Pathophysiology Flashcards
(21 cards)
describe the control of breathing
- INCREASE pCO2 is the MOST potent stimulator of respiration
- Decrease p02 and pH

describe the generations in which gas exchange occurs
- Generation 0 to 16 = NO GAS EXCHANGE
- generation 17-23 = GAS EXCHANGE OCCURS
whats conditions increase air flow.
Most RESTRICTION is due to BRONCHIOLES
–> inflammation of bronchial epithelium = bronchitis
–> secretions from epithelium = asthma, infection, decrease cilia
–> constriction of smooth muscle = asthma
–> physical blockade = tumors, aspiration
air resistance is most impacted by…
- Radius of the airway (increase in resistance –> decrease in radius
- affected in ASTHMA and Bronchitis (medium sized bronchioles have highest resistance
describe the effects of parasympathetic activation on airway resistance
- Parasympathetic activation INCREASES (M3 activation) RESISTANCE
- affected in ASTHMA and muscarinic agonists
describe the effects of sympathetic activation on airway resistance
- Symapthetic activation DECREASES (Beta2 activation) RESISTANCE
- Affected by epinephrine and albuterol
- USED during emergency in acute asthma attack
what are the 3 disorders due to obstruction from conditions in the airway wall
- asthma
- acute bronchitis
- chronic bronchitis
obstructive disorders related to loss of lung parenchyma
- emphysema
obstructive disorders of the airway lumen
- bronchiectasis
- bronchiolitis
- cystic fibrosis
- acute tracheobronchial obstruction
- epiglottitis
- croup syndrome
describe the omposistion of the respiratory membrane
site of gas exchange
- COMPOSITION
- layer of fluid lining the alveolus containing surfactant
- alveolar epithelium
- epithelial basement membrane
- intersitial space
- capillary basement membrane
- capillary endothelial membrane
describe the lung interstitium
found within the respiratory membrane
- COMPOSITION: connective tissue, smooth muscle, lymphatics, capillaries, cells
- FIBROBLASTS: prominent cells of the interstitium that PRODUCE collagen and elastin –> distensiblity and elastic recoil of lungs
- Lung interstitium is very small under normal conditions but becomes ENLARGED with INFLAMMATORY CELLS and EDEMA FLUID –> interfere with gas exchange
describe the factors that affect gas exchange
- D = diffusion of gas across respiratory membrane
- delta P = partial pressure difference between alveoli and blood
–> affects in high altitude, restrictive lung disease, O2 mask
- A = surface area (affected in atelectasis, tumor)
- d = distance between the two sides of membrane (thickness)
–> affected in pulmonary edema, pneumonia

describe pleural effusion
- Commonly seen in CONGESTIVE HEART FAILURE
–> increased pulmonary venous hydrostatic pressure - from the visceral side
- decreased microvascular oncotic pressure
- Due to decreased pleural pressure (atelectasis) or blockade of lymphatic drainage (tumors)
describe restrictive pulmonary disorders
- result of DECREASED EXPANSION OF THE LUNGS due to alterations in the lung parenchyma, pleura, chest wall or neurmuscular function
- result of lung parenchyma disorders, pleural space disorder, INFECTION or INFLAMMATINO OF THE LUNG (PNEUMONIA)
Hypoxic pulmonary vasoconstriction (HPV)
- is unique to lungs
- mechanisms for automatic control of pulmonary blood flow distribution
–> MATCHES VENTILATION AND PERFUSION

describe the perfusion relationship
- Matching ventilation (V) to perfusion (Q) is important for ideal gas exchange (Average normal value of V/Q = .8)
- V/Q = infinity (DEAD SPACE - ventilation coming in but no blood flow around it (PE))
- High V/Q = decrease in blood flow but ventilation is still good
- Low V/Q = increase in blood flow but decrease ventilation
- V/Q = 0 (shunt) = abnormal alveoli ventilation, but blood flow still goes through (ASD, VSD)
what aspect can’t be measured by spirometry
- Residual volume cannot be measured by spirometry
obstuctive lung disease

Obstructive lung disease

Upper airway obstruction

Upper airway obstruction

restrictive lung disease
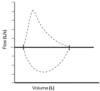
restrictive lung disease

describe clinical use of FEV1/FVC ratio
** USED TO DIFFERENTIATE AMONG LUNG DISEASES**
- FEV1/FVC = .8 –> NORMAL
- FEV1/FVC LESS .7 –> OBSTRUCTIVE LUNG DISEASE
–> FEV1 is DECREASED MORE than FVC
- FEV1/FVC INCREASED –> RESTRICTIVE LUNG DISEASE
–> both FVC and FEV1 are decreased, but FEV1 is decreased LESS than FVC


