Postoperative care Flashcards
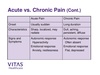
Outline differences between acute and chronic pain
Acute pain: less than 3 months, has a cause
Chronic pain: >3 months, persists after injury has healed, difficult to treat
Nociceptive vs neuropathic pain
Nociceptive pain:
- Obvious tissue injury or illness
- Protective function
- Sharp or dull, well localised
- Responds to analgesics
Neuropathic:
- Tissue injury may not be obvious
- Nervous system damage
- Burning, shooting, numbness
- Not well localised
- Poor response to analgesics
Physiology of pain
Periphery:
- Nociceptors are activated by tissue injury
- Release of chemicals can amplify the pain
- Signal travels via a delta or C fibres to the dorsal horn of the spinal cord
Spinal cord:
- Dorsal horn is the first relay station
- A delta or C fibre synapses with second order neuron
- Second order neuron travels up the opposite side of the spinal cord
Brain:
- Thalamus is the second relay station
- Connections to many parts of the brain
- The perception of pain occurs in the brain
Pain modulation
- Can occur in the spinal cord or brain
- In the dorsal horn, peripheral or spinal cord nerves can increase or reduce pain
- A descending pathway from brain to dorsal horn usually inhibits pain signals from the periphery

Outline the WHO analgesic ladder
Step 1: non-opioid analgesia
Step 2: weak opioid analgesia + non opioid analgesia
Step 3: strong opioids + non opioid analgesia
WHO analgesia ladder step 1
Paracetamol
- Mild pain
- Cheap
- Safe
- Can be given by multiple routes
- Can cause liver damage
NSAIDs
E.g. ibuprophen, aspirin, diclofenac, naproxen, indomethacin
- Mild pain
- Cheap
- Usually safe
- Can cause GI and renal side effects
- Can only be given orally
- Interferes with blood clotting
WHO analgesia ladder step 2
Mild opioids
Tramadol, codeine
WHO analgesia ladder step 3
Strong opioids
E.g. morphine, diamorphine, oxycodone, fentanyl
What is neuropathic pain?
Pain caused by damage or disease affecting the somatosensory nervous system
Due to abnormalities in the nociceptive pathway:
- Abnormal tissue
- Abnormal firing of nociceptors
- Changes to chemical signalling in the dorsal horn
- Abnormal nerve connections in the dorsal horn
- Loss of normal inhibitory function
- E.g. amputation/ cancer invading nerve plexus
What are the 5 Rs of fluid therapy?
Resuscitation
Replacement
Routine maintenance
Redistribution
Reassessment
Why do we use Hartmann’s or saline for fluid resuscitation?
They are isotonic and stay in the intravascular space for longer
Calculating maintenance fluids
- Need the patients weight
- Calculate the 24hr fluid volume in ml - multiply the patients weight by 25-30 e.g. 70kg x 25-30 = -5 1500-1800ml in 24hrs
- Work our the rate in ml/ hr - 1500ml over 24 hrs = 62.5ml per hr
- Work out the sodium and potassium requirements to choose the type of fluid - roughly 60mmol Na and K per day
A blood gas shows hypochloraemia, hypokalaemia, hyponatremia and a metabolic alkalosis - what are your thoughts?
Give 0.9% sodium chloride
Potassium replacement
Fluid resuscitation
- Give 500ml over 15 mins if patient haemodynamically unstable
- Except in patients with cardiac failure, renal failure and the elderly - consider 250ml boluses
- If no improvement after 2L - call for help
- In haemorrhage, replace fluid with blood products
Use of routine maintenance
If patient is unable to meet their fluid/ electrolyte requirement orally or enterally then they need IV fluids
Requirements:
- 25-30ml/kg/day fluid
- 1mmol/kg/day of K+ and Na+
- 50-100g glucose/ day
Which factors might indicate a patient may need fluid resuscitation?
Systolic BP <100
HR >90
Capillary refill >2s
Cold peripheries
RR >20
NEWS2 >5
NICE fluid therapy algorithm

Which is the only fluid option that contains K+
Hartmann’s - 5mmol/L


