Organ failure and referral Flashcards
What does ICU do?
Cares for patients with severe life threatening illness who require enhanced monitoring and organ support - they replace the failing organ system e.g. if the patient needs oxygen, they give oxygen
- ICU get the patient through the illness and allow the medical or surgical team to do the work they need to do
Which patients go to ICU?
- Those needing higher level monitoring or organ support
- Those with reversible pathology
- Those with physiological reserve to survive intensive care or invasive treatment - difficult to judge this, the ICU consultants make this call
Levels of care in the hospital
- Level 0: patients whose needs can be met through normal ward care in an acute hospital. Approx. 1 nurse to 8 patients
- Level 1: patients at risk of their condition deteriorating or those recently relocated from higher levels of care whose needs can be met on an acute ward with additional advice and support from the critical care team. Sometimes used as a step down area e.g. patients have come from ITU and need a good level of care but not intensive. 1 nurse to 4 patients
- Level 2: HDU areas, patients requiring more detailed observation or intervention including support for a single failing organ system or post-operative care and those stepping down from higher levels of care
- Level 3: patients requiring advanced respiratory support alone or basic respiratory support together with support of at least two organ systems. Includes all complex patients requiring support for multi-organ failure
Discuss nasal high flow oxygen
- Like a big nasal cannula
- Up to 95% o2
- 1060L/min depending on brand
- Air is humidified and warmed
- Allows patient to talk and eat
What is CPAP?
- Continuous positive pressure ventilation - does not breathe for the patient
- Positive pressure via a mask or hood - increases oxygenation
- Fi 100% oxygen
- Allows titration or PEEP or EPAP
- Increases intrathoracic pressure - less blood returns to the heart and thus reduces preload and can cause low blood pressure
- Treatment for T1RF or heart failure - reduces preload and reduces the strain on the heart
What is BiPAP?
- Bilevel positive pressure
- Same as CPAP but can give 2 levels of pressure
- EPAP increases oxygenation
- IPAP increases CO2 removal
- Treatment for T2RF (low o2, raised co2)
Mechanical ventilation
- Fully controlled ventilation
- Can set IPAP and EPAP
- Requires sedation
- Problems with sedation and paralysis: hypotension, arrhythmias, opiate withdrawal, sleep problems, PTSD, weakness, airway trauma and oedema
- IPPV > CPAP if consolidation
- Requires significant physiological reserve
ECMO
- Extracorporeal membrane oxygenation
- Essentially like a cardiac bypass machine but the heart keeps beating
- Allows oxygenation and removal of co2
- Very specific criteria - often reserved for young patients waiting for lung transplants or patients stuck on bypass after surgery
- Require very large ventral venous access

Acute indications for renal replacement therapy
- Refractory fluid overload
- Severe hyperkalaemia
- Signs of uraemia
- Severe metabolic acidosis
- Removal of certain toxins e.g. lithium, ethanol, methanol, salicylate
Discuss invasive haemodynamic monitoring
Arterial line - long cannula into artery
- Usually radial but can use any
- Real time BP monitoring
- Can take bloods/ ABG
Non invasive cardiac output monitoring
- Central line/ PA catheter (not often used outside of cardiothoracic)
- Venous line in neck - goes into the right side of the heart and pulmonary tree
- Measures pressure in central veins/ right atria/ ventricle/ pulmonary artery
Transoesophageal ECHO
- Real time monitoring of cardiac output/ contractility - measure flow and cardiac output using ultrasound
Alpha and beta receptors in summary
alpha receptors are in the vessels, they squeeze
beta receptors are in the heart, they pump
What is iSBAR?
Framework used to structure communication to other healthcare professionals regarding patients
The purpose of iSBAR is to communicate or escalate effectively in a structured way with the aim of improve patient safety
i: Identify yourself and your patient - here it is recommended that (once qualified) you use your title of Dr because it grabs attention
S: Situation: short opening statement stating the name and age of the patient, the problem and your location
B: background: concise summary of the presentation and any relevant PMHx
A: Assessment: relevant + and - of A-E, don’t just list all the observations, say the most important thing first
R: Recommendation: advice over the phone or do you want them to come and see the patient? Make this clear - avoid telling people what you think they should do clinically but re-iterate your concerns. Steer clear of demands e.g. you need to take this patient to ICU - alternative would be ‘I’d like a critical care opinion’

What are the benefits of iSBAR?
- Promotes quicker and more effective handovers
- Structure helps to remove vagueness and uncertainty from communication
- Common system used by all healthcare professionals regardless of role/ hierarchy
- Easy to remember
- Can be used in a variety of ways: in emails, over the phone, letters, during handover
Tips for referrals
- Ask who you are speaking to and write their name and grade down in the notes with the time of the referral
- Be calm and polite
- Ensure you take the notes and relevant investigations plus the latest observations to the phone so you can answer any additional questions or have the electronic records open in front of you
- Can be useful to write down what you want to say first
- Avoid listing the whole hx and A-E - only what is relevant
- What are you most worried about? Use key phrases to get peoples attention depending on the clinical situation
- Practice is key
What is NEWS2?
National Early Warning Score (version 2)
Use of 6 physiological parameters to identify unwell patients as early as possible
Aggregate system – the scores for each parameter are added together to give an overall score
The score indicated how unwell patients are
Parameters that make up NEWS2
- Respiratory rate
- Oxygen sats
- Systolic BP
- Pulse rate
- Level of consciousness or new confusion
- Temperature
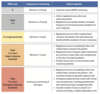
Response to NEWS2 score?
0: monitor every 12hrs minimum, continue reoutine obs
1-4: monitor every 4-6hrs, inform nurse, nurse then decided whether increased obs frequency is needed or whether escalation required
3 in single parameter: monitor every hr minimum, nurse to inform medical team who will review patient and assess whether escalation needed >> consider sepsis if scoring 3 in one parameter
5+: monitor every hr minimum, medical team informed by nurse, nurse to request assessment by clinician
7+: continuous monitoring of vital signs: medical team should be immediately notified (at least specialist reg level), emergency assessment, consider transfer to a level 2/3 clinical care facility (higher dependency unit)
Score of 3 in any one parameter or 5+ accumulative? Consider sepsis
Categories of shock
Hypovolaemic: inadequate circulating volume secondary to fluid loss
- Haemorrhage
- Diarrhoea and vomiting
- Diabetic ketoacidosis
- Burns
Obstructive: inadequate cardiac output as a result of mechanical obstruction
- Pulmonary embolism
- Tension pneumothorax
- Cardiac tamponade
- Acute IVC or SVC obstruction
Distributive: inadequate perfusion secondary to maldistribution
- Sepsis
- Neurogenic shock
- Anaphylaxis
Cardiogenic: inadequate cardiac output due to cardiac failure
- MI
- Myocarditis
- Late sepsis
- Over dose e.g. beta blockers
- Complete heart block
Consequence of a lack of O2 delivery to tissues?
Anaerobic respiration is 18x less efficient in terms of ATP production, without ATP the cells have no energy and die
On the macroscopic level this leads to organ dysfunction and failure
Does the absence of tachycardia rule out haemorrhagic shock?
No
30-35% of people present with initial bradycardia
Patients on b-blockers are pharmacolgically prevented from mounting a tachycardia
In some patients tachycardia may go unnoticed because their resting HR is low e.g. athletes
Why is resp. rate a good measure of perfusion?
Hypoperfusion >> metabolic acidosis >> RR increases to breathe off excess CO2
RR is often overlooked but is a very good clinical marker
How much circulating volume has to be lost before BP falls?
30-40%
Calculate MAP
= systolic BP + diastolic BP + diastolic BP / 3
What MAP is considered sufficient to maintain organ perfusion in a healthy adult?
65mmHg





