in these patients]
[UpToDate: The toe-brachial index (TBI) is a more reliable indicator of limb perfusion in patients with diabetes because the small vessels of the toes are frequently spared from medial calcification.
The TBI is obtained by placing a pneumatic cuff on one of the toes. The great toe is usually chosen but in the face of amputation the second or other toe is used. A photo-electrode is placed on the end of the toe to obtain a photoplethysmographic (PPG) arterial waveform using infrared light. The infrared light is transmitted into the superficial layers of the skin and the reflected portion is received by a photosensor within the photo-electrode. The signal is proportional to the quantity of red blood cells in the cutaneous circulation.
Analogous to the ankle and wrist pressure measurements, the toe cuff is inflated until the PPG waveform flattens and then the cuff is slowly deflated. The systolic pressure is recorded at the point in which the baseline waveform is re-established. The ratio of the recorded toe systolic pressure to the higher of the two brachial pressures gives the TBI.
A pressure gradient of 20 to 30 mmHg normally exists between the ankle and the toe, and thus, a normal toe-brachial index is 0.7 to 0.8. An absolute toe pressure >30 mmHg is favorable for wound healing, although toe pressures >45 to 55 mmHg may be required for healing in patients with diabetes. Toe pressures are useful to define perfusion at the level of the foot, especially in patients with incompressible vessels, but they provide no indication of the site of occlusive disease. In addition to measuring toe systolic pressures, the toe Doppler arterial waveforms should also be evaluated.]
What is migrating thrombophlebitis associated with?
Pancreatic cancer
[UpToDate: Unexplained superficial thrombophlebitis, which may be migratory (classic Trousseau’s syndrome), is sometimes present and reflects the hypercoagulable state that frequently accompanies pancreatic cancer. There is a particularly high incidence of thromboembolic events (both venous and arterial), particularly in the setting of advanced disease, and clinicians should maintain a high index of suspicion. Multiple arterial emboli resulting from nonbacterial thrombotic endocarditis may occasionally be the presenting sign of a pancreatic cancer. Thromboembolic complications occur more commonly in patients with tumors arising in the tail or body of the pancreas.]
What is the treatment of nonocclusive mesenteric ischemia?
- Volume resuscitation
- Catheter-directed nitroglycerin can increase visceral blood flow
- Also need to increase cardiac output (dobutamine)
- Resection of infarcted bowel if present
[UpToDate: The treatment of nonocclusive mesenteric ischemia focuses on removing inciting factors (vasoconstrictive medications), treating underlying causes (heart failure, sepsis), hemodynamic support and monitoring, and intraarterial infusion of vasodilators, if necessary.]

Which protein is defective in Marfan syndrome?
Fibrillin (connective tissue elastic fiber)
[UpToDate: Marfan syndrome (MFS) is a highly variable systemic tissue disorder with clinical characteristics similar to a variety of other hereditary disorders from which it should be distinguished. MFS is almost exclusively inherited in an autosomal dominant manner, although rare case reports have described recessive fibrillin 1 gene (FBN1) mutations. While most individuals with MFS have an affected parent, 25% or more of probands have MFS as the result of a de novo mutation.
Most patients with the typical Marfan phenotype harbor mutations involving the gene (FBN1) encoding the connective tissue protein fibrillin-1. However, FBN1 mutations also cause a wide range of milder phenotypes that often show at least some overlap with the classic Marfan phenotype.
In a minority of cases (less than 10%) with typical Marfan phenotype, no mutation in FBN1 is identified. Studies have suggested that at least some of these cases are due to a complete allele deletion, more complex rearrangements, or alterations in regulatory sequences involving the FBN1 gene. In some of these individuals with atypical presentations reminiscent of MFS, an inactivating mutation in a gene encoding for transforming growth factor-beta receptor (TGFBR) may be responsible.]
What is the treatment for a carotid body tumor?
Resection
[UpToDate: Complete surgical resection for cervical (carotid body, vagal, perithyroid) paragangliomas was historically considered the treatment of choice for cervical paragangliomas. Cure rates after complete resection of a benign carotid body tumor are 89% to 100%. Although few data are available, long-term control of disease was reported in 93% of vagal paragangliomas in a systematic review of 211 cases. Cure rates are lower in patients with regional nodal metastases (five-year survival 77% in one series from the National Cancer Database) and adjuvant RT is frequently recommended, although its benefits are unproven.
Resection of carotid body tumors is performed via a transcervical approach. Special care must be taken to avoid injury to the cranial nerves. Especially in Shamblin class III tumors, there is also the potential for injury to the common or internal carotid artery.]

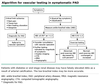
What happens to the ankle-brachial index (ABI) in patients with claudication as they go from resting to walking?
The ABI drops (ABI may be 0.9 but can drop to less than 0.6 with exercise, resulting in pain)
[UpToDate: Some patients with PAD who have a classic history of claudication, and others with atypical extremity pain, have a normal resting ABI (0.91 to 1.30). For these patients, exercise testing is indicated. Abnormal exercise ABIs support a diagnosis of PAD as the etiology of their symptoms.
The study should be performed in a vascular laboratory using a standardized exercise protocol (fixed or graded) and a motorized treadmill to ensure reproducibility of measurements of pain-free walking distance and maximal walking distance.
Exercise treadmill tests are useful for providing the most objective evidence of the magnitude of the functional limitation in patients with claudication, and can also be used to guide the response to treatment.]

What are the 3 indications for repair of an ascending aortic aneurysm?
- Acutely symptomatic
- Greater than or equal to 5.5 cm (> 5.0 cm with Marfans)
- Rapid increase in size (>0.5cm/yr)
[UpToDate: For most patients with asymptomatic thoracic aortic aneurysm (TAA), we use the following thresholds as criteria for elective repair.
Ascending TAA:
- End-diastolic aortic diameter of 5 to 6 cm or aortic size index (aortic diameter [cm] divided by body surface area [m2]) ≥2.75 cm/m2. A body surface area calculator can be found in the link.
- For patients with genetically-mediated TAAD, including syndromic conditions such as Marfan, Loeys-Dietz, vascular Ehlers-Danlos, and Turner syndromes, and nonsyndromic conditions like familial TAAD or bicuspid aortic valve, a lower diameter (eg, 4.5 to 5.0 cm depending on the condition) or aortic size index is suggested as an indicator for repair.
- Non-Turner’s patients undergoing aortic valve surgery: end-diastolic aortic diameter >4.5 cm in diameter at the time of aortic valve surgery.
- Rapid expansion ≥10 mm per year for aneurysms <5 cm in diameter. For patients with associated genetically-mediated conditions, a lower expansion rate (eg, >5 mm/year) is suggested as an indicator for repair.]