Mycobacteria, Other AFB, Antimycotic Agents Flashcards
Mycobacteria
Morphology and Cultivation
- Slender, straight or slightly curved rods (1-4 cm)
- Colonies appear rough, granular, and buff-colored
- Some atypical mycobacteria are rapid growers
- Most very slow growing, including M. tuberculosis
- Generation time up to 18 hrs

Mycobacteria
Species

Mycobacterial Infection
Classification
-
Mycobacerium tuberculosis
- ~ ⅓ of world population infected
- Humans only known reservoir
- 85% of TB cases present with pulmonary sx
-
Mycobacterium avium-intracellular
- Atypical mycobacteria
- Ubiquitously found in fresh and salt water worldwide
- Usu. only infects immunocompromised pts
- Mostly pulmonary disease but also infects other tissues
-
Mycobacterium leprae
- Causes leprosy
- Infects skin and peripheral nervous system
- Very slow growing ⇒ progressive course over a long time
Mycobacteria
Properties
- Aerobic
- Bacillus ⇒ slender straight or curved rods
- Highly resistant to:
- Drying
- Many disinfectants
- Acids
- Alkalis
- Heat sensitive

Mycobacteria
Cell Wall
Lipids are 60% of cell wall structure
Inside ⇒ outside:
- Cytoplasmic membrane
-
Lipoarabinomannan (LAM)
- Anchored to cell membrane
- Functionally related to O-antigen of LPS
-
Murein ⇒ thick peptidoglycan layer
- 2 chains of alternating sugars linked by polypeptide chains
-
Arabinogalactan ⇒ polymer consisting of arbinose and galactose
- Attached to cell wall & mycolic acid chains
-
Mycolic acids ⇒ long alkyl chains
- Each arabinogalactan attached to 60-90 myolic acid chains
- Forms waxy protective lipid shell
- Additional lipids also present
- Reason for resistance to acid decolorization
- Do not take up dyes in gram staining
- Contributes to abx resistance
- Outer membrane of secreted phospholipids

Mycobacteria
Visualization
-
Ziehl-Neelson or Kinyoun stains ⇒ bacteria that retain the primary stain after decolorization are called acid-fast ⇒⇒ Mycobacteria called acid fast bacilli (AFB)
- Apply primary stain, carbol fuchsin
- Decolorize with acid alcohol
- Counterstain with methylene blue
- Visualize by fluorescent staining ⇒ Auramine-rhodamine

Tuberculosis
Epidemiology
- Globally:
- ~ 2.3 billlion Latent TB Infections (LTBI)
- ~ 9 million new active cases / yr
- ~ 1.4 million deaths / yr
- 22 countries have 80% of all TB cases
- USA:
- ↑ incidence since 1985
- Likely d/t AIDS epidemic
- ↓ since 1993
- TB control programs
- ↑ incidence since 1985

Tuberculosis
Transmission
- Via inhalation of mycobacteria in droplet nuclei
- ~ 3,000 in a single cough
- < 10 bacilli may initiate infection
-
Droplet nuclei dry and may become airborne
- Remains infectious for extended periods
Tuberculosis
Transmission Risk Factors
- Overcrowded areas
- Prisons
- Foreign born
- HIV-infection
Tuberculosis
Invasion
Facultative intracellular pathogens
- Ingested by alveolar macrophages
- Grow within non-activated MΦ and outside of them
- Prefers sub-pleural location near fissures
- Lesion development, progression, and resolution depends on:
- # of mycobacteria inhaled
- Subsequent multiplication
- Host immune response

M. tuberculosis
Virulence Factors
-
Facultative intracellular pathogen
- Able to grow within MΦ
-
Liproarabinomannan (LAM)
- ⊗ MΦ activation
- Scavenges oxygen radicals
- ⊗ Phagolysosome fusion
TB
Exposure
- ⊕ Contact with a person w/ contagious pulmonary TB
- ⊖ PPD skin test
- Normal CXR
- Some exposed persons develop infection w/ subsequent PPD conversion, others do not
Tuberculosis
Infection
- ⊕ PPD skin test
- No physical findings of disease
- CXR normal or reveals old granulomas or calcifications in lung or regional lymph nodes
- Requires preventative therapy
- 90% remain asymptomatic
- ~ 5% develop disease within 2 years of infection ⇒ primary TB
-
~ 5% develop disease at some later time ⇒ reactivation disease
- Usually d/t ↓ immune response with age, immunosuppressive disease, or therapy

Tuberculosis
Disease
Infected individual with signs, symptoms, and/or radiographic findings consistent with disease.
May be pulmonary and/or extrapulmonary.

Tuberculosis
Clinical Infection
Characterized as a chronic pneumonia.
Onset is insidious.
Primary TB is usually mild.
-
TB is an indolent, wasting, fibrile illness
- Chronic productive cough ± hemoptysis
- Fatigue
- Weight loss
- Night sweats
- Weakness
- Fever
TB
Primary Infection
Varies: completely asymptomatic → primary progressive disease
- Early during infection prior to immune response ⇒ organisms grow uninhibited @ pulmonary & additional sites
-
Tubercle or Ghon focus ⇒ productive granuloma caused by mycobacteria
- Center ⇒ multinucleated giant cells containing organism ± caseous necrosis
- Middle ⇒ epitheloid cells
- Outer ⇒ fibroblasts, lymphocytes, and monocytes
- Ghon complex ⇒ granuloma within the lung and within a draining hilar LN
- Granuloma may heal by fibrosis and calcification ⇒ lung scarring
- May result in lymphohematogenous spread throughout body & seeding of lung apices

Progressive Primary TB
- May directly result from lesion eroding into bronchioles ⇒ cavitation & dissemination within lung
- Lymphohematogenous spread ⇒ remote dissemination ⇒ miliary tuberculosis
- Child < 5 y/o @ high risk for progressive 1° TB

Secondary Pulmonary TB
Etiology
- Most cases d/t reactivation of latent TB
- Usually in apical portion of lung
- Leads to chronic pulmonary diseases w/ 1 or more productive lesions
- Associated with conditions that ⊗ immune system
- Alcoholism
- DM
- Old age
- Immunosuppressive therapy
- AIDS
- Can result from an exogenous secondary infection
- Exposed to TB again

Secondary Pulmonary TB
Manifestations
- Cough
- Fever
- Fatigue
- CXR ⇒ usually show upper lobe involvement with a cavitary lesion
- ± TB pleurisy w/ rupture of cavity or granuloma into pleural space ⇒ empyema
- Sputum smear and PPD usually ⊕

Miliary Tuberculosis
Dissemination and seeding of TB bacilli to various distant organs.
- Develop infectious foci in meninges, urogenital tract, peritoneum, skin, bones, etc
- Usually occurs in immunocompromised individuals
-
Most commonly occurs w/ primary infection
- Can also occur during reactivation
- Focal sx may be absent ⇒ difficult to dx
- PPD skin test often ⊖
- Communicability of miliary TB relatively low
- If lungs involved, CXR shows “miliary” pattern
- Clinical manifestations:
- Fever
- Night sweats
- Weight loss

Extrapulmonary TB
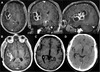
Meningitis
- Indolent onset HA with systemic sx
- CSF ⇒ PMNs early then lymphocyte predominance, low glucose, high protein
- Imaging ⇒ enhancement of basilar meninges

Extrapulmonary TB
Renal Disease
- Infection of renal parenchyma
-
Sx ⇒ dysuria, frequency, flank pain
- Fever and systemic sx uncommon
- Sterile pyuria ⇒ WBC in urine with no organisms
- Organism frequently grows from urine if repeated AFB urine cultures performed

Extrapulmonary TB
Bone Disease
- Spine affected in 50% of cases w/ bone involvement ⇒ Potts disease
- Hips and knees less affected
- Pts usually c/o pain
- ± Fever

Extrapumonary TB
Local LN Disease
- Most commonly occurs in children < 15 y/o
- Can be caused by M. tuberculosis or M. scrofulaceum
- Cervical lymph nodes most commonly involved ⇒ Scrofula
- Dx ⇒ excisional biopsy or fine-needle biopsy