Laboratory Tests of Renal Function Flashcards
What contributes towards total body volume?
In health body volume is in a steady state
(this means what goes in should come out)

What does the concentration of any solute in the body depend on?
For any solute, the concentration depends on the amount of the solute present and the volume of solvent (water) in which it is dispersed
What happens if the input of a solute increases and the excreteion stays constant?
The concentration will rise
If the input of a solute decreases and the excretion stays constant, what will happen?
The concentration of the solute will fall
What will happen if the excretion of a solute decreases and the input stays constant?
The concentration of the solute will rise
What will happen to the concentration of solute if the body volume increases and decreases?
If the volume increases due to water overload, the concentration will fall
if the volume decreases due to water deprivation, the concentration will rise
What are the 3 main functions of the kidney?
Excretion:
- the kidneys excrete the end products of metabolism
- e.g. urea from amino acid breakdown
- uric acid from purine (nucleic acid) metabolism
regulation:
- e.g. homeostasis, water, acid base balance
endocrine:
- e.g. renin, erythropoietin
What are some of the homeostatic functions of the kidney?
- Maintenance of water balance by regulating urine volume
- acid base balance by altering hydrogen ion excretion
- sodium balance by altering the rate of sodium reabsorption
What are the endocrine functions of the kidney?
- Secretion of renin from the JGA which influences aldosterone
- erythropoietin effects the rate of red cell production
- 1,25 - dihydroxycholecalciferol is the active form of vitamin D, which affects calcium homeostasis
What types of defects will be seen in patients with chronic renal disease and impaired renal functions?
They show defects in endocrine and excretory functions before the loss of homeostatic control
when homeostatic functions cease, the patient is in renal failure and would die if there were no interventions
What are the purposes of renal function tests?
- They detect renal damage
- They monitor functional damage
- They distinguish between impairment and failure
What is an early test to detect renal damage?
What is a test used to monitor a patient with renal disease?
An early test to detect renal damage is a simple strip test for haematuria - important in screening for heavy metal poisoning
there is a clinical need to monitor a patient with renal disease - this is acheived by serial plasma measurements
About how many nephrons would have to lose their function before tests could detect this?
In renal disease, about half the nephrons have to lose their functioning before the abnormality can be detected by conventional laboratory tests
What are the pre-renal, renal and post-renal causes of kidney failure?
Pre-renal:
- e.g. decreased ECFV or MI
renal:
- e.g. acute tubular necrosis
post-renal:
- ureteral obstruction
What are all the laboratory tests of renal function?
The detection of substances such as red cells or glucose could be an early indicator of renal damage
- glomerular filtration rate
- eGFR - estimate
- creatinine clearance
- plasma creatinine
- plasma urea
- urine volume
- urine urea
- urine sodium
- urine protein
- urine glucose
- haematuria
What is the normal urine volume in health and what does this depend on?
Urine volume depends on how much you drink and sweat
In health it is closely matched to water balance by the hormone ADH, or vasopresssin (AVP)
750 - 2000 mL / 24 hours is typical in health
What is oliguria?
Abnormally low urine volume is a 24 hour volume less than 400 mL
this is oliguria
What is the definition of polyuria?
There is no absolute definition of polyuria as some people can drink an full lot and match it with a high urine output
if the urine volume is greater than 3 litres per day, and the patient is not drinking, this is polyuria
What is the output for anuria?
Anuria is less than 100 mL / 24 hours
What is the reference range for plasma urea?
How sensitive / specific is it?
It provides a quick, simple measurement
it has a wide reference range of 3 - 8 mmol / L
it gives a sensitive but non-specific index of illness
Why is the plasma urea measurement sensitive but non-specific?
The concentration of urea is increased in many different conditions, this makes it sensitive to the presence of disease but a non-specific test
What are the factors influencing plasma urea concentration?


Where is urea filtered?
What % of filtered urea is reabsorbed in health?
Urea is filtered at the glomerulus
about 40% of filtered urea is reabsorbed by renal tubules in health
60% of filtered urea is excreted
How does the amount of urea reabsorbed change with the rate of tubular flow?
The rate of urea reabsorption is variable and depends on the rate of tubular flow
more urea is reabsorbed if the flow rate is slow as there is more time for urea to diffuse into the peritubular capillaries
When does tubular flow rate tend to be slow?
When there is renal hypoperfusion
this may be following myocardial infarction
more urea is reabsorbed and plasma urea increases
What types of conditions result in renal hypoperfusion?
Fluid loss, circulatory insufficiency, renal artery stenosis
What are the causes of increased plasma urea?
How are they divided?
Acute renal impairment:
- gastrointestinal bleed
trauma
chronic renal disease:
- renal hypoperfusion
- decreased RBF
- decreased ECFV
post-renal obstruction:
- Calculus tumour
Why are the risks of performing a urea test?
It is a useful test but needs to be interpreted with great care
you need to consider input, output and a patient’s fluid volume
What is normal plasma creatinine?
What does this measurement show?
50 - 140 umol / L
it has a wide reference range
a body builder may have a plasma creatinine at the top end, and an old lady a value at the low end, reflecting muscle mass
measurement of plasma creatinine can provide a specific test of glomerular function
How long after a meal should plasma creatinine be measured?
Plasma creatinine should not be measured until 8 hours after a meal
there is some evidence that the concentration increases after meat ingestion
How is plasma creatinine concentration linked to GFR?
Plasma creatinine concentration increases when GFR falls
GFR has to fall quite considerably before the plasma creatinine reliably increases
What important analytical inferences need to be checked with a lab when interpreting plasma creatinine?
A patient with ketoacidosis, jaundice or infection might have agents in the plasma which could invalidate the measurement of creatinine
How is plasma creatinine linked to renal damage?
Plasma creatinine is not proportional to renal damage
How is the plasma creatinine change within an individual patient related to the absolute value?
The change within an individual patient is usually more important than the absolute value

How does plasma creatinine change in patients with chronic renal disease?
Patients with chronic renal disease have elevated plasma creatinine concentrations
this can be up to 1000 umol / L
plasma creatinine increases in an exponential fashion
How is a plot of reciprocal of plasma creatinine concentration used in clinic?
Renal physicians need to predict when a patient will require dialysis or transplantation
the plot of reciprocal of plasma creatinine concentration against time is used to predict when intervention is required

When is glomerular filtration rate measured?
It is rarely measured in clinical practice and is required when a patient comes to hospital
people who are considering donating a kidney whilst they are alive have their GFR measured
how is GFR measured?
It used to be measured by calculating the clearance of inulin
now radioactive substances are used
this is either technetium labelled diethylenediaminetetra acetic acid DTPA or 51-chromium labelled EDTA ethylenediaminetetra acetic acid
What is used as a marker of GFR?
Creatinine clearance
What are typical values for creatinine clearance in health?
100 - 130 mL / min
What samples must a patient give in order to calculate creatinine clearance?
The subject collects all the urine produced over 24 hours into a container
a portion of this urine is used to measure creatinine concentration - Ucreat
a blood sample during the 24 hours is needed to measure plasma creatinine concentration - Pcreat
What is the calculation for creatinine clearance?
What measurements are required ?
Ccreat = [Ucreat x V] / Pcreat
Ucreat = urine creatinine concentration (mmol/L)
V = urine volume (mL collected in 24 hours)
Pcreat = plasma creatinine concentration (umol / L)
In health, how much higher should creatinine clearance be compared to GFR?
Why is it higher?
Creatinine clearance should be 10 - 30% higher than GFR
it is higher as creatinine is secreted by the renal tubules
as plasma creatinine increases, the rate of creatinine secretion increases, so more creatinine in urine gets there by tubular secretion rather than by glomerular filtration
What does the fact that creatinine clearance is higher than GFR mean clinically?
Creatinine clearance is not a reliable marker of GFR in chronic renal disease
secretion is also inhibited by common drugs such as aspirin and cimetidine
Why is creatinine clearance an unreliable test?
- Tubular secretion is increased in chronic renal disease
- tubular secretion is inhibited by drugs such as salicylate and cimetidine
- problems with incomplete collection of urine
What is normal creatinine clearance, as a marker of GFR, in health?
How much must renal function be reduced until creatinine clearance is affected?
120 mL / min in health
there is no increase in plasma creatinine concentration until renal function is halved
with creatinine clearance at 20 - 60 mL / min, increased creatinine and urea can be measured in plasma
What are the plasma changes associated with the creatinine clearance decrease in chronic renal disease?

When creatinine clearance falls below 30 mL/min , what kind of changes are observed?
Hyperkalaemia and acidosis
when creatinine clearance becomes very low at 10 - 20 mL / min, then there is an increase in phosphate and uric acid
Currently, how is eGFR calculated in practice?
It is calculated in the lab using an international formula
In the UK, the abbreviated MDRD equation is used
What would the treatment decisions be if a patient had these eGFR readings?


In pre-renal oliguria, how would ADH levels change and why?
ADH increased
If a patient has lost water from the ECFV, then ADH is secreted
this produces a low volume of concentrated urine
urine osmolality is greater than 500 mmol / kg H2O
Why is urine urea concentration high in pre-renal oliguria?
There is increased urea reabsorption
plasma urea concentration will also be elevated
What does renal hypoperfusion (low RBF) lead to in pre-renal oliguria?
Renal hypoperfusion causes renin secretion
This leads to hyperaldosteronism - increase in aldosterone levels leads to functioning nephrons increasing sodium reabsorption
this means that urine sodium concentration is very low - less than 20 mmol/L
What can low renal perfusion in pre-renal oliguria/failure lead to?
- Dehydration - sodium / water
- haemorrhage
- renal artery damage
- hypotension
What would you expect the GFR, urine properties and renal renin secretion to be like in renal oliguria?
- GFR normal or reduced
- weak urine and a low volume produced
- renal renin secretion may be raised
Why may renal renin secretion be raised in renal oliguria?
What are the consequences of this?
Hypertension is present but the nephrons are unable to reabsorb sodium
this leads to urine sodium concentration being high and above 40 mmol/L
What types of things may cause renal oliguria / failure?
intrinsic damage:
- tubular necrosis
- chronic infection
- immunological damage - SLE
- toxic damage - drugs, heavy metals, poisons
What other clues and problems may be present that suggest renal failure?
- Anaemia
- haematuria
- proteinuria
- urine cases
- problems with calcium / phosphate or bone disease
What do PRU and ARF stand for in the differentiation of oliguria?
PRU - prerenal uraemia:
- refers to conditions that produce renal hypoperfusion
- e.g. Fluid loss and circulatory problems
ARF - acute renal failure:
- involves tubular necrosis
- there is damage to the nephrons
Why should a patient with ARF not be infused with a fluid?
Patients with ARF have nephrons which cannot respond to aldosterone or frusemide
urine sodium concentration is usually greater than 40 mmol/L
if they are infused with a fluid, this may lead to fluid overload with pulmonary oedema
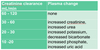
Complete the table for the differentiation of oliguria


What are the laboratory tests of renal function?
- Plasma creatinine
- plasma urea
- plasma sodium
- urine volume
- urine sodium
- urine urea
- creatinine clearance
- urine dipsticks
Which tests can be used to assess both hydration status and renal function?
Plasma urea and urine volume


