acute leukaemia & MDS Flashcards
what is acute leukaemia a result of?
it is the result of accumulation of early myeloid (AML) or lymphoid (ALL) precursors in the bone marrow, blood and other tissues
What does acute leukaemia arise from?
it occurs by somatic mutation in a single cell within a population of earlly progenitor cells
it may arise de novo or secondary to prior chemotherapy/radiotherapy or develop from another haematological condition
What is the median age at presentation in acute myeloid leukaemia (AML)?
What are survival rates like?
median age at presentation is 69 years
poor survival rates compared with those < 60
optimal treatment for older patients is unclear
What are the clinical features of AML?
it presents with features of bone marrow failure
- anaemia
- infections
- easy brusing & haemorrhage
organ infiltration by leukaemia cells may occur e.g. spleen, liver, meninges, testes and skin
How can AML affect the mouth?
it can lead to gum hypertrophy
what are the haematological features of AML?
- anaemia
- low or high white cell count with circulating leukaemia cells
- low platelets
What are the 3 stages in diagnosis of AML?
- morphology
- immunological markers
- cytogenetics (chromosomes)
- certain abnormalities correlate with prognosis
- e.g. t(8;21) inv(16) and t(15:17)
what is shown in this image?

inv(16)
the inv(16) is one of the most frequent chromosomal translocations associated with AML
the inv(16) fusion protein interferes with transcriptional regulation
What are important prognostic factors in AML?
- age
- chromosomes
- molecular features
- NPM1 and FLT3-ITD
- extramedullary disease
- disease that doesn’t respond to treatment
What is intensive chemotherapy?
What is the % remission?
3-4 cycles of intravenous cytotoxic drugs are given centrally
80-85% complete remission with cycle 1
disease assessment after cycle 1
life is on hold for 6 months
What are the risks of intensive chemotherapy?
What should be done for high risk patients?
risk of death, sepsis, alopecia, infertility and tumour lysis
high risk patients go on to have a bone marrow transplant
What do you need to take into account when determining who should be targeted with intensive chemotherapy?
- age
- comorbidities
- body habitus
- lifestyle decisions
- cytogenetics
- molecular information
When should intensive therapy be started?
immediate treatment:
- critically ill patients with rapidly progressive disease (such as WCC > 100 x 109 / L) with respiratory / neurological / other organ compromise
all other patients:
- no proven benefit to early initiation of treatment
- wait for cytogenetics and mutational status prior to deciding on definitive therapy
what is shown in this graph?
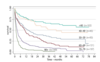
AML survival by age at diagnosis
survival rates decrease with increasing age
Whar is the main adverse prognostic factor in AML?
age is the most important adverse prognostic factor
there are other factors responsible for poor outcomes
What are the other adverse prognostic factors that explain why survival from AML is so poor?
- higher proportion of unfavourable cytogenetics
- frequent involvement of more immature leukaemic precursor clone
- multidrug resistance (MDR1/P-glycoprotein)
- antecedent haem disorders
- higher levels of co-morbidity
When do relapses of AML tend to occur?
relapses in AML occur within 18 months of intensive chemotherapy finishing
at 4 years post-chemotherapy, the patient is likely to be cured
What does treatment for relapsed AML consist of?
What does it depend on?
treatment depends on speed of relapse, AML subtype, physical state, co-morbidity and patient wishes
further intensive chemotherapy is possible followed by BMT
otherwise non-intensive treatment / experimental options
What is the main non-intensive treatment for AML?
In which patients is it used and in which should it be avoided?
low dose chemotherapy (cytarabine)
can get CRs in 8 - 18% of patients and it can prolong survival
it is useful in those not suitable for intensive chemotherapy, but is not good in patients with adverse cytogenetics
What is meant by “CR”?
complete response
this is the term used for the absence of all detectable cancer after treatment is complete
What are hypomethylating agents?
Who do they tend to be used in?
decitibine (dec) and azacytidine (aza)
they are used to treat AML in “unfit” elderly patients
they are well tolerated and can prolong survival
What are the purposes of newer treatments for AML?
What are they used with?
- target specific abnormalities expressed on leukaemia cells
- provide individualised treatments
- they are used in combination with chemotherapy or on their own
What are FLT3 mutations and how do they relate to AML?
FLT3 mutations occur in around 30% of AML patients
a common mutation is FLTIDT - FLT3-internal tandem duplication mutation
What is the FLT3-internal tandem duplication (ITD) mutation and how does it impact survival?
it is common and leads to constitutive activation of FLT3 receptor
it is a poorer prognostic marker and has an impact on overall survival and disease-free survival
Which protein is affected by FLT3 mutations?
FLT3 receptor tyrosine kinase
internal tandem duplication of genes occurs within the juxtamembrane domain
point mutations and gene insertions occur within the second kinase domain

What is the treatment to prevent poor prognosis from FLT3 mutations?
FLT3 inhibitors
- midostaurin
- quizartinib
- crenolanib
- gantesebib
- gilteritinib
they have variable specificity
How does midostaurin affect survival?
intensive chemotherapy + midostaurin shows an improved 4-year survival when compared to a placebo

What drug is used for IDH2 inhibition?
How does this impact survival?
Enasidenib
- 19% treated with enasidenib acheived complete recovery
When does Enasidenib tend to be used as a treatment?
in relapsed or refractory AML
What are the broad priniciples of treatment and common complications in AML?
broad principles of treatment:
- intensive chemotherapy / non-intensive chemotherapy / supportive care
common complications:
- neutropenic sepsis
- bleeding
what features are involved in the clinical presentation of acute lymphoblastic leukaemia (ALL)?
- fatigue
- bruising / bleeding
- weight loss
- night sweats
- hepatosplenomegaly
- lymphadenopathy
- mediastinal mass
What are the 4 components of treatment for ALL?
What should be done in high risk patients?
4 components:
- induction (8 weeks)
- intensification / CNS prophylaxis (4 weeks)
- consolidation (20 weeks)
- maintenance ( 2 years )
- if high risk proceed to bone marrow transplant after intensification
When does relapse tend to occur in ALL?
What is the average duration of survival at relapse?
disease relapse tends to occur within 18 months of stopping maintenance chemotherapy
average duration of survival at relapse is 4 months
What are current options for relapsed disease?
- further intensive chemotherapy
- blinatumomab
- inotuzumab
- CAR-T cells
- BMT - sib / MUD / Cord / Haplo
How does blinatumomab work?
it is a bispecific T-cell engager (BiTE)
it enables a patient’s T cells to recognise malignant B cells
each molecule combines 2 binding sites - a CD3 site for T cells and a CD19 site for the target B cells

What is the role of immunotoxins / immunoconjugates?
monoclonal antibodies / cell antigen binding fragment and a toxin moiety which induces cell death
this markedly increases the activity of the antibody (blinatumomab)
CD22 is the most attractive target
How does inotuzumab work?
it is used to treat relapsed or refractory ALL
the monoclonal antibody binds to CD22 on the surface of B cells and then releases calicheamicin
this induces cell cycle arrest and apoptotic cell death

What is the response rate and adverse effects with inotuzumab?
response rate is 57% with 18% CR
adverse effects:
- fever
- bacterial infections
- transient rise in transaminases
What are chimeric antigen receptors (CARs)?
receptor proteins that have been engineered to give T cells the new abiliy to target a specific protein

What is neutropenic sepsis a complication of?
What are the symptoms and how should it be treated?
it is a life-threatening complication of chemotherapy
symptoms:
- fever
- hypotension
- organ impairment
treatment:
- broad spectrum IV antibiotics as soon as suspected
What are the broad priniciples of treatment and common complications in ALL?
broad priniciples of treatment:
- intensive chemotherapy / bone marrow transplant
common complications:
- neutropenic sepsis
- bleeding
What is myelodysplasia (MDS)?
MDS represents several related disorders with common features
myelodysplastic syndromes are a group of cancers in which immature blood cells in the bone marrow do not mature and do not become healthy blood cells

What is the definition of MDS?
a heterogenous group of clonal bone marrow stem cell disorders that result in ineffective haematopoiesis with reduced production of one or more of the peripheral blood cell lineages
What are the features of MDS?
- dysplasia
- inefficient haematopoiesis
- cytopenias
- increased risk of transformation to AML
How does incidence of MDS change with age?
incidence of MDS increases with age

What scoring system is used in patients with MDS?
IPSS-R parameters
this groups patients into 1 of 5 groups, from very low risk to very high risk
this is based on risk of mortality and transformation to acute myeloid leukaemia (AML)
What are the 5 prognostic variables in the IPSS-R parameters?
- cytogenetics
- bone marrow blast %
- haemoglobin
- platelets
- absolute neutrophil count (ANC)

How is IPSS-R scored?
the risk group depends on your overall risk score from the 5 parameters

How is IPSS-R score related to prognosis?
the lower the IPSS-R score, the better the prognosis and longer survival time

What is the treatment for low risk MDS?
it should only be treated if it is symptomatic and you may only need to monitor the patient
erythropoietin is given for anaemia
blood product support is given as necessary
What is the treatment for high risk MDS?
treatment is aimed at altering the natural history of the disease
if the patient is fit enough, they are treated as per AML with intensive chemotherapy and bone marrow transplant
if they are not fit of have complex cytogenetics, azacytidine is considered


