Valvular disease and HTN Flashcards
How is hypertension defined?
Systolic over 140 and diastolic over 85 on over three occasions
How to diagnose hypertension?/What investigations are done for hypertension?
If one clinic reading over 140/85, take second measurement + if this is significantly different, take third measurement
then ABPM
- Confirm Dx of HTN in people with a:
- clinic blood pressure of 140/90 mmHg or higher and
- ABPM daytime average or HBPM average of 135/85 mmHg or higher
What is malignant hypertension?
Hypertension where bp=
>200/130 mmHg
Can cause organ failure
Aetiology of hypertension?
Primary- idiopathic-> essential hypertension [most cases]
Secondary:
Endocrine- Phaeochromocytoma, Cushing’s, Conn’s, Acromegaly, Congenital adrenal hyperplasia, diabetes, hyperthyroidism, hyperparathyroidism
Renal- renal artery stenosis, chronic glomerulonephritis/pyelonephritis, polycystic kidney disease, renal failure
Cardio- coarctation of aorta
Drugs- adrenaline/sympathomimetics, steroids, OC
Pregnancy- pre eclampsia
Symptoms of hypertension?
Mostly asymptomatic
Symptoms of underlying cause in secondary hypertension: endocrine, cardiac, drug side effects, renal symptoms, signs of pregnancy
Malignant hypertension causes symptoms: headaches, blurred vision, scotoma [loss of central visual field], seizures, nausea, vomiting
Symptoms of complications of hypertension: stroke, TIA, IHD, peripheral vasc disease, retinopathy etc.
Management of hypertension?
Conservative: lifestyle changes- diet and exercise
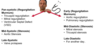
If under 55 or not Afro-Carribean:
First line: ACEi/ARB
Second line: + CCB/thiazide diuretics
Third line: ACEi + CCB + Thiazide
Fourth line: Add alpha/beta blocker or spirinolactone
If over 55 or Afro Carribean:
Start with CCB
Then add ACEi/ARB/thiazide
What are the stages of hypertension?
Stage 1= 140/90-159/99mmHg
Stage 2=160/100-179/119
Stage 3= sbp >180 or dbp>120
Hypertension
Definition
Aetiology
Diagnosis/Investigations
Symptoms and signs
Management
Monitoring
Red flags
Complications
Prognosis
Hypertension
Definition
Blood pressure higher than 140/90 mmHg
Aetiology
Either primary/essential- unknown cause
Or secondary: endocrine, renal [see other slide for more details on these two], cardio[coarctation of aorta], drugs [sympathomimetics, steroids, COCP]
Diagnosis/Investigations
Clinic blood pressure
Ambulatory blood pressure monitoring [automatically at least two measurements an hour] or Home blood pressure monitoring [twice daily for four to seven days] [if former not tolerated]
Investigations into secondary causes esp if young
Investigations for target organ damage- nine of them:
- Proteinuria + haematuria + albumin creatinine ratio
- eGFR
- Creatinine
- Electrolytes
- HbA1C
- Lipid profile- HDL and total cholesterol
- Fundocopy
- ECG
- CV risk score
Symptoms and signs
Asymptomatic mostly
Unless:
Symptoms of underlying cause in secondary HTN/ Symptoms of complications
or
Malignant hypertension: neuro ish symptoms- headaches, blurred vision, scotoma [central visual field loss], nausea, vomiting
Management
- See pics
Conservative: Lifestyle changes
Medical if: Persistent stage 2 HTN or Stage 1 HTN + less than eighty years + one of: target organ damage/CVD risk of >10%/renal disease/CVD/diabetes
Consider frailty and effects of multimorbidity in > eighty years
Monitoring
Regular check up- clinic BP measurement
Consider ABPM/HBPM - if white coat hypertension or masked hypertension
Monitor sitting and standing BP if: >eighty years / T2DM / postural hypotension symptoms
Target BP
< eighty years old
Target clinic BP: <140/90, home BP: <135/85
> eighty years old
Add 10 to target systolic bp:
Clinic BP: <150/90, home BP: 145/85
Monitor for complications- signs of CVD, stroke, PVD etc
Red flags
- Stage 3 or Malignant hypertension- >200/130 mmHg = assess for target organ damage ASAP +
- start drug Tx immediately if target organ damage
- repeat clinic BP in a week if no target organ damage
- SAME DAY SPECIALIST REVIEW IF:
- Papilloedema or retinal haemorrhage
- Life threatening symptoms or signs- suggested HF, AKI, consufsion, chest pain
- Phaeochromocytoma suspected
Young age - suggests secondary cause- but not red flag
Complications [if untreated]
8-10 y after onset:
- Atherosclerotic disease in 30%: eg CVD, PVD, Stroke
- Target organ damage in 50%- eg, brain, eye, kidney, heart, blood glucose [see pic for examples
Prognosis
If treated, good prognosis
If left untreated/uncontrolled severe consequences

What are the side effects of the hypertension medications?
ACE inhibitors
CCB
Thiazide diuretics
Beta/alpha blockers
ACEi- dry cough, increased potassium, increased creatinine
CCB- ankle swelling, angioedema
Thiazide diuretics- low potassium, dry mouth
Beta/alpha blockers- dizziness [postural hypertension]
What are red flag symptoms and signs of hypertension?
SEVERE RED FLAGS [Same day specialist review]:
Papilloedema/retinal haemorrhage
Symptoms of life threatening disease- chest pain, confusion etc.
Phaechromocytoma suspicion
Stage three hypertension- immediately assess for target organ damage and if present, start treatment immediately
What are the complications and prognosis of hypertension?
If untreated + mild to moderate:
30%= atherosclerotic disease- eg CVD, PVD
50%= organ damage- brain, eye, heart, kidney, blood vessels+ high blood glucose
SBA 1
a] 48-year-old woman, diagnosed with essential hypertension + commenced on treatment three months ago. She presents with a dry cough which has not been getting better despite taking cough linctus and antibiotics.
Which of the following antihypertensive medications is responsible for the patient’s symptoms?
A. Amlodipine
B. Lisinopril
C. Bendroflumethiazide
D. Furosemide
E. Atenolol
b] Which medication should she be started on as next line management instead?
A. Amlodipine
B. Spironolactone
C. Bendroflumethiazide
D. Furosemide
E. Losartan
B Lisinopril [ACE inhibitor]
and
E Losartan [ARB]
SBA 2
57-year-old man, Kevin, is reviewed in a hypertension clinic, where it is found that his blood pressure is 165/105 mmHg despite standard doses of amlodipine, perindopril, doxazosin and bendroflumethiazide. Electrolytes and physical examination have been, and remain, normal.
Which of the following would be your next stage in his management?
A.Arrange for his medication to be given under direct observation
B.Add spironolactone to his medication
C.Arrange urinary catecholamine assays
D.Request an adrenal CT scan
E.Add verapamil to his medication
A = poor adherence = most common cause of ineffective hypertension treatment
If good adherence, then B
SBA 3
47-year-old woman presents to clinic after being referred from her GP for consistently elevated blood pressure. Her last reading was 147/93. The female does not report any symptoms but recently lost her job and attributes the elevated reading to stress. Her blood tests are as follows:
Sodium = 146 (135-145 mmol/L)
Potassium = 3.4 (3.5-5 mmol/L)
Random glucose= 7.7 (4.4-7.8mmol/L)
Urea = 4 (2.5-7.8 mmol/L)
The next most appropriate investigation is:
A.CT scan
B. 24-hour ambulatory blood pressure
C. Abdominal ultrasound scan
D. Aldosterone-renin ratio
E. Glucose tolerance test
B
The main differential in this patient is hyperaldosteronism arising from an adrenal tumour (Conn’s syndrome). The excess aldosterone causes hypertension, elevated sodium reabsorption and potassium excretion. However, given the patient history, the elevated blood pressure could easily be due to the stress of having blood pressure measured or the patient’s personal situation. A 24-hour ambulatory blood pressure measurement (B) is therefore the most appropriate investigation to eliminate essential hypertension. Since the blood results are only mildly deranged and essential hypertension has not been eliminated, an aldosterone–renin ratio (D), CT scan (A) or abdominal ultrasound (C) would not be the first-line investigations to consider. They would be useful to investigate Conn’s syndrome if essential hypertension was excluded as a differential.
What are the normal heart sounds and the physiological causes of them?
S1- mitral/tricuspid valve closing- start of systole
S2- aortic/pulmonary semilunar valves closing- end of systole
When are heart sounds split?
Physiologically
S2 is split - first sound=aortic valve, second sound= pulmonary valve
-> right ventricular systole is longer because right heart filling augmented during inspiration because intrathoracic pressure decreasing increasing complicance of pulmonary vascular bed
Pathologically
Can be:
- Paradoxical - prolonged/delayed onset of left ventricle systole- mitral valve closed later
- Persistent- prolonged/delayed onset or prolongation of right ventricular systole
Normal wide splitting S1 – RBBB, LV pacing, ectopic beats
Paradoxical split S2: prolong LV emptying – aortic stenosis , LBBB – eliminated on inspiration
Widened split S2 – prolong RV emptying – pulmonay stenosis, RBBB
Fixed Split S2 – ASD