Pediatric ENT, Allergy, Immunology Flashcards
Acute epiglottitis may present with a muffled (“hot potato”) voice and inspiratory […].
Acute epiglottitis may present with a muffled (“hot potato”) voice and inspiratory stridor.
the presence of drooling helps differentiate epiglottitis from laryngotracheobronchitis (croup)

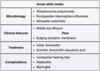
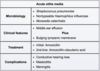
Acute otitis media often follows an […] infection.
Acute otitis media often follows an upper respiratory infection.
nasal congestion contributes to Eustachian tube inflammation and fluid accumulation in the middle ear space; other predisposing factors include cigarette smoke exposure, day care attendance, and formula feeds
Acute epiglottitis often presents with acute-onset fever, […], and dysphagia with respiratory distress.
Acute epiglottitis often presents with acute-onset fever, drooling, and dysphagia with respiratory distress.

Acute […] often presents with acute-onset fever, drooling, and dysphagia with respiratory distress.
Acute epiglottitis often presents with acute-onset fever, drooling, and dysphagia with respiratory distress.

C1 esterase inhibitor deficiency results in elevated levels of the edema-producing factors C2b and […].
C1 esterase inhibitor deficiency results in elevated levels of the edema-producing factors C2b and bradykinin.
results in hereditary angioedema
Can the rotavirus vaccine be administered to patients with a history of intussusception?
No (contraindicated)

Chronic granulomatous disease (CGD) is due to a defect in […] enzyme.
Chronic granulomatous disease (CGD) is due to a defect in NADPH oxidase enzyme.

Conditions causing […] deficiency predispose patients to chronic giardiasis.
Conditions causing IgA deficiency predispose patients to chronic giardiasis.
e.g. selective IgA deficiency, Bruton’s, CVID
Contraindications to the DTaP vaccine include history of anaphylaxis to vaccine ingredients, unstable neurologic disorders, and […] within a week of previous vaccine administration.
Contraindications to the DTaP vaccine include history of anaphylaxis to vaccine ingredients, unstable neurologic disorders, and encephalopathy within a week of previous vaccine administration.
patients with unstable neurologic disease or encephalopathy following vaccination should receive diphtheria and tetanus toxoids without pertussis (Td)

Contraindications to the DTaP vaccine include history of […] to vaccine ingredients, unstable neurologic disorders, and encephalopathy within a week of previous vaccine administration.
Contraindications to the DTaP vaccine include history of anaphylaxis to vaccine ingredients, unstable neurologic disorders, and encephalopathy within a week of previous vaccine administration
patients with unstable neurologic disease or encephalopathy following vaccination should receive diphtheria and tetanus toxoids without pertussis (Td)

In preterm infants, all vaccines should be administered according to […] age. (chronologic or gestational)
In preterm infants, all vaccines should be administered according to chronologic age. (chronologic or gestational)

Leukocyte adhesion deficiency is characterized by marked leukocytosis with […] predominance.
Leukocyte adhesion deficiency is characterized by marked leukocytosis with neutrophil predominance.
due to impaired adhesion of the marginated pool of leukocytes

Myringotomy with tympanostomy tube placement should be considered in children with > […] episodes of acute otitis media in 6 months or > […] episodes in 12 months.
Myringotomy with tympanostomy tube placement should be considered in children with > 3 episodes of acute otitis media in 6 months or > 4 episodes in 12 months.
Otitis externa is most commonly caused by infection with […].
Otitis externa is most commonly caused by infection with Pseudomonas aeruginosa.
Staphylococcus aureus is another common cause

Otitis media with effusion can be distinguished from acute otitis media by the lack of […] signs.
Otitis media with effusion can be distinguished from acute otitis media by the lack of acute inflammatory signs.
e.g. absence of fever and no bulging of the tympanic membrane
Patients with acute epiglottitis may […] the neck and maintain a tripod position, which is a sign of respiratory distress.
Patients with acute epiglottitis may hyperextend the neck and maintain a tripod position, which is a sign of respiratory distress.

SCID is characterized by absent […] cells and dysfunctional […] cells.
SCID is characterized by absent T cells and dysfunctional B cells.

The first hepatitis B vaccine should be administered when the newborn weighs > […] kg.
The first hepatitis B vaccine should be administered when the newborn weighs > 2 kg.
2 kg = 4 lb 6 oz; this is the only exception to the rule that preterm infants should receive vaccines according to chronologic age
What are the most common causative organisms (3) associated with acute otitis media?
Streptococcus pneumoniae, nontypeable Haemophilus influenzae, and Moraxella catarrhalis.
What imaging test/study may be used to confirm the diagnosis of laryngomalacia?
Direct laryngoscopy

What is the definitive treatment for severe combined immunodeficiency (SCID)?
Stem cell transplant
no concern for rejection; other options include antimicrobrial prophylaxis, IVIG, and sterile isolation

What is the first-line treatment for acute otitis media?
Oral amoxicillin
if infection reoccurs within one month, amoxicillin-clavulanic acid should be given to cover beta-lactamase resistant strains; children with mild symptoms (e.g. mild pain, low-grade fever, unilateral disease) may be treated with supportive care and observation
What is the likely diagnosis in a 8-month-old infant with low serum IgG and normal serum IgM/IgA?
Transient hypogammaglobulinemia of infancy
due to decreased maternally derived IgG by 3 - 6 months; usually resolves by 12 months of age
What is the likely diagnosis in a child that presents with ear pain with a bulging, erythematous tympanic membrane on otoscopic exam?
Acute otitis media
tympanic membrane bulging is the most specific sign of AOM; young children are predisposed to middle ear infections due to narrower and straighter Eustachian tubes

What is the likely diagnosis in a child that presents with ear pain, erythema, and discharge after swimming in an outdoor pool?
Otitis externa (“swimmers ear”)
loss of cerumen due to swimming or excessive ear cleaning can increase the risk

What is the likely diagnosis in a child that presents with persistent ear discharge, despite antibiotic treatment, with granulation tissue and skin debris visible on otoscopic exam?
Cholesteatoma
may be complicated by hearing loss, cranial nerve palsies, vertigo, and/or infection
What is the likely diagnosis in a child that presents with worsening purulent nasal discharge and facial pain one week after a viral URI?
Acute bacterial rhinosinusitis
viral URI is the most common predisposing factor

What is the likely diagnosis in an infant with chronic inspiratory stridor that worsens in the supine position?
Laryngomalacia
stridor typically peaks at age 4 - 8 months; occurs due to “floppy” supraglottic structures that collapse during inspiration

What is the most common cause of acute epiglottitis in unvaccinated children?
H. influenzae type B
incidence has decreased with vaccination; bacteria that are now typically involved include Streptococcus pneumoniae, Streptococcus pyogenes, or Staphylococcus aureus

What is the most common primary immunodeficiency?
Selective IgA deficiency

What is the recommended management for infants with laryngomalacia?
Reassurance
typically resolves by 18 months of age; rarely requires surgery

What is the recommended management for patients with chronic variable immunodeficiency (CVID)?
IV immunoglobulins

What is the recommended pharmacotherapy for otitis externa?
Topical antibiotics (e.g. fluoroquinolones)
the antibiotic must cover for Pseudomonas

What is the recommended treatment for acute bacterial rhinosinusitis?
Oral amoxicillin-clavulanic acid

Which complement deficiency results in increased risk for recurrent Neisseria infection?
C5-C9 (MAC) deficiency























