Physiologic Mechanisms of Excitotoxicity Flashcards
What are two ions that are required for our survival?
- Calcium
- Oxygen
What are the different Excitatory Amino Acids (EAA)?
What are their precursors?
Where are they located?
- Glutamate
- Precursor: a-Ketoglutarate
- 2 pools: Metabolic and in the Axon Terminals! - Aspartate
- Precursor: Oxaloacetate
- Located in the VISUAL CORTEX and PYRAMIDAL cells (often found WITH Glutamate)
List the different Ionotropic receptors and their actions when activated.
- NMDA Receptor
- Activated by exogenous agent N-Methyl-D-Aspartate (NMDA)
- Also glutamate and Aspartate
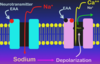
- when activated it allows Ca2+ INTO the cell
- Activation leads to Excitatory Postsynaptic Potential (EPSP); Slow ONSET (Can’t do anything because the Mg2+ has to get out of the WAY!!!) and PROLONGED duration (Ca2+) - Non-NMDA Receptors
- Almost ONLY on Post-Synaptic Membrane
- Na+ comes INTO the cell (*a little bit of Ca2+ can also enter)
- 2 Subtypes: AMPA and *Kainate
- AMPA have a Benzodiazepine site and if it binds it will INHIBIT the response to the Neurotransmitter!
- Activation leads to an EPSP
*** OFTEN co-localized at teh same synapse with NMDA receptors!

Why are the Non-NMDA and NMDA receptors in close proximity to each other on Post-Synaptic Membranes?
Have to depolarize the membrane in order for Mg2+ to leave the NMDA receptor and allow Ca2+ to come INTO the CELL!!!
What are some characteristics of Metaotropic Receptors in relation to Excitatory Amino Acids?`
On BOTH Pre-Synaptic and Post-Synaptic Membranes
- Pre-Synaptic: Tells the membrane that you have released the Neurotransmitters!
Describe the GENERAL functions of Excitatory Amino Acids when they bind to their receptors.
Major EXCITATORY system in the CNS
- Non-NMDA Receptors: Primary afferents, Premotor
- NMDA Receptors: Long-term changes in synaptic strength, learning, memory
- Metabotropic Receptors: Learning, Memory, and Motor Systems (“Motor Memory”)
How do you get rid of the EAAs from the synaptic Cleft?
- Neurons and Glia will UPTAKE the EAAs via a Na+ DEPENDENT 2 Active Transport (HIGH AFFINITY)
- GLIA will convert EAAs to GLUTAMINE (will NOT bind to any of the receptors) and release into the Extracellular Fluid
- NEURONS take Glutamine up and convert it back to GLUTAMATE
How is NO formed in relationship to EAAs?
What is the function of NO?
Calcineurin is going to ACTIVATE Nitric Oxide Synthase!
- Long-Term Potentiation and Memory
- Cardiovascular and Respiratory Control in the Brain
*** Can be VERY TOXIC! (Leads to production of Free Radicals)

Explain the phenomena of Excitotoxicity.
Over-Stimulation of the EAA system can cause cell death even in neurons that were not ischemic/hypoxic/anoxic.
What happens when you have an area in the brain that is subjected to Oxygen Deprivation? How does Oxygen Deprivation INCREASE cytoplasmic Ca2+ levels?
- DEPOLARIZATION of the Membrane due to a DECREASE in activity of the Na+/K+ ATPase
- Within 4 Minutes the ATP levels within the neurons will drop to 0
- Action Potentials are going to be INEVITABLE which will lead to the Release of Neurotransmitters (EAAs)
- HIGH EAAs for 2 reasons:
1. EAA release is excessive (due to APs)
2. EAA Re-UPTAKE will fail (Secondary Active Transport is dependent on SODIUM)
*** You will have ACTIVATION of NMDA receptors and have a HUGH INFLUX of Ca2+ INTO the cell!
What is going to happen when you have HIGH cytoplasmic Ca2+ levels in response to an Oxygen Deprivational event in the Brain?
- Activation of Phopholipase A2
- Releases Arachidonate from the membrane and causes PHYSICAL DAMAGE to the membrane
- ARACHIDONATE is going to bind to RYANODINE receptors on the ER and cause a RELEASE of Ca2+ from intracellular stores
- Causes the “Unfolded Protein Response” which will cause this cell to STOP making PROTEINS - Activation of Calcineurin (phosphatase)
- INCREASES NO synthesis! - Activation of mu-calpain (protease)
- Will undergo PROTEOLYSIS and effects SPECTRIN and eIF4G
- This will IMPAIR the REPAIR pathways of the cell and it will NOT be able to FIX itself - Activation of the apoptotic pathway
- Increase in cytoplasmic Ca2+ will cause the release of CYTOCHROME C and CASPASE 9 from the Mitochondria
- Activation of Caspase 9 will activate CASPASE 3 and these cell will DIE!

Explain the Reperfusion of O2 injury.
Oxygen is going to come back but it is used inappropriately and will be turned into FREE RADICALS which will damage the neuron further
*** Kinases will take the Remaining ATP and modify Enzymatic action through PHOSPHORYLATION
- Phosphorylation of eIF2a KINASE leads to a DECREASE in protein synthesis and ACTIVATES Caspase 3, which will INCREASE apoptotic signaling!
When given a case presentation about Oxygen Deprivation in the Brain and Increased Cytoplasmic Ca2+, which symptoms point to the involvement of Nitric Oxide?
Severe Swelling and Edema


