Stomach Flashcards
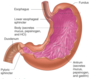
What happens when the bolus of food passes into stomach
Lower oesophageal sphincter hypercontracts to prevent reflux

What do specialised cells in the stomach do
Synthesise and secrete mucous fluid, enzyme precursors, HCl, hormones
What is responsible for gastric motility
Abundant SM in the stomach
Name for “food” in the stomach
Chyme
What secretes gastric juice
Cells of gastric mucosa
HCl (contained in gastric juice)
Cleans food
Protein digestion
Pepsinogen
Precursor to pepsin
Digests protein
Intrinsic factor
Vitamin B12 absorption in the ileum
Mucus
Protects gastric mucosa from acidic environment (H+ - pH 1-2)
PARIETAL CELLS
- Location
- Secretion
- Body
- HCl and intrinsic factor
CHIEF CELLS
- Location
- Secretion
- body
- Pepsinogen
G CELLS
- Location
- Secretion
- Antrum
- Gastrin INTO CIRCULATION
MUCOUS CELLS
- Location
- Secretion
- Antrum
- Mucus and pepsinogen
D CELLS
- Location
- Secretion
- Antrum
- Somatostatin
Why is gastrin unusual
Secretion is not into the lumen but into bloodstream
PARACRINE secretion
4 types of secretion
- EXOCRINE - outside of body (going to outer space)
- ENDOCRINE - with G cells (radio broadcast, signal to whole body but only people tuning in will listen to the message)
- PARACRINE - somatostatin (talking to the neighbours -conc of message decreases to the power of 3 as you move out from source - communicates 10 cells width)
- AUTOCRINE - acid secretion (singing to yourself)
What are gastric pits similar to
salivary gland
What are the pits lined with
Parietal cells
Chief cells
G cells
D cells
Mucus neck cells (secrete mucus and bicarbonate)
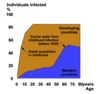
Where do regional differences exist
- Secretions near lower oesophagus/pyloric sphincter
- Secretions in rest of stomach
in the number of cell types lining a gastric pit
- Mucus, HCO3-
- Digestive secretions (H+, pepsinogen)
2 functions of HCl
- Clean food - make it aseptic, but becteria and viruses can still get through
- Denature proteins and break protein bonds
How is HCl secreted
At apical membrane, H+ is secreted into lumen of stomach via primary active transport
Cl- follows H+ into the lumen
However, at basolateral membrane, HCO3- is moved into interstitial space in exchange for Cl-

If the pH of the cell increases, what happens
Encourages the disintegration of carbonic acid to H2O and CO2
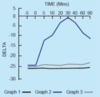
Stimulation of H+ secretion by gastric parietal cells
PNS stimulation starts at Vagus (Gs)
HISTAMINE is released from enterochromaffin-like cells in gastric mucosa, binds to nearby PARIETAL cells, binds to H2 receptor, Gs protein, cAMP, PKA increases ATPase activity
** ALL 3 involve PKA

What are ulcers
What was first used to treat it
Injury to gastric mucosa, with acid going into it
Atropine - muscarinic antagonist
Now omeprazole - directly inhibitd the H+ K+ ATPase pump
- reduces acid secretion, prevents acidic environment in the stomach, extremely effective against acid reflux