Upper and lower limb injury Flashcards
(136 cards)
X-ray principles
The more a site absorbs x-ray the more white it becomes: air is black, soft tissue is grey, bone is white
Fracture lines are usually black unless bone impacts/ overlaps another bone in which case it appears sclerotic/ darker
To assess an x-ray look at all available views, use step by step approach and compare to past x-rays
How to describe a fracture
- Oxford handbook method:
- age of patient and how it occurred
- say whether it is compound and Gustilo type
- name the bone (specify right/left; whether dominant hand)
- position of fracture (e.g. proximal, supracondylar)
- type of fracture (simple, spiral, communicated, crush)
- intra-articular involvement
- deformity (displacement, angulation) from anatomical position
- grade/classification of fracture
- presence of complications (e.g. pulse absent, paraesthesia, tissue loss)
- other injuries and medical problems
How to describe a long bone fracture
Site: which bone and which part of the bone
Open/ closed
Fragments
Direct of fracture e.g. transverse, oblique, spiral
Articular surface involvement? Risk of subsequent osteoarthritis
Position of major fragments: the anatomical position of the distal component compared to the proximal component
Rotational deformity: has the fragment rotated?
Supracondylar: above the condyles of the femur/ epicondyles of the humerus
Intercondylar
Intertrochanteric: priximal femur between greater/ lesser trochanters
Steps of describing a fracture - simple
1. Describe radiograph: name, what, where, why, when
2. What type of fracture?
Direction: transverse, oblique, spiral
Salter Harris classification if it involves the growth plate
3. Where is the fracture?
Diaphysis: shaft
Metaphysis: widening portion next to growth plate
Epiphysis: end of the bone adjacent to the joint
4. Is it displaced?
Describes what happened to the bone during the fracture
Body assumed to be in anatomical position and the injury is described in terms of the distal component in relation to the proximal component
5. Anything else going on?
Joint involvement? Another fracture? Underlying bone lesion?
What is the Salter-Harris classification?
Only applies to children - this classification system does not apply to the well-developed bones of adults
Describes the patterns of fractures that occur through the growth plate of a long bone
Used to describe the fractures and predict the outcome as well as guiding management
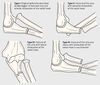
Discuss the Salter-Harris classification fracture types
Class 1-5
SALTR = MNEMONIC
Type 1: separation through the physis (growth plate)
S = SLIPPED
Type 2: fracture through the physis that extends ABOVE the physis into the metaphysis
A = ABOVE
Type 3: Fracture through the growth plate that extends into the epiphysis and involves the joint space, the fracture is lower in relation to growth plate
L = LOWER
Type 4: Through the growth plate, metaphysis and epiphysis
T = THROUGH
Type 5: Crush injury to growth plate, area is rammed together
R = RAMMED

Discuss type 1 Salter-Harris fractures
SLIPPED
5-7% fractures
Describes a slipping or separation of the growth plate
Does not involve bone, only the growth plate
Good prognosis - generally heals without surgery

Discuss type 2 Salter-Harris fractures
ABOVE
Occurs across growth plate (physis) and then ABOVE into metaphysis
Most common form of fracture - 75%
Good prognosis

Discuss type 3 Salter-Harris fractures
LOWER
Fracture passes along physis and then down through the epiphysis
Poorer prognosis - often an unstable fracture and can require operative management

Discuss type 4 Salter-Harris fractures
THROUGH
Passes through epiphysis, physis and metaphysis
Prognosis is variable, can be unstable and operative management should be considered
Discuss type 5 Salter-Harris fractures
RAMMED
Crushing injury damages the growth plate via compression
Worst prognosis of all 5 SH types

Fracture types
Simple: single, transverse fracture with 2 main fragments
Oblique: single, oblique fracture with 2 main fragments
Spiral: twists around long bone
Greenstick: seen in children, incomplete fracture
Comminuted: complex, >2 fragments - like someone has crunched the fracture site
Crush, wedge, burst, impacted
Avulsion: bony attachment of ligament or muscle is pulled off
Pathological
Stress: due to repetitive injury

Outline what open fractures are
A fracture is open when there is direct communication between the fracture site and the external environment
Most common open fractures: tibial, phalangeal, forearm, ankle and metacarpal
Consider the following consequences:
Skin: small wound to significant loss of skin meaning plastics may be needed to create a flap
Soft tissue: ranging from very little tissue loss to significant muscle, tendon, ligament loss which will require reconstructive surgery
Neurovascular: nerves and vessels may be compressed, go into spasm, be intimally dissected or transected
Infection: rate of infection following open fracture is high
What is the Gustilo classification?
Most commonly used system to classify open fractures
Uses the amount of energy, the extent of soft tissue injury and the extent of contamination to determine the severity of a fracture
Grade I: Open fracture, wound clean and <1cm
Grade II: Open fracture, wound <10cm without extensive soft tissue damage
Grade IIIA: Open fracture, adequate soft tissue coverage of fracture despite extensive laceration irrespective of the size of the wound
Grade IIIB: Open fracture with extensive soft tissue loss, usually with massive contamination and often needs soft-tissue reconstruction e.g. flap
Grade IIIC: Open fracture, vascular injury needing repair

Management of open fractures
Emergency: debride and lavage within 6hrs
IV antibiotics (broad)
Tetanus vaccine
Amputation is often required following IIIC open fractures
What is tetanus?
AKA lockjaw, a bacterial infection characterised by muscle spasms
Caused by clostidium tetani which is found in soil, saliva, dust and manure
Those who suffer a significant wound should be given a tetanus vaccine booster
What is subluxation?
Sometimes known as a partial dislocation
Partial loss of the congruity of a joint i.e. some parts of the articular surface of the bones contributing to the joint are touching each other

What is dislocation?
Articular surfaces at the joint have lost all contact with each other

Management of subluxation or dislocation
X-ray before reduction unless there is neurovascular compromise
What is a sprain?
Overstretching or tearing of a ligament
Causes pain, swelling and tenderness
Ranges from 1st-3rd degree depending on severity
3rd degree = completely torn, significant laxity and a snapping sound may have been heard

What is a strain?
Muscle-tendon injury
Pain on palpation and on active/ passive contraction
sTrain = Tendon

What is myositis ossificans?
Condition where bone tissue forms inside muscle or soft tissue after injury
Mainly occurs in the muscles of the arms and legs following trauma - mainly seen in young adults
Also seen in paraplegics, often in the absence of trauma
Presentation: painful, tender, enlarging mass often following localised trauma
Shows as an egg shell appearance on CT - often mistaken for osteosarcoma
Management of myositis ossificans
Myositis ossificans is benign and treatment is reserved for symptomatic lesions
Management is usally surgical which is often curative
Types of pathological fractures
Pathological fractures = fractures that occur in abnormal bone either spontaneously or following minor trauma that would not otherwise fracture normaly bone
Usually reserved for malignancies but also in other diseases e.g. osteomyelitis, Paget’s, bone cysts etc