Respiratory physiology Flashcards
Whats the biochemical definition for cellular respiration?
The process in which nutrients are converted into useful energy in a cell
Whats the physiological defintion for gaseous exchange?
The process by which an organism exchanges gases with its environment- process and regulation
Whats are the roles of the respiratory system?
and how do these things occur?
- gas exchange
- regulation of blood (tissue) PH: altered by changing blood CO2 levels
- voice production: movement of air past vocal fold makes sound and speech
- Olfaction: smell occurs when airborne molecules are drawn into nasal cavity
- protection: against particles/ microorganisms by preventing entry and removing them
Label the respiratory system…


What are the two zones the respiratory system has and what included in these systems?
1. Conductive zone
- URT (upper respiratory tract)
- Tracheobronchial tree
2. Respiratory zone
- Resoiratory bronchioles to alveoli
- Site for gas exchange
Whats the roles of the nasal cavity?
- passage for air
- cleans the air
- humidifies, warms air
- smell
- acts along with paranasal
- sinuses (resonating chambers)
Whats the structure in the nose that causes turbulalce? What does this mean for keeping the nose/body healthy?
The Conchae causes turbulance of air (gives large surface area)
large particles are blocked from coming in
What do sinuses help with?
- lighten skull
- protection
Whats the pharynx and what are the regions of it?
The Pharynx is a common opening for digestive and respiratory systems
the three regions of the pharynx are;
- Nasopharynx
- Oropharynx
- Laryngopharynx
What are the functions of the larynx?
- maintain an open passageway
- Epiglottis and ventricular folds prevent swallowed material from moving into larynx
- vocal folds are the primary source of sound production
What are the unpaired cartilages of the larynx?
The thyroid, cricoid and epiglottis
What are the paired cartilages of the larynx?
The arytenoid, corniculate and cuneiforms
Whats the functions of the tracheobronchial tree ?
What must we ensure for correct function?
Functions:
- passageway for air movement
- ciliated for the removal of debris
For the correct function to occur you must ensure:
- Theres limited turbulance
- minimal size (dead space)
What does the trachea branch into and where does this lead?
Where is cilia lost in the traceobroncial and why?
The trachea branches into 2 bronchi, one to each lung
In the terminal bronchiole you lose the ciliated epithelium and get squamous epithelium instead which allow for gaseous exchnage with the blood
Label the alveoli?


Tell me the types of cells found in the alveoli and some of the properties/ roles?
1. Type 1 alveolar cells (septal cells)
- in contact with capillary
- simple squamous cells where gaseous exchnage occurs
2. Type 2 alveolar cells
- free surface has microvilli
- secrete alveolar fluid which contains surfactant
3. Alveolar dust cells
- macrophages also found in alveoli to remove debris
The lungs ‘float’ in the thoracic cavity because they are surrounded by a thin layer of what?
pleural fluid
Is the lung directly attached to any muscle?
no
The continual transfer of fluid into the lymphatic channel maintains a negative pressure between what?
The visceral surface of the lung pleura and the parietal pleural surface of the thoracic cavity
Label the muscles that are used for ventilation?


What are the passive elements of ventilation?
- elastic return in lungs
- elastic recoil of ribs
- surface tension in lungs
Whats are the types of pressure in the lungs and where are they found?
- Pleural pressure: pressure in the intrapleural space (always a slightly negative pressure)
- Alveolar pressure: pressure inside the lung alveoli
- Transpulmonary pressure: alveolar pressure- pleural pressure (force that tends to distend the alveoli)
Describe the changes in pressure in the lungs during inspiration and just after?
- the Barometric air pressure (PB) is equal to alveolar pressure (Palv) and there is no air movement
- increases thoracic volume results in increased alveolar volume and decreases alveolar pressure
- Barometric air pressure is greater than alveolar pressure and air moves into the lungs
- End of inspiration
- Decreased thoracic volume results in decreased alveolar volume and increased alveolar pressure
- alveolar pressure is greater than barometric air pressure, and air moves out of the lungs
Whats meant by compliance of the lungs?
Name some conditions that decrease the compliance
the ease in which the lungs and thorax expand
conditions which decrease the compliance: pulmonary fibrosis and pulmonary oedema (fluid in the lungs)
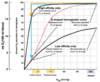
What is compliance altered by? Which one has the greatest effect?
- elastic fibres of the lung/chest
- elastic fibres caused by surface tension in alveoli (this has the greatest effect)
Whats surfactant and what’s it a mixture of?
Surfactant is an surface-active agent in water, gently reducing the surface tension of water
Surfactant is a mixture of:
- Dipalmitoyl phosphatidylcholine, (amphiphilic) (roughly 40%)
- Other phospholipids (roughly 40%)
- Surfactant apolipoproteins (SP-A, -B, -C, -D) (roughly 10%)
Whats surfactant formed in specifically?
Whats the secretion of surfactant regulated by?
Formed in lamellar bodies (LB) in type II alveolar cells
Secretion of surfactant is regulated by increased tidal volumes
What are the functions of the surfactant?
- Reduced work in inspiration (increases compliance). Results in 1/12 of the surface tension of a pure water air interface
- Stabilises alveoli (Laplace)
- Reduced alveolar pressure help keep alveoli dry; helps prevent pulmonary oedema
- Crucial for expansion of lungs at birth
Whats the definition of the following…
- Respiratory rate
- Minute ventilation
- Anatomic dead space (ADS)
- Alveolar ventilation (AV)
1. Respiratory rate: The number of breaths per minute
2. Minute ventilation: The amount of air moved in and out of the respiratory system per minute
Tidal volume (Tv) x Respiratory rate (RR)
3. Anatomic dead space (ADS): part of the respiratory system where gas exchnage does not take place (found in conducting zone and bronchioles is roughly 150 mls)
4. Alveolar ventilation (AV): Volume of air per minute entering the parts of the respiratory system in which gas exchnage takes place
(Tv - ADS) x RR
Whats partial pressure?
The pressure exerted by each type of gas in a mixture
Whats Dalton’s law?
Whats the general formula and then that to do with atmospheric gases?
total pressure = sum of partial pressure
Ptotal = P1 + P2 + P3 + …
involving atmospheric gases
P= pN2 + pO2 + PCO2 + pH2O
What are the 3 facotrs that changes the alveolar pressure of oxygen and carbon dioxide in the alveolus?
- Alveolar ventilation rate (v)
- increase Oxygen consumption and carbon dioxide production (exercise)
- Atmospheric pO2 and pCO2 alter with atmospheric pressure (altitude)
What does Fick’s law explain?
Whats the equation? and what each represent?
The diffusion of gases
Rate of diffusion: K x A x (P2 – P1)/ D
K= diffusion constant
A= area for gas exchange
P2 and P1= difference in partial pressures of gas on either side of diffusion barrier
D= distance (thickness of diffusion barrier)
What does the The respiratory membrane consist of ?
- layer of fluid lining the alveolus, containing surfactant
- alveolar epithelium
- epithelial basement membrane
- capiallary basement membrane (may fuse with epithelial basement membrane)
- capillary endothelium
What factors affect the rate of gas transfer?
- area for diffusion (emphysema) (area of functioning alveoli in contact with functioning capillaries)
- Thickness of path (here fluid path- cyctic fibrosis, pulmonary oedema, alveolar blocks)
- Changes in partial pressure difference over the memrbane (altitude etc.)
What are the causes that lead to an increase in pulmonary alterial blood pressure?
- the speed of blood transit through the pulmonary capillaries increases
- collapses vessels in the lungs to open so overall alveolar perfusion increases
What two factors are involved with the regulation of oxygen and carbon dioxide transfer between alveolus and blood? Tell me about the perfusion and ventilation in each part?
1. Rate of alveolar ventilation (v): upper parts of the chest are better ventilated but have a worse perfusion
2. Blood flow (perfusion) (Q): lower parts of the lungs are perfused better but have a worse ventilation
are all the alveoli ventilated and perfused equally?
no
What does the ventilation-perfusion rate provide?
a balance between the alveolar ventilation and alveolar blood flow
What are the special blood vessles surrounding alveoli in hypoxic conditions (low oxygen)?
- When pO2 within the alveoli decrease there is a decrease in blood flow to alveolus: this is called hypoxic vasoconstriction
- Oxygen sensitive K+ channels in the smooth muscle membrane of the pulmonary arteriole close, the cell depolarises so these arterioles partially close
- it is important in the pulomary circulation helping to match perfusion with ventilation
Whats Henry’s law?
concentration of dissolved gas= partial pressure x solubility coefficient
Tell me the colour changes of the Hb in oxygenation? and the equation to go alongside it
Hb (deoxyhaemoglobin: blueish) + O2 + HbO2 (oxyhaemoglobin:red)
Hb is a tatramer (4 molecules together) so what is Hb reaction with oxygen really like? (equation?)
Hb + 4O2 –> Hb(O2)4