Urinary Tract Infections Flashcards
What is the definition of a UTI?
an infection of any part of the urinary system

What is the definition of an infection?
What does infection lead to?
an infection is the invasion of body tissues by a pathogenic organism
this causes an immune response, giving rise to symptoms
What is the most common type of pathogen causing a UTI?
in a UTI, the pathogen is often an endogenous bacteria that has got in the wrong place and invaded
What are the predisposing factors to UTI?
- female sex
- urinary stasis
- urological instrumentation (including catheters)
- sexual intercourse
- fistulae (recto-vesical, vesico-vaginal)
- congenital abnormalities (vesico-ureteric reflux)
What are common causes of urinary stasis?
- pregnancy
- prostatic hypertrophy
- stones
- strictures
- neoplasia
- residual urine from poor bladder emptying
Which areas of the urinary tract are sterile and colonised?
- the kidneys are ureters are sterile
- the bladder is considered sterile, but this may not be the case
- the urethra contains perineal flora

What makes up the perineal flora?
skin flora:
- mainly coagulase negative staphylococci
lower GI tract flora:
- ‘internal’ colonising bacteria are often found on the skin around the relevant orifice
enterobacterales:
- “coliforms” - enteric Gram-negative bacilli
Gram-positive cocci:
- Enterococcus spp.
What endogenous source are most UTIs caused by?
most infections are caused by gut bacteria (enteric flora)
perineum:
- movement of bacteria along a lumen
fistulae:
- movement of bacteria from the genital/GI tract to the urinary tract
What is the other cause of a UTI involving endogenous bacteria?
haematogenous spread
this is the seeding of bacteria to the urinary tract via the blood
e.g. Staphylococcus aureus
this is very rare
What organisms commonly cause UTIs?
- E. coli
- Staphylococcus saprophyticus
- Proteus mirabilis
- Enterococcus spp.
- Klebsiella spp.
- other coliforms
- Pseudomonas aeruginosa

What is the problem with knowing whether a bacteria is the cause of a UTI or whether it is local?
bacteria that cause UTIs can also:
- contaminate poorly taken samples
- colonise catheters
- cause asymptomatic bacteriuria (particularly in >65s)
What is the key to diagnosis in UTIs?
clinical signs and symptoms are the key to diagnosis
AND
microbiology results guide you to the culprit and appropriate, directed treatment
What is seen in asymptomatic bacteriuria?
no symptoms of a urinary tract infection
BUT
cultured urine sample will grow a single organism in significant numbers
What is cystitis?
What are the signs and symptoms?
it is a lower UTI that is more common in women
- dysuria
- frequency
- urgency
- supra-pubic pain or tenderness
- polyuria, nocturia, haematuria
What is pyelonephritis?
What are the signs and symptoms?
an infection of the kidney and/or renal pelvis
symptoms:
- all the symptoms of a lower UTI
- loin / abdominal pain or tenderness
- fever
other signs of systemic infection:
- rigors, nausea, vomiting, diarrhoea
- elevated CRP and WBCs
What are the 2 different types of UTIs?
complicated or uncomplicated
What is the difference between a complicated and uncomplicated UTI?
Complicated UTI:
- underlying abnormailty that is structural or functional
- e.g. urinary stasis - obstruction/retention
- presence of a foreign body
- e.g. catheter / renal calculi / biofilm
Uncomplicated UTI:
- in absence of above
In which types of people should a complicated UTI be suspected unless confirmed otherwise?
children < 10-12
men < 65
what is a catheter-associated UTI?
What are the risks and treatment?
indwelling catheterisation results in bacteriuria
biofilm formation has led to colonisation
manipulation or catheter removal may lead to bacteraemia
antibiotic prophylaxis can be indicated for some patient groups
What types of patient groups would be indicated for antibiotic prophylaxis against a catheter associated UTI?
- previous symptomatic CA-UTI with catheter change/removal
- traumatic catheterisation (including 2 or more attempts)
- purulent urethral/suprapubic catheter exit site discharge
- catheter or meatal/suprapubic catheter exit site colonisation with Staphylococcus aureus (including MRSA)
How is diagnosis of a catheter-associated UTI made?
diagnosis is made by clinical features
there is a need to distinguish between colonisation and infection
dipsticks are no use and “normal” / “sterile” results should not be expected
What is a nephrostomy?
an artifical opening created between the kidney and the skin which allows for the urinary diversion directly from the upper part of the urinary system (renal pelvis)
this is performed if there is a blockage in the urinary tract

What are the signs of infection following nephrostomy?
- fever
- pain and tenderness at the site
- haematuria or purulent discharge
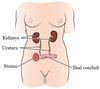
What is meant by an ileal conduit / urostomy?
a short section of the ileum is used to drain the ureters directly to a stoma on the anterior abdominal wall after cystectomy
What signs might be seen if there was an infection following ileal conduit / urostomy?
- fever
- ascending infection (upper UTI symptoms)
- para-stomal skin infections - redness, swelling, pus
Why is it important to recognise the symptoms of infection following nephrostomy or ileal conduit?
like catheters, colonisation of the tubing and bags occurs
What is meant by urosepsis?
What symptoms will be present?
systemic signs of infection related to any underlying urinary source of infection
- fever
- rigors
- nausea, vomiting, diarrhoea
- +/- haemodynamic compromise
- raised inflammatory markers (CRP, WCC)
often thought as akin to ‘upper UTI’, but there may not be clinical signs of pyelonephritis
What are some common causes of urethritis?
- some STIs cause urethral symptoms
- thrush (vulvovaginal candidiasis) causes irritation and dysuria
- urethral syndrome
What is meant by “urethral syndrome”?
Who is most commonly affected?
symptoms of lower UTI without any demonstratable infection
also known as abacterial cystitis and frequency-dysuria sundrome
mostly affects 30-50 year old women
What are the 2 different types of urinary tract abscesses?
perinephric and intra-renal
What causes a peri-nephric urinary tract abscess?
uncommon complication:
- renal stones and/or diabetics
- secondary to obstruction of infected kidney
gram-negative bacilli
What causes an intra-renal urinary tract abscess?
haematogenous spread:
- this can be unilateral, single or renal cortex
- caused by Staphylococcus aureus
classic acute pyelonephritis:
- in the cortex or medulla
what is prostatitis?
What are the signs and symptoms?
inflammation of the prostate
signs & symptoms:
- lower urinary tract symptoms
- fever
- tender tense prostate on PR palpation
- acute retention
Which pathogens cause prostatitis?
What are the risk factors associated with this condition?
pathogens:
- normal urinary pathogens e.g. E. coli
- can be caused by S. aureus
risk factors:
- procedures involving the prostate
- indwelling urinary catheter
What are the symptoms of chronic prostatitis?
- pain in and around the perineum and genitalia
- lower urinary tract symptoms
- enlarged or tender prostate on examination
What are the causes of chronic prostatitis?
>90% due to chronic pelvic pain syndrome
this is non-bacterial and will have a negative urine culture
chronic bacterial prostatitis
caused by recurrent UTIs with the same organism and asymptomatic in-between
If a diagnosis of UTI relies on clinical symptoms, what are the purposes of tests?
- to confirm clinical suspicion
- to find out the pathogen and how best to treat it
- to monitor response through inflammatory marker trends
- imaging can be used to look for abnormalities in urinary tract anatomy, stones and abscesses
this can guide the duration of therapy required
Why is it important to find out the pathogen causing a UTI and how best to treat it?
this allows for a directed approach to treatment
it confirms the empirical choice, or prompts change if needed
the narrowest spectrum antibiotic possible can be given
this reduces the impact on the patient’s microbiome and reduces risk of C. diff
What are the most common microbiological investigations for UTIs?
dipsticks, ward-tests and urinalysis
this provides a quick screen, but has limitations and is only suitable for certain groups
laboratory testing of urine samples
When should dipsticks/ward-tests/urinalysis NOT be used?
What are the guidelines surrounding their use in children?
do NOT use for catheter samples and unreliable in >65y
children:
- do NOT use if < 3 months
- 3m - 3y can use but if high risk send for culture regardless of result
- >3y they are reliable
What do dipsticks test for?
- blood
- protein
- nitrite
- white blood cells (leukocyte esterase)

What samples should be collected for microbiology lab tests?
urine:
- mid-stream (MSU)
- catheter urine (CSU)
- paediatric samples - “clean catch”, pad, bag
- supra-pubic aspirate (SPA)
blood cultures:
- suspected pyelonephritis or severe sepsis
What types of tests are performed on the urine samples?
microscopy, culture and sensitivity testing
What types of clinical details should be sent to the lab with the urine sample?
Why?
- age
- gender
- pregnant?
- symptoms
- antibiotics
- allergies
this allows the lab to determine what needs to be ‘set up’, what antibiotics to test and what growth is relevant
Why is mid-stream urine used?
the inital stream will pick up the bacteria colonising the urethra
the mid-stream better represents any bacteria actually in the bladder or higher urinary tract
What types of bottles should mid-stream urine be collected in?
sterile:
- should not be decanted into from non-sterile containers
preservative:
- e.g. boric acid (“red top”)
- this needs the right amount of urine but prevents overgrowth
How are lab results on urine samples interpreted?
What does a raised WCC, RCC and epithelial cells show?
if there is bacterial growth in the presence of clinical symptoms, this confirms diagnosis
raised WCC indicates inflammation
raised RCC indicates bleeding
epithelial cells may indicate contamination if present
What is meant by “sterile pyuria”?
pus cells (raised WCC) in the urine
no organisms are grown with standard lab methods
What can cause sterile pyuria?
inhibition of bacterial growth:
- antibiotics - collect sample before starting if possible
- specimen contaminated with antiseptic
“fastidious” (hard to grow) organisms:
- anaerobes
- Mycobacterium tuberculosis, Haemophilus spp.
urinary tract inflammation:
- renal or bladder stones
urethritis (sexually transmitted pathogens)
- Neisseria gonorrhoeae
- chlamydia trachomatis
When might an early morning urine test (x3) be requested?
What is needed specifically?
if suspected urinary tuberculosis
need to request acid fast bacilli (AFBs) specifically
this test has poor sensitivity and a tissue biopsy at the site of suspected disease would be better
What are the indications for further non-microbiological investigations?
What are these investigations?
- recurrent UTI
- any UTI in a male patient
- any UTI in childhood
- pyelonephritis
investigations:
- renal tract ultrasound scan
- CT KUB
- specialised tests - isotope scans, micturating cystourethrogram
What is involved in the non-antimicrobial management of UTIs?
- increased fluid intake
- anti-inflammatories - NSAIDs, ibuprofen
- device removal if no longer indicated
if the device is still needed, it should be changed under prophylaxis
- drainage is there is an obstruction or abscess
When are recurrent UTIs deemed to be “significant”?
recurrent UTI can be caused by re-infection or bacterial persistence
it is significant if there are 3 or more episodes within 12 months
What are the requirements for a “good” UTI antibiotic?
- gets into urine
- minimally toxic
- effective against the likely organisms
- easily administered
- cheap
What UTI antibiotics are commonly used?
- Nitrofurantoin
inadequate for systemic infections and prostatitis so used in lower UTIs only
- Pivmecillinam
- Trimethoprim
- Fosfomycin
How is cystitis treated in females?
- treatment is often started before microbiology results
- short course of antibiotics (3 days)
- in mild cases, a delayed prescription is given and patient is told to increase fluids +/- ibuprofen
What is the treatment of cystitis in males or recurrent cases?
- longer course of antibiotics - 7 days
if there are recurrent UTIs in men - think PROSTATE
What is the empiric therapy for pyelonephritis?
- broad action against likely urinary pathogens required
- needs to be systemically active
- cefuroxime, aztreonam, ciprofloxacin, gentamicin
What is involved in the directed therapy for pyelonephritis?
this is based on sensitivity results and the narrowest spectrum agent possible is used
not all oral agents are suitable for PO step-down
e.g. cannot use nitrofurantoin for follow on treatment
What is the duration of treatment for pyelonephritis?
7 - 14 days depending on antibiotic used
What must an agent that is used to treat prostatitis be?
- it needs to be active against likely pathogens
- it needs to penetrate the prostate
most antibiotics have poor penetration into prostatic tissue
penetration is better in the inflammation present in acute prostatitis
What are the empiric and directed options used to treat prostatitis?
what is the duration?
empirical options:
- piperacillin-tazobactam (IV only)
- ciprofloxacin (IV/PO)
directed options:
- as above
- trimethoprim or co-trimoxazole
duration:
- 2-4 weeks
Which patients should be treated for asymptomatic bacteruria?
pregnant:
- associated with upper UTI, pre-term delivery and low birth weight
Infants:
- preventon of pyelonephritis and renal damage
prior to urological procedures:
- prevention of UTI/bacteriaemia
elderly and catheterised patients DO NOT require antibiotics
What lifestyle modification factors are undertaken in treatment of confirmed recurrent UTIs?
- increased fluid intake
- review of contraception
- voiding before and after sex
- oestrogen replacement in post-menopausal women - local or oral
What are the antimicrobial strategies used to treat confirmed recurrent UTIs?
continuous prophylaxis with methanamine hippurate
no catheter and acidic urine needed
continous antibiotic prophylaxis - urology guided
this drives resistance, and therefore breakthrough infections with resistant organisms but may have short term benefit


