Inflammatory Skin Pathology & Skin Tumours Flashcards
What are the 2 categories of inflammatory skin disease and examples?
infectious
non-infectious inflammatory diseases:
- dermatitis / psoriasis
- blistering
- connective tissue diseases
- e.g. lupus erythematosus / dermatomyositis
- skin lesions as a sign of systemic disease
- skin lesions caused by metabolic disorders
plus some rare types
How common is eczema / dermatitis?
How severe it is?
it is very common and affects 5% of children in UK
it varies from trivial to severe
it is a reaction pattern rather than a specific disease
What are the 3 clinical stages of dermatitis (eczema)?
1. acute dermatitis:
- red skin, weeping serous exudate +/- small vesicles
2. subacute dermatitis:
- red skin, less exudate, lots of itching, crusting
3. chronic dermatitis:
- skin is thick and leathery secondary to scratching
What are the 3 things seen in the microscopy in dermatitis?
spongiosis:
- intercellular oedema within epidermis
chronic inflammation:
- predominantly superficial dermis
epidermal hyperplasia & hyperkeratosis:
- mild in acute dermatitis
- marked in chronic dermatitis
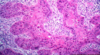
What is visible in this image?

spongiosis in eczema
What is atopic eczema?
When does it occur?
it is a type 1 hypersensitivity reaction to an allergen
it usually starts in childhood, but occasionally occurs in adults
there is often a family history and it is often associated with asthma and hay fever
What are the 2 types of contact dermatitis?
What causes them?
contact irritant dermatitis:
- direct injury to skin by an irritant
- e.g. acid, alkali, strong detergent
contact allergic dermatitis:
- e.g. nickel, dyes, rubber
- act as haptens which combine with epidermal protein to become immunogenic
What are the morphological subtypes of dermatitis of unknown aetiology?
seborrhoeic dermatitis:
- affect areas rich in sebaceous glands
- e.g. scalp, forehead, upper chest
nummular dermatitis:
- coin shaped lesions
What is psoriasis?
What % of the population are affected?
well defined, red oval plaques on extensor surfaces (knees, elbow, sacrum)
they have a fine silvery scale and Auspitz sign
removal of the scale causes small bleeding points
+/- pitting nails, +/- sero-negative arthritis
affects 1-2% of the population
What are the microscopic features of psoriasis?
“psoriasiform hyperplasia” has a distinct appearance:
- regular elongated club shaped rete ridges
- thinning of epidermis over dermal papillae
- parakeratotic (contain nuclei) scale
- collections of neutrophils in scale (Munro microabscesses)
What is the pathogenesis of psoriasis?
the clinical and microscopic features reflect massive cell turnover
What is shown here?

psoriasis

What are the genetic factors and environmental trigger factors involved in the aetiology of psoriasis?
genetic factors:
- some have family history
- multiple loci (psoriasis susceptibility or PSORS genes) with many in the region of MHC on chromosome 6p2 implicated
- this is the same area involved in other autoimmune disorders
environmental trigger factors:
- these are acquired factors
- infection, stress, trauma, drugs
What is the associated comorbidity in psoriasis?
- arthropathy (disease of the joints) associated in 5-10% cases
- psychosocial effects
- cardiovascular disease increased risk by 2-3 x
- cancer - increased risk of non-melanoma skin cancer & lymphoma
What are the 2 different types of lupus erythematosus?
discoid LE
- affects the skin only
systemic LE
- this is a visceral disease that may or may not involve the skin
What does lupus erythematosus look like clinically?
- red scaly patches on sun-exposed skin +/- scarring
- scalp involvement causes alopecia
- butterfly rash on cheeks and nose in SLE
What is lupus erythematosus?
What body parts can it affect?
an autoimmune disorder primarily affecting connective tissues of the body
autoantibodies are directed at various tissues
it may affect any part of the body, but importantly kidneys
What does lupus erythematosus look like microscopically?
thin, atrophic epidermis with inflammation and destruction of adnexal structures
IMF - LE band
IgG deposited in basement membrane
How does systemic lupus erythematosus (SLE) affect the body?
- 30% CNS involvement
- 50% butterfly erythema
- 50% pleuropericarditis
- 50% renal involvement
- 20% discoid skin involvement
- 90% arthralgia, arthritis
- 80% common symptoms (fever, fatigue)
- 70% vasculitis / skin involvement

what is shown here?

lupus erythematosus
What technique is used to detect lupus erythematosus?
immunofluorescence
What is dermatomyositis?
what test can be performed?
peri-ocular oedema and erythema (Heliotropic rash)
erythema in photosensitive distribution
myositis - proximal muscle weakness
(can check for creatinine kinase)
25% cases are associated with underlying visceral cancer
What is a heliotropic rash?
reddish purple rash on or around the eyelids
it is often accompanied by swollen eyelids
What does the microscopy look like in dermatomyositis?
- similar to lupus erythematosus
- often a lot of dermal mucin
- negative IMF
What are bullous diseases?
formation of fluid filled blisters
What is the difference between pemphigus and pemphigoid?
pemphigus:
- affects the outer layer of the skin (epidermis)
- causes lesions and blisters that are easily ruptured
pemphigoid:
- affects a lower layer of the skin, between the epidermis and the dermis
- causes tense blisters that do not break easily

What is pemphigus?
What types of blisters does it involve in?
group of disorders characterised by loss of cohesion between keratinocytes resulting in an intraepidermal blister
all types cause fragile blisters / bullae which rupture easily
can be extensive +/- involve mucous membranes
What is the pathogenesis of pemphigus?
autoantibodies directed against intercellular material
can be detected by immunofluorescence (IMF)
What is bullous pemphigoid?
What are the blisters like?
a disease characterised by subepidermal blisters
elderly with large tense bullae which do not rupture easily
it can be localised or extensive disease
What is the pathogenesis of bullous pemphigoid?
autoantibodies to glycoprotein in the basement membrane
it can be detected by IMF
What is dermatitis herpetiformis?
What is it associated with?
small intensely itchy blisters on extensor surfaces
often affects young patients and is associated with coeliac disease
What is the IMF and histopathology associated with dermatitis herpetiformis?
IgA deposition in dermal papillae on IMF
histopathology shows neutrophil microabscesses in dermal papillae
What is shown here?

dermatitis herpetiformis
small intensely itchy blisters on extensor surfaces
What type of bullae are present in dermatitis herpetiformis?
subepidermal bulla
IgA is present in dermal papillae

What systemic diseases can dermatomyositis and dermatitis herpetiformis be sign for?
dermatomyositis is a sign of visceral cancer
dermatitis herpetiformis is a sign of coeliac disease
What is acanthosis nigricans and what systemic disease can it be a sign for?
dark warty lesions present in the armpits
it can be a sign of internal malignancy

What is necrobiosis lipoidica and what systemic disease can it be a sign of?
red and yellow plaques on the legs
a sign of diabetes mellitus
What is erythema nodosum and what systemic disease can it be a sign of?
red tender nodules on the shins
associated with infections elsewhere (especially in lungs), drugs and other diseases
What type of skin tumours arise from the epidermis, melanocytes and Merkel cells?
epidermis:
- basal cell carcinoma
- squamous cell carcinoma
melanocytes:
- naevi
- melanoma
Merkel cell:
- Merkel cell tumour (rare but dangerous)
What type of skin tumours arise from adnexal structures, nerves/blood vessels and connective tissue?
adnexal structures:
- sweat gland and hair follicle tumours and cysts
nerves & blood vessels:
- haemangioma
- neuromas
connective tissue:
- dermatofibroma
What is the aetiology of basal cell carcinoma?
Does it metastasise?
aetiology:
- sun exposed site, especially on the face
- occasionally can be secondary to radiotherapy
- pale skin that burns easily
- immunosuppression
it is the commonest malignant tumour and metastases are very rare
What is a rare complication of basal cell carcinoma?
Gorlin’s syndrome
this is a condition that affects many areas of the body and increases the risk of developing various cancerous and noncancerous tumours
What does BCC look like clinically in the early and late stages?
- early - nodule
- late - ulcer (rodent ulcer)
image shows rodent ulcer with rolled edges

What does BCC look like microscopically?
tumour composed of islands of basalooid cells with peripheral palisade

What is morphoeic BCC?
What does this look like clinically?
the morphoeic basal cell carcinoma (mBCC) is the most aggressive subtype
it spreads into the dermis beyond the clinically visible or palpable borders, making complete excision difficult
it is ill-defined and infiltrative
What are the different causes of squamous cell carcinoma?
UV irradiation:
- usually occurs in sun exposed sites with increased risk in tropical countries
radiotherapy
hydrocarbon exposure:
- tars, mineral oils, soot
- e.g. SCC was found in scrotum of chimney sweeps
chronic scars / ulcers:
- SCC arises within these (Marjolins ulcer)
immunosuppresion:
- renal transplant patients at increased risk
drugs:
- some newer drugs for melanoma (BRAF inhibitors)
What does SCC look like clinically and microscopically?
clinically:
- nodule with ulcerated, crusted surface
microscopically:
- invasive islands and trabeculae of squamous cells showing cytological atypia
Does SCC metastasise?
What are other high risk features?
metastases in 5% to the lip, ear and perineum
high risk features:
- > 2cm
- > 4mm thick
- high grade
What is actinic keratosis?
What causes it?
a scaly lesion with an erythematous base that is very common on chronic sun exposed sites
it involves dysplasia to squamous epithelium
What can actinic keratosis lead to?
it is a pre-malignant disease
it only rarely progresses to invasive squamous cell carcinoma
it may spontaneously resolve
What is shown here?

actinic keratosis
(caused by chronic sun exposure)
Where are melanocytes derived from?
What is their function?
melanocytes are derived from the neural crest
they form melanin
this is transferred to epidermal cells to protect the nucleus from UV radiation
What tumours do melanocytes give rise to?
benign - naevi (moles)
malignant - melanoma

What are naevi (moles)?
What are the different types?
local benign collections of melanocytes
superficial:
- can be congenital or acquired
deep:
- blue naevi (mongolian spot)
What is atypical mole syndrome?
What are patients at an increased risk of?
multiple clinically atypical moles
histologically atypical / dysplastic naevi
seen in families with increased incidence of melanoma and associated with increased risk of developing melanoma
What is shown here?

common naevus (mole)

How dangerous and common is melanoma?
- it is much rarer than BCC and SCC but incidence is rapidly rising
- it is a very dangerous malignancy which can metastasize widely
What is the ABCD approach to distinguishing between a naevus and melanoma?
Naevus:
- symmetrical
- Borders even
- Colour uniform
- Diameter < 6mm
Melanoma:
- Asymmetrical
- Borders uneven
- Colour variation
- Diameter > 6mm

What 4 factors increase the risk of melanoma?
sun exposure:
- especially short intermittent severe exposure
race:
- celtic with red hair, blue eyes, fair complexions who tan poorly are most at risk
- melanoma is rare in dark skinned people
family history:
- atypical mole syndrome - multiple large atypical moles
giant congenital naevi:
- small risk of turning malignant (<5%)
What is lentigo maligna?
Who is usually affected?
a slow growing, flat, pigmented patch usually seen in elderly people
it is an early form of melanoma in which the malignant cells are confined to the tissue of origin (epidermis)
it occurs in sun damaged skin so is often found on the face or neck
What is the microscopic appearance of lentigo maligna?
What happens late in the disease?
proliferation of atypical melanocytes along the basal layer of the epidermis
skin also shows signs of chronic sun damage
late in disease, melanocytes may invade the dermis with potential to metastasise (lentigo maligna melanoma)
What is acral lentigenous melanoma?
Who is it most commonly seen in?
it is a specific type of melanoma that appears on the palms of the hands, the soles of the feet or under the nails (subungual)
the commonest form is seen in afro-carribbeans where it forms an enlarging pigmented patch
What is the microscopy of acral lentigenous melanoma like?
similar to lentigo maligna except no marked sun damage
What does superficial spreading melanoma look like?
it slowly grows horizontally across the top layer of skin before moving to the deeper layers
early - flat macule
late - blue / black nodule
most common type of melanoma
What is the microscopy of superficial spreading melanoma like?
proliferation of atypical melanocytes which invade the epidermis [pategoid spread] and dermis
What is meant by pategoid spread?
the “upward spreading” of normal cells in the epidermis
it is uncommon and a possible indication of a precancerous or cancerous condition
cells invade the upper epidermis from below
What are the genetics implicated in superficial spreading melanoma?
often, BRAF mutations are the target for anticancer agents

What is shown here?

melanoma
this image shows a melanoma with pagetoid spread

What is a nodualr melanoma?
What is the prognosis like?
starts as a pigmented nodule +/- ulceration
it is a dangerous form of melanoma that grows quickly and has poor prognosis

What is the microscopy of nodular melanoma like?
invasive atypical melanocytes invade dermis to produce nodules of tumour cells
What is Breslow thickness?
How can it be used to predict 5-year survival rates for primary melanoma?
measure on microscope from granular layer of epidermis to the base of the tumour
it gives a 5-year survival rate for primary melanoma

Which sites have a poorer prognosis in melanoma?
BANS
- back
- arms (posterior upper)
- neck
- scalp
all these sites have a poorer prognosis
What are the other 3 prognostic factors implicated in melanoma?
ulceration
satellites / in-transits:
- these are cutaneous deposits that occur before the first lymph node
sentinel node:
- lymph node which drains from the melanoma first
- it is removed, and if positive, the rest of the lymph nodes in that anatomic area are removed to try and halt disease progression
What are the treatment options for melanoma?
- surgery - excise primary melanoma and lymph nodes if the sentinel node is positive
- BRAF inhibitors - 60% of melanomas have a mutation in the B-raf gene


