Pathology of the Head & Neck Flashcards
How does the most common aetiology cause the changes described in the stroma?
trauma damaging tissue which can feasibly both directly make vessels leak by structural damage or trigger an inflammatory response which leads to increased vascular permeability
What is the significance of a polyp becoming fibrotic?
rather than being potentially reversible like oedema and fibrin deposition could be, fibrosis is likely to be permanent
it may only be remedied by a surgical procedure
What is the main factor influencing the severity of a polyp?
there are different implications of inflammation and fibrosis depending on the location
it is more life threating in organs such as the heart, liver, kidney or lungs
What are the 3 main lesions of voice abuse?
- vocal cord nodules
- vocal cord polyp
- contact ulcer
these are due to overuse or abuse and are more common in people who use their voice a lot (e.g. professional singers)
What are the main differences between vocal cord polyps and nodules?
nodules:
- usually bilateral
- present on opposing surfaces of the vocal fold, usually on the middle third
polyps:
- >90% are unilateral
- usually in Reinke’s space / ventricular space, usually on the anterior half of the vocal cord
they are clinically different, but histologically similar
What is Reinke’s space?
the part of the vocal cord that lies beneath the elastic lamina
some mucosa in this area is capable of almost intimate expansion
it is a potential space between the vocal ligament and the overlying mucosa
What is a vocal cord polyp?
Who is more commonly affected?
a reactive change of laryngeal mucosa and stroma resulting in benign polypoid or nodular growth
it is caused by vocal abuse and phonation changes
it can occur at any age but is more common in young women
What does a vocal cord polyp look like?
it has a smooth surface and affects the anterior half / anterior third of the vocal cord
it has a translucent appearance (can almost see through it)

What are the histological features of nodules & polyps?
- epithelium is usually unremarkable (normal)
- initially the stroma is edematous, with myxoid matrix
- later the stroma may demonstrate a spectrum of vascular proliferation, hyaline change, or fibrosis
- blood vessels and lymphatics become leaky
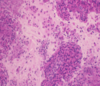
What is shown here?

vocal cord polyp
it is recognised by markedly oedematous stroma underlying a normal epithelium
What is shown here?

vocal cord polyp (late stage)
the polyp may progress to form fibrosis and a solid nodule
fibrin is present
this is plasma that has leaked out of damaged vessels and clotted to form the pink masses
What is the most common aetiology of vocal cord nodules and polyps?
voice abuse, in particular people who use their voice a lot
How can continuous trauma affect the vocal cords?
- trauma can directly damage structures or damage them enough to trigger an inflammatory response
- this leads to vessels becoming more leaky (reversible process as oedema becomes reabsorbed again)
- continuous trauma and inflammation leads to fibrosis
What is the definition of “precursor lesions of laryngeal squamous cell carcinoma”?
What is the problem with identifying these lesions?
squamous lesions with an increased risk of progression to squamous carcinoma
some histologically normal squamous mucosa can be a precursor for dysplasia and invasive squamous cell carcinoma
only 10% of precursor lesions progress to carcinoma
Who is more likely to be affected by precursor lesions of laryngeal squamous carcinoma?
Where are they usually found?
the supraglottic and glottis region are most affected
- peaks in 6th decade
- more common in males than females
- associated with carcinogen exposure - tobacco and alcohol abuse
What is shown here?

low grade dysplasia
abnormal but there is a definite risk of developing invasive carcinoma
What is shown here?

high grade dysplasia
malignant appearing epithelium is confined to the epithelium
there is no evidence of breach of the basement membrane and invasion of underlying tissues
What is a squamous cell carcinoma of the larynx?
What % of cancers does it account for?
a malignant tumour characterised by squamous differentiation
the supraglottic and glottic regions are most affected
it is 1% of all cancers but 90% of all head and neck cancers
Where is squamous epithelium found?
it covers the skin and most of the mucous membranes in the body
it keratinises, flattens off and becomes anucleate and impermeable to water as it becomes more superficial
Who is more likely to get squamous cell carcinoma?
males are much more commonly affected than females
it is associated with tobacco and alcohol abuse
these factors work synergistically
(much more likely to get it if you smoke and drink than if you just smoke and don’t drink)
What is the prognosis like for squamous cell carcinoma of the larynx?
prognosis is dependent on size, site, stage and differentiation
early lesions that are confined to the vocal cord (T1) have a 90% 5 year survival
there is a less than 50% 5 year survival for a T4 lesion
What is shown here?

squamous cell carcinoma
islands of squamous epithelium inflitrating into fibrous connective tissue
it is keratinizing (pink areas are keratin)
How do the 2 most common predisposing factors for laryngeal dysplasia act on the epithelium?
alcohol and tobacco smoke act as carcinogens (synergistically) and the mechanisms for carcinogenesis include:
- activating oncogenes (“foot on the accelerator”)
- inactivating tumour suppressor genes (foot off the brake)
- inhibiting apoptosis (“stopping the car from crashing”)
Why is inhibiting apoptosis a mechanism of carcinogenesis?
when cells show uncontrolled proliferation they may be confined to the basement membrane (“in situ”)
if they keep on proliferating in an uncontrolled way, there is more chance of acquisition of further mutations to enable further “bad” capabilities
What is the significance of grade in laryngeal epithelial dysplasia?
low and high grade make it more reproducible between pathology opinions (rather than having many grades)
low grade progression to invasion is 5-10% and management is to observe
high grade progress in 30-50% and management is treatment through excision or irradiation
What capabilities have invasive cells developing compared to those of non-invasive dysplastic cells?
- break down the basement membrane, stroma and other structures
- break apart from neighbours if adhesion molecules do not work as well
- move to allow invasion
- adhere to stroma to enable movement
- evade host immune response
- survive in vessels
- adhere to vessel lining at distant sites
- survive at distant sites
- produce own blood supply
What are sinonasal polyps and where do they develop?
polypoid lesions formed by expansion of the lamina propria of nasal mucosa by fluids, protein and fibrosis
found in the nasal cavity and paranasal sinuses
What are the clinical features and aetiology of sinonasal polyps?
clinical features:
- rhinorrhoea (runny nose)
- nasal stuffiness
- obstruction
- chronic headache
aetiology:
- allergy
- infection
- diabetes
- triad including aspirin sensitivity, asthma & cystic fibrosis
What is the prognosis of sinonasal polyps like?
they have no malignant potential
prognosis is excellent but they are often recurrent if the aetiological factors are not removed
What is shown here and how can it be recognised?

sinonasal polyp
underlying the epithelium is very oedematous
the submucosa is full of fluid and eosinophils / mast cells, highlighting the allergic aetiology
Who is most commonly affected by sinonasal polyps?
they equally affect males and females
most are over 20 and they are rare under 5 years
stromal atypia has no clinical significance and DDx is rhabdomyosarc
What is allergic fungal sinusitis?
Who is more commonly affected?
an allergic response to fungal allergens
(inhaled fungi sit within the sinuses - predominantly maxillary, but also frontal & sphenoid)
it is more common in warmer climates
it has an equal sex ration, but is more common in third to seventh decade
What are the clinical features of allergic fungal sinusitis?
What most commonly causes it?
may often find fungal hyphae, most commonly Aspergillus
clinical features:
- allergic symptoms
- nasal discharge
- rinorrhoea (runny nose)
- may be associated with peripheral eosinophilia and elevated antifungal IgG
What is shown here?

allergic fungal sinusitis
hypersensitivity to fungal antigens causes headaches & obstruction
lots of eosinophils are present and occasionally fungal hyphae are visible within the mucus
What is the treatment for allergic fungal sinusitis?
it is mainly treated with surgery (evacuation) but also with inhaled steroids
What is shown here?
What is a particularly dominant feature?
allergic fungal sinusitis
- mucin
- eosinophils
- Charcot-Leyden crystals
crystals are formed by the degranulation of eosinophils
What is shown here?

allergic fungal sinusitis
fungal hyphae are stained with a silver stain
cultures:
- aspergillus
- curvularia
- dreshella
- bipolaris
- exserohilum
What proportion of the adult population develop sinonasal polyps?
10%
How can sinonasal polyps lead to chronic headaches?
they obstruct the sinuses
sinuses are constantly draining mucus out of them and if they are blocked, pressure builds up
Which chronic self limiting inflammatory condition is common in the oral cavity?
oral lichen planus
In what group of patients is the prognosis better in oropharyngeal cancer?
those with HPV infection but no smoking and drinking history
the smoking and drinking makes the prognosis much worse
What is oral lichen planus?
Who is more likely to be affected?
common and chronic self-limited inflammatory mucocutaneous disorder of unknown aetiology
- 1-2% of world population
- more common in females
- peak in middle aged adults
What are the clinical features of oral lichen planus?
What is it associated with?
reticular variant:
- white patches consisting of fine white lace-like striae on the buccal mucosa
erosive variant:
- atrophic oedematous mucosa with ulcerations
it is associated with increased risk of malignant disease
What is squamous cell carcinoma of the oral cavity?
Where does it most commonly arise from?
malignant neoplasm arising from squamous epithelium lining the oral cavity
most common malignancy of the oral cavity and anterior 2/3 of the tongue
most commonly arises from the lip, tongue, floor of mouth, gingiva, palate and buccal mucosa
What is squamous cell carcinoma of the oral cavity often preceeded by?
What is the prognosis like?
often preceded by white (leukoplakia) or red (erythroplakia) mucosal patches
prognosis is stage dependent, but advanced stages have poor survival
What is squamous cell carcinoma of the oropharynx?
What is it commonly associated with?
usually a poorly differentiated squamous cell carcinoma with minimal keratinisation
most common at the tonsil and base of tongue
commonly associated with HPV 16 and 18
In what types of patients is the prognosis of squamous cell carcinoma of the oropharynx better?
prognosis is better in patients who do not have a carcinogen history (e.g. smoking / drinking) as well as HPV
prognosis is better in HPV-associated cases
What are the 4 main benign neoplasms of the salivary gland?
- pleomorphic adenoma
- basal cell adenoma
- canalicular adenoma
- warthin’s tumour
What is a pleomorphic adenoma?
a benign neoplasm composed of ductal epithelial cells and myoepithelial cells within a mesenchymal stroma
it shows divergent differentiation derived from a common stem cell
it is the most common salivary gland neoplasm
What is meant by a major and minor salivary gland?
major glands are the parotid, submandibular and sublingual
minor glands are distributed in the palate, oral cavity, tongue and also in the larynx, bronchi and trachea
Who is most commonly affected by pleomorphic adenoma?
What does it develop from and what are the clinical features?
peak age in fourth to fifth decade
disease in minor salivary glands is rare and 60% are in the parotid gland
it is an asymptomatic slow-growing mass
What are the 2 major clinical problems associated with pleomorphic adenoma?
if they are not excised completely then they recur
they tend to recur multifocally and they are not curable at this stage
they may undergo malignant transformation at a rate of 1% per year
What is meant by carcinoma ex pleomorphic adenoma?
What is the risk of carcinoma developing?
carcinoma arising in association with pleomorphic adenoma
risk of carcinoma development is dependent on the length of history of pleomorphic adenoma
non-invasive carcinoma has the same prognosis as pleomorphic adenoma
What is the prognosis like for non-invasive and invasive tumours in carcinoma ex pleomorphic adenoma?
non-invasive / minimally invasive:
- non-invasive carcinomas live within the same capsule as the pleomorphic adenoma
- minimally invasive are less than 1.5mm beyond capsule
- good prognosis
invasive:
- greater than 1.5mm beyond the capsule
- poor prognosis with < 50% alive at 5 years
- aggressive with systemic metastases to the bone, liver, lung and brain
What are the different malignant neoplasms of the salivary gland?
- adenoid cystic carcinoma
- mucoepidermoid carcinoma
- acinic cell carcinoma
- polymorphous low-grade adenocarcinoma
- carcinoma ex pleomorphic adenoma
What is an adenoid cystic carcinoma?
What % of neoplasms does it account for?
basaloid tumour consisting of epithelial and myoepithelial cells
(divergent differentiation)
accounts for 10% of salivary gland neoplasms with 75% arising in minor salivary glands
Who is most likely to be affected by adenoid cystic carcinoma?
What is significant about the outcome?
peak age instance fifth to seventh decade
it is an incurable epithelial neoplasm and most patients die of or with the tumour
metastasis to lung, bone, brain and liver seen in up to 60% of cases
In what anatomical location are pleomorphic adenomas most common?
usually in the major salivary glands
60% occur in parotid gland and they are rare in minor salivary glands
What sort of malignancy can arise in a pleomorphic adenoma?
carcinoma ex pleomorphic adenoma
the most important prognostic factor is whether it is confined within the capsule, minimally invading (<1.5mm) or invading beyond this
What is notable about the clinical progression of adenoid cystic carcinoma?
all patients will either die of it or with it
it is incurable and is one of the more common malignant tumours of the salivary glands


