Head and spinal injury Flashcards
Which type of head injury is most common?
Blunt trauma (as opposed to penetrating)
Common causes of head injury
- RTAs
- Falls
- Assaults
- Sports
- Workplace injuries
Primary vs secondary brain injury
Primary: occurs at time of injury, axonal shearing and disrutpion with associated areas of haemorrhage
Widespread: diffuse axonal injury
Localised injury: coup-contre-coup
>>The only cure for this would be to prevent accidents/ damage limitation e.g. helmets<<
Secondary: occurs later, due to various problems that commonly occur e.g. hypoxia, hypovolemia, intracranial haematoma and raised ICP, epileptic fits, infection
>>The aim of managament in ED is to prevent secondary traumatic brain injury<<
How do we calculate CPP?
MAP - ICP
MAP = systolic BP + diastolic BP + diastolic BP
Following head injury, what are the indications for referral to hospital?
- Impaired consciousness at any time
- Amnesia
- Neuro symptoms: vomiting, severe headache, seizures
- Skull fracture: CSF leak, peri-orbital haematoma
- Significant extracranial injuries
- Worrying mechanism e.g. high energy/ NAI
- Comorbidity e.g. anticoagulant use/ alcohol
- Adverse social factors e.g. home alone
Simple method of assessing the severity of a head injury
AVPU
Patient unresponsive/ only responding to pain - call for senior help + ICU/ anaesthetist as patient will need expert airway care and IPPV
Monitoring of patients following head injury
Every head-injured patient must receive regularneurological obs - early identification of complications e.g. intracranial haematoma, fits and hypovolaemia is esstntial in order for early treatment
Any deterioration in GCS is an emergency - re-examine and correct problems + call for senior help
Important to know about when taking a head injury hx
Mechanism: allows for impression of the forces involved and risk of complications
Time of injury
Loss of consciousness/ amnesia: unconsciousness suggests at least moderate severity, 30mins+ amnesia warrants head CT
Subsequent symptoms: headache, N&V, weakness, sensory loss, visual disturbance, rhinorrhoea, otorrhoea
PMHx: anything that could have caused the injury/ make it worse e.g. epilepsy, cardiac arrhythmias, DM, coagulopathy, thrombocytopenic
Drug hx: drugs/ alcohol, antigoagulants, patients on clopidogrel may be at higher risk of intracranial haemorrhage following head injury so low CT threshold
Social: is there someone at home/ someone they can stay the night with
Discuss the GCS score
Scored from 3-15 assessing eye response, verbal response and motor response
Unconsciousness is taken to mean no eye response and GCS =<8
Simple blood test essential in all patients presenting to a&e following head injury/ confused
BLOOD GLUCOSE
DONT EVER FORGET GLUCOSE
Areas to cover in examination following head injury
C-spine
GCS
Vital signs/ obs
Blood glucose
Alcohol: never assume low GCS is due to alcohol
Eye signs: pupils
Scalp, face, head: cranial nerves
Limbs: neuro exam
Other injuries: intra-abdominal injuries often co-exist with serious head injuries
Signs of base of skull fracture
Often a clinical diagnosis
- Bilateral orbital bruising confined to orbital margin: panda eyes
- Subconjunctival haemorrhage
- Bleeding from ears/ blood behind typanum
- CSF otorrhoea and rhinorrhoea: separates into double ring when dropped on blotting paper
- Battle’s sign: brusing behind ears without local direct trauma - occurs due topetrous temporal bone facture - takes a few days to appear

Clinical features pointing towards an intracranial haematoma
Emergence of focal neurological signs
Deteriorating GCS
Indications for CT scan following head injury
GCS <13 on initial assessment
GCS <15 after 2hrs
Suspected skull fracture/ basal skull fracture
Post injury seizure
Focal neurological deficit Vomiting
Amnesia >30mins
LOC
Dangerous mechanism
Most requests will be urgent - scan interpreted within 1hr
Initial management of a head injury
ABCDE dont ever forget GLUCOSE
2x IV large bore cannula
Bloods: FBC, clotting screen, U&E, glucose
If GCS =<8: rapid sequence induction + intubation
Arrange CT
Give IV antibiotics for compound skull fracture
Liaise w/neurosurgery early
Urinary catheter
Treating complications of head injury
Diminishing consciousness likely to reflect intracranial pathology leading to rise in ICP
Liaise w/ neurosurgeon: they may advise use of mannitol to decrease ICP as a time buying measure
Hypertonic saline acts as an osmotic agent and can dcrease ICP whilst increasing intravascular volume
What medical therapy is used to reduce ICP to buy time?
Mannitol - bolus IV
Hypertonic saline
Investigations and management of patient with seizure
Check glucose and ABG
Give IV lorazepam - repeat once if it doesn’t work
IVI phenytoin with ECG monitoring (can cause bradycardia when given IV)
Levetiracetam is an alternative to phenytoin
Seizure >10-15mins - senior help, RSI, intubation and IPPV
Golden rules for managing head injury
- Never attribute low GCS to alcohol alone
- Never discharge a head-injured patient to go home alone
- Consider admitting patients with head injury who have a coagulopathy/ anticoagulants
Head injury warning instructions
Adults
- Ensure eye is kept on patient for 24hrs
- Rest 24hr
- Pain killers
- No alcohol for 24hrs
- Do not take sleeping tablets
- Any of the following, come back: persistent headache, vomiting, visual changes, balance problems, fits, unrousable
Children
- Child may be more tired than usual
- Allow them to sleep
- Pain killers
- Any of the following come back: persistent headache, vomiting, visual changes, balance problems, fits, unrousable
Post-concussion symptoms
Frequent: headache, dizziness, lethargy, depression, inability to concentrate
~30% patients have headaches for 2months
Migraine may become more frequent after head injury
Diagnosis of exclusion
Subdural haematoma: consider in alcoholics/ elderly and those on anticoagulants - low threshold for CT
How are post concussion symptoms managed?
Reassure + explain that they are likely to resolve gradually
Arrange appropriate follow up with GP
Concussion advice for those who play sport and high-level sport
Rest initially, especially when symptomatic
Take advice from those within their sport about when it is safe to return
Pulsatile tinnitus/ whooshing sound in one ear following head injury
Consider carotid/ vertebral artery dissection
What evidence might there be on the bedsheet of a patient with a CSF leak?
Blood surrounded by a halo of pale fluid

Assessing for maxillofacial injuries
Palpate facial bones systematically
Dish face, flattening of cheek, assymetry, nasal deviation, uneven pupil levels (orbital floor fracture)
Loose/ lost teeth: may have been aspirated
Which airway adjunct should not be used in patients with facial fractures
NP - can go into brain
What is silver trauma?
Trauma in the elderly
Most common cause of serious injury in those 60+ is a fall from standing
Why is it so important to immobilise the neck
It is the most common site of cord injury
Important to note that ventilation can be impaired due to cord oedema so keep a regular eye on diaphragmatic breathing and use pulse oximetry and regular ABGs to confirm adequate oxygenation
Indicators of spinal injruy in patients with loss/ decrease in consciousness
Flaccid arreflexia
Decreased anal tone
Diaphragmatic breathing
Able to flex C5/C6 but not extenf C6/C7
Response to pain above the clavicle but not below
Hypotension + bradycardia
Priapism
Initial management of a patient with a spinal cord injury
Monitor ECG and BP: interruption of cord sympathetic system causes loss of vasomotor tone + vasodilation, venous pooling and decreased BP
Insert urinary catheter to monitor urine output and prevent bladder distension
Neuro examination
Use MRC power scale
Standard practice to record the most caudal location which has normal motor and sensory function
Anterior cord syndrome
Loss of power and pain sensation below injury, preserved touch and proprioception
Posterior cord syndrome
Loss of sensation and prorioception, power preserved
Brown-Sequard syndrome
Hemisection of cord
Ipsilateral paralysis + sensory loss below injury
Contralateral loss of pain and temperature
Central cord syndrome
Tyoically seen in the elderly following extension injuries to the neck
Affects upper limbs more than lower, variable sensory deficits
Incomplete tetraparesis/ quadraparesis
Epidemiology of head injuries
- Commonest cause of death and disability in those aged 1-40 in UK
- 1.4 million ED attendances/ yr
- 70-88% male
- 33-50% <15yrs
- 95% have GCS 13-15 on arrival
- 0.2% die due to head injury
Classification of head injury based on GCS
Mild: 13-15
Moderate:9-12
Severe: =<8
Normal ICP?
10mmHg
Consequences of uncal herniation
Compression of 3rd cranial nerve: ipsilateral pupillary dilation then loss of eye movements
Compression of ipsilateral corticospinal tracts in the brainstem leading to contralateral hemiparesis
Consequence of foramen magnum/ tonsillar herniation
Decreased ocnsciousness
Decorticate posturing
Irregular respiration
Loss of brainstem reflexes
Bilateral fixed + dilated pupils
Cushing’s response: high BP, bradycardia, abnormal breathing
Most common vessel causing extradural haematoma
Middle meningeal
Typical presentation of patient with extradural haematoma
Lucid >> aware >> lucid
*Although this is spoken about in the literature it is not overly common*
- Likely to have skull fracture, temporal bone most common
Shape of bleed on CT following extradural haematoma
Lens shape - blood can only travel so far when outside the dura mater
What vessels are responsible for subdural haematomas?
Tearing of bridging veins between brain and dura
Bleeding involves entire surface of brain
May be sub-acute/ chronic e.g. in elderly or alcoholics
Why are subdural bleeds more common in people with smaller brains e.g. alcoholics?
The brain is smaller and the veins are stretched which makes them more prone to bleeding
Discuss coup-contre coup injuries
Coup: region affected directly related to external injury site
Contre-coip: region affected is opposite site of external injury, due to movement of the brain within the skull

Why is it so important to manage pain following head injury?
Pain can lead to raised ICP
Algorithm for patients requiring CT head following head injury

Risk factors for c-spine injury
- Age >65
- Known chronic spinal conditions e.g. ankylosing spondylitis, rheumatoid arthritis
- Dangerous mechanism of injury e.g.
- Fall from height of greater than 1m or 5 steps
- Axial load to the head e.g. diving, falling on to head
- High speed motor collision
- Accident involving motorised vehicles
- Bike collision
- Horse riding accidents
Imaging based on Canadian c-spine rules

Problems with c-spine immobilisation
Collars significantly raise ICP
Long boards and collar cause pain and tissue ischaemia
Supine immobilisaiton causes deterioration in resp. function
What are the nexus criteria?
If all of the following 5 criteria are negative, the patient is classified as having a low risk of c-spine injury
No focal neurological deficit
No midline cervical tenderness
Normal level of alterness
No intoxication
No painful distracting injury - an injury so painful that it distracts the patient from a neck injury

How to manage a patient in whom a c-spine injury cannot be excluded clinically
Plain x-rays fon’t detect all c-spine fractures
- 3 view x-ray: lateral, AP and odontoid peg (open mouth) view
- CT scan should not be undertaken lightly as it exposed patient to 14x dose of radiation compared to x-ray
- MRI indicated if there is any neurology referable from the cervical spine or if there is severe pain despite normal CT
*NICE guidelines do not recommend use of MRI to clear c-spine

Pitfalls of c-spine management
Patients holding their head in a fixed flexed position - do not try and get their head in a collar >> can cause paralysis in patients with ankylosing spondylitis
Fractures are often missed in patients with distracting injuries/ intoxication
Red flags of acute lower back pain
- Onset age <20 or >55
- Non-mechanical pain e.g. unrelated to time or activity
- Thoracic pain
- Previous hx or cancer, steroids or HIV
- Fever, night sweats or weight loss
- Widespread neuro symptoms
- Structural spinal deformity
What is spondylolisthesis?
Forward slippage of one vertebrae onto another
Most common:
- L4 on to L5
- L5 on to S1
Usually occurs in young people
Vertebrae
- 7 cervical vertebrae
- 12 thoracic vertebrae
- 5 lumbar vertebrae
- Sacrum
- Coccyx
Where does the spinal cord begin?
Caudal medulla oblongata at the level of the foramen magnum

Which spinal tracts can be clinically assessed?
Corticospinal
- Located in the posterolateral cord
- Function - motor innervation
- Decussates in the medulla
- Injury to this tract causes ipsilateral weakness
Dorsal columns
- Located in the posteromedial cord
- Function - light touch and proprioception
- Decussates in the medulla
- Injury causes ipsilateral loss of sensation
Spinothalamic
- Located in the anterolateral cord
- Function - pain and temperature innervation
- Decussates immediately after entering spinal cord
- Injury causes contralateral loss of pain and temperature
Can a patient be diagosed with a complete spinal cord injury in the acute setting?
No - spinal shock will affect the function so important to wait before diagnosis is made
Spinal levels

What is neurogenic shock?
- Results from damage to descending sympathetic pathways in the cervical and upper thoracic spinal cord
- Results in loss of vasomotor tone and cardiac sympathetic innervation
Leads to hypotension and bradycardia/ absence of tachycardia as vagal tone dominates
Hypotension may not be corrected by fluid resus alone - may need vasopressors
What is atlanto-occipital dislocation?
AKA internal decapitation
Sepatation of the spinal cord from the skull base
70% cases result in immediate death
Most commonly due to high speed RTA
Common cause of death in shaken baby syndrome

What is the atlas?
C1 - first cervical vertebrae, just after the occiput

What causes cervical spine fractures?
Secondary to exaggerated flexion/ extension
Direct trauma
Axial loading (force directed through the top of the head and through the spine)
Why is the c-spine more susceptible to injury?
Highly mobile with relatively small vertebral bodies
Supports the head which is heavy
Which are the most commonly fractured vertebrae?
C2 and C7
Most common mechanism for c-spine fractures
Flexion
What is the mechanism of a hangman’s fracture?
Hyperextension injury e.g. high speed RTA
Causes fracture of the posterior elements of C2

What is spinal shock?
Loss of sensation accompanied by motor paralysis with initial loss but gradual recovery of reflexes
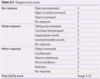
MRC power grading
- 5 = normal power
- 4 = weak
- 3 = movement against gravity
- 2 = movement with gravity eliminated
- 1 = flicker of movement
- 0 = complete paralysis
Key myotomes
- C5: shoulder abduction, deltoid
- C6: elbow flexion, biceps
- C7: elbow extension, triceps
- C8: wrist and finger flexion
- T1: finger abduction, interossei
- L2: hip flexion, iliopsoas
- L3-4: knee extension, quadriceps
- L4-S1: knee flexion, hamstrings
- L5: ankle and hallux dorsiflexion, extensor hallucis longus
- S1: ankle plantarflexion, gastrocnemius
Indications for doing a CT spine as opposed to a 3-view x-ray
- Elderly patients
- Patients with known or presumed cervical spine degenerative disease
- GCS <13
- Intubated patients
- Inadequate plain film series
- Suspicion or certainty of abnormality on plain film series
- Patients being scanned for head trauma and/or multi-region trauma as well
How to assess spinal x-rays
Confirm details, time and date x-ray taken
Ensure 3 views available for c-spine
- Alignment of vertebrae: no ‘steps’ should be visible - straight lines or curves
- Alignment on the AP film can be assessed by looking at the spinous processes and tips of the transverse processes - Look at interspinal distances: should be roughly similar in height throughout cervical spine with no obvious loss of height
- Assess the integrity of each vertebrae: bodies, laminae and pedicles - don’t stop searching once an abnormality is found
- Soft tissue: pre-vertebral soft tissue (anterior to vertebral bodies, best assessed using lateral view, tissue apprears as light grey - widening of this space may inficate pre-vertebral haematoma - this should raise suspicion of cervical fracture
- Alignment: assess the alignment of all relevant views (e.g. lateral, AP and open mouth).
- Bones: assess each of the vertebrae, inspecting the cortex for irregularities.
- Cartilage: assess the height of each intervertebral disc.
- Soft tissue: assess the pre-vertebral soft tissue width, for evidence of swelling

1st line imagine of patients with suspected spinal injuries >65yrs
CT - x-ray is not done as it will be difficult to interpret due to degenerative changes


