Pulmonary Physiology Review Flashcards
Ventilation
Definition
How gases get into the alveoli.
Diffusion
Definition
How gases move across the alveolar walls into the blood or vice versa.
Perfusion
Definition
How blood vessels remove gas from the lungs.
Pulmonary Functions
- Gas exchange
- Metabolize certain compounds
- Filter small clots out of the blood
- Reservoir of blood
Conducting Zones
- first 16 generations including:
- trachea
- bronchi
- bronchioles
- terminal bronchioles
- do not contain alveoli = no gas exchange
- makes up the anatomical dead space (~150ml)
- serves to warm and humdify incoming air

Transitional & Respiratory Zones
- after the 16th generation including:
- respiratory bronchioles
- alveolar ducts
- alveolar sacs
- alveoli start to appear ⇒ gas exchange
- increased cross-sectional area ⇒ decreased resistance ⇒ increased flow ⇒ decreased velocity

Alveolar Structure
- Blood-gas barrier consists of:
- alveolar epithelia
- capillary epithelia
- associated basement membranes
- Contains:
-
Type I Pneumocytes
- Thin and flat
- comprise ~ 90% of alveolar surface area
-
Type II Pneumocytes
- smaller cells
- filled with lamellar inclusions
- contain pulmonary surfactant
- can transform into Type I pneumocytes if needed
- Macrophages present
-
Type I Pneumocytes

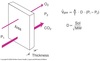
Pulmonary Vasculature
Lungs receive blood from two different sources:
-
Pulmonary circulation
- brings O2-poor venous blood via pulmonary arteries to blood-gas interface in alveoli
- O2/CO2 exchange occurs
- oxygenated blood travels via pulmonary veins to left-sided heart
- receives entire cardiac output (~5 L/min at rest)
- low pressure (~15 mmHg)
-
Bronchial Circulation
- part of systemic circulation
- supplies conducting airways
- comes from aorta and bronchial capillaries
- drain into:
- bronchial veins
-
anatomoses with pulmonary capillaries into veins of pulmonary system = physiological shunt
- Allows small amount of deoxygenated blood to enter systemic circulation
- Decreases pulmonary vein spO2 by 1-2%

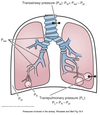
Pleural Pressure
( Ppl )
Pressure in the pleural fluid between the lung and the chest wall.
Subatmospheric at rest, approximately -5 cm H2O.
Due to inward elastic recoil of the lungs and outward recoil of the chest wall.

Airway Pressure
( Paw )
Pressure within the airway.
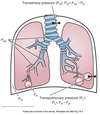
Alveolar Pressure
( PA )
Pressure inside the alveoli.
At rest with no airflow = 0 cm H2O.

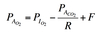
Transpulmonary Pressure
( PL )
Difference between the alveolar pressure and pleural pressure.
PL = PA - PPl
~ -5 cm H2O at rest

Transairway Pressure
( Pta )
Pressure difference across the airways.
Pta = Paw - Ppl
Responsible for keeping the airways open during forced expiration.
Tidal Volume
(VT)
The amount of air that enters and leaves the lung during quiet breathing.
~ 500 ml

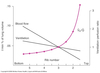
Total Lung Capacity
(TLC)
Total air capacity of the lungs.
~ 6 L
TLC = VC + RV
= IRV + VT + ERV + RV

Functional Residual Capacity
(FRC)
The amount of air remaining in the lungs after a tidal exhalation.
Cannot be determined by spirometry.
FRC = RV + ERV

Inspiratory Reserve Volume
(IRV)
The additional air brought in beyond the tital volume by deep inspiration.

Inspiratory Capacity
(IC)
The amount of air which can be brought in after a tidal expiration.
Sum of the tidal volume and IRV.

Expiratory Reserve Volume
(ERV)
The additional air beyond a tidal expiration which can be moved out due to deep exhalation.

Residual Volume
(RV)
The air that remains in the lung after a deep exhalation.
Cannot be determined by spirometry.

Vital Capacity
(VC)
The maximal amount of air that can be exhaled after a deep inspiration.
VC = ERV + VT + IRV

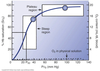
Spirometry
Measurement of the volume and speed of airflow under conditions of quiet breathing, maximal inspiration, and maximal expiration.

Helium Dilution Technique
Used to measure the residual volume and thus determine the FRC and TLC.
Helium insoluble in the blood so entire volume remains in the lungs.
C1 + V1 = C2 x (V1 + V2)
V2 = V1 x [(C1 - C2)/C2]
- Subject breaths in air containing known concentration of helium (C1).
- Amount of helium in the system before equilibrium mest be the same as after equilibrium with the lungs.
- If inspiration of He starts and ends at the end of a tidal breath, V2 = FRC
- If inspiration starts and ends with forced expiration, V2 = RV.

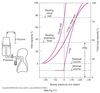
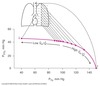
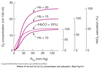
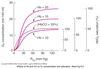
Rates of Airflow
Spirometry
Forced vital capacity (FVC) = air expired as rapidly as possible after a maximal inspiration ⇒ ~ 5 L in healthy adult male
FEV1 = volume of forced air expiration in 1 second
FEV1 / FVC = ratio of air expired over 1 second over the total ⇒ normal ~ 80%
Usually lung diseases involve mixed restrictive and obstructive patterns.
Ex. asthma.