Pathology-White Cell Disorders Flashcards
A 9 year old presents with persistent severe eczema and superficial skin pustules. Physical exam reveals lymphadenopathy. Labs show eosinophilia. Lymph node biopsy shows scattered rare large cells with prominent nucleoli in a background of normal appearing lymphocytes. What is your diagnosis?
Non-classic Hodgkin’s lymphoma.
What are causes of low white count?
Leukopenia is caused by marrow failure, aplastic anemia, chemotherapy, drugs, hyper or hypo cellular bone marrow and infections.
What are causes of a high white count?
Leukocytosis is caused by neutrophilia (infection/inflammation), eosinophilia (allergies, parasites, drugs, cancer), basophilia (CML), monocytosis (chronic infection, collagen vascular diseases), lymphocytosis (chronic infections, viral)
What are causes of leukemoid reaction?
Reactive leukocytosis can be caused by 30-50,000 granulocytosis (bacterial or myeloproliferative disease) or >10,000 lymphocytosis (viral, TB, sarcoid, leukemia or lymphoma)
What is the common abnormality of all the myeloproliferative diseases (CML/polycythemia vera)?
Abnormal tyrosine kinase
What does this indicate?

Doehle bodies are found in reactive neutrophils and are more commonly found in reactive diseases rather than neoplastic diseases.
What does this indicate?

This is reactive follicular hyperplasia. Note the sharp polarized mantle and “starry sky” appearance due to tingible body macrophages in the center of the lymph node gobbling up cells turning over in the germinal center.
A 14 year old girl comes to the clinic with a fever, sore throat and fatigue for the past month. On physical exam you note posterior cervical lymphadenitis. What would you expect to see on blood smear?
She has infectious mononucleosis from EBV. You would see atypical lymphocytes on blood smear because of the reactive T cell response to the viral infection.
What other virus follows a similar pattern as EBV?
CMV. It also will present as infectious mononucleosis.
A 14 year old girl comes to the clinic with a fever, sore throat and fatigue for the past month. On physical exam you note posterior cervical lymphadenitis. How did she get this condition?
EBV is transmitted orally. You 1st get IgM antibodies against the capsid, then you form IgG. Infection causes atypical (really large) cytotoxic T and NK lymphocytes activity against polyclonal B cell proliferation (hence the lymphadenopathy).
A 14 year old girl comes to the clinic with a fever, sore throat and fatigue for the past month. On physical exam you note posterior cervical lymphadenitis and hepatosplenomegaly. Her peripheral blood smear is shown below. Why do you think this is a reactive condition vs. a neoplastic condition?

Note the atypical lymphocyte skirting around the RBCs, this is not seen in neoplastic states, often seen in reactive states.
What are people with long-standing mono at risk for if they get into a car accident?
Spleen rupture. Splenomegaly thins the capsule wall and makes it more prone to rupture.
A 14 year old girl comes to the clinic with a fever, sore throat and fatigue for the past month. On physical exam you note posterior cervical lymphadenitis and hepatosplenomegaly. She is also on immunosuppressive therapy for juvenile arthritis. Her peripheral blood smear is shown below. What types of cancer is she at risk for?

EBV infection can cause a second hit mutation causing a translocation of 8:14 when patients are immunosuppressed. This can cause a proliferation of Burkitt lymphoma.

A kid gets scratched by a cat. Fine needle biopsy of his posterior cervical lymph nodes is shown below. What organism causes this and what is he at risk for developing?

The kid has Cat Scratch Disease from infection by Bartonella henselae. As the disease progresses you get stellate necrosis (shown below) in the lymph node germinal centers

Where are most neoplastic cells in leukemia?
Bone marrow and peripheral blood
Where are most neoplastic cells in lymphoma?
Lymph nodes
Where are most neoplastic cells in myeloma?
Bone marrow
Where are most neoplastic cells in Hodgkin’s disease?
Some in marrow, primarily in lymph nodes.
What precursor cells causes lymphoblastic lymphomas and leukemias?
Lymphoblasts (big immature B cells)

What precursor cells causes small lymphocytic lymphoma and chronic lymphocytic leukemia?
Naive B cells

What precursor cells cause mantle cell lymphomas?
Mantle cells.

Where do follicular, Burkitt, diffuse large B cell and Hodgkin’s lymphomas originate from?
Germinal centers

Where do diffuse large B cell, marginal zone and small lymphocytic lymphomas and chronic lymphocytic leukemias originate from?
Marginal zone

How do T-cells develop and progress in the thymus?
They start and double negatives, then they become double positive for CD4 and CD8. Then they mature into either a CD4 or CD8 T cells.
What precursor cells are responsible for precursor T lymphoblastic lymphomas and leukemias?
Immature ones that are double negatives or CD4 and CD8 positive.
What precursor cells are responsible fore peripheral T cell lymphomas?
Differentiated CD4+ and CD8+ T cells.
Where do eosinophils, macrophages, PMNs, platelets, erythrocytes, basophils, plasma cells, NK cells and T cells come from?
*

Two patients come to your office. One is 6 years old, the other is 86 years old. They both have symptoms of fatigue, fever and bone pain that was sudden onset. Labs show anemia. Peripheral blood smear on both of them reveals blasts. What diseases are in your differential at this point?
This sound like an acute leukemia. Acute leukemias are acute lymphoblastic leukemia (ALL) and acute myelogenous leukemia (AML).
A 40 year old woman comes in for a well check up. She says that she has felt tired recently. You order a CBC and see increased mature WBCs and anemia. What diseases are in your differential at this point?
She is presenting with a chronic leukemia. Chronic leukemias include chronic lymphocytic leukemia, small lymphocytic leukemia and chronic myelogenous leukemia.
Why are people with leukemia at increased risk for anemia, infection and hemorrhage?
Bone marrow failure causes defects in hematopoiesis
How do you diagnose leukemia?
Bone marrow biopsy.
A 6 year old child presents with sudden onset of fatigue, fever, petechial rashes and bone pain. Labs reveal abundant lymphoblasts and anemia. He is treated with chemotherapy and symptoms completely resolve. What was most likely causing his condition?
Acute lymphoblastic leukemia. This is the most common malignancy in children. B cell blasts fill up the bone marrow and cause thrombocytopenia, hence the petechial rashes.
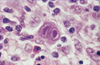
A 6 year old child presents with sudden onset of fatigue, fever, petechial rashes and bone pain. Labs reveal anemia. Peripheral blood smear is shown below. How do you determine if the cells shown below are leukemic lymphoid cells or myeloid cells?

Note the immature, large, high nuclear : cytoplasmic ratio and maintained round shape indicative of lymphoblasts. This kid has acute lymphoblastic leukemia. TdT+ = lymphoid cell line. CD19+ and CD22+ = B cell markers. CD10+ = common leukocyte antigen marker for immature cells. These are all assess with flow cytometry.
What CD markers tend to be T cell markers?
Those less than 10
A 6 year old child presents with sudden onset of fatigue, fever, petechial rashes and bone pain. Labs reveal anemia. Peripheral blood smear and flow cytometry is shown below.What cells are causing cancer in this child?

This is a flow cytometry reading. The lower left quadrant indicates negative for both markers. The upper right quadrant indicates positivity for both markers. This kid has cells positive for CD10/19, indicative of acute lymphoblastic leukemia.
What would you expect to see on bone marrow biopsy in a kid who has acute lymphoblastic leukemia?
Blast cells that completely fill the bone marrow.

What factors give you a worse prognosis for acute lymphoblastic leukemia?
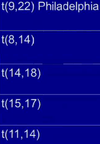
1) < 2 years old and > 10 years old 2) Peripheral blood blast count > 100,000 3) Philadelphia chromosome T(9,22), found in most adults, this is why adults do worse.
What factors give you a better prognosis for acute lymphoblastic leukemia?
1) 2-10 years old 2) Low WBC count 3) Hyperdiploidy 4) t(12,21)
What is the major risk associated with acute lymphoblastic leukemia?
The blast cells are so large that they get stuck in capillaries and cause infarction.

A 60 year old man presents with acute onset of fever, fatigue, bone pain and petechial rashes. He has had recurrent infections over the past few months. Labs reveal > 20% myeloid blasts in the bone marrow and anemia. What helps you differentiate between the different spectrums of his disease in the clinic?
Acute myelogenous leukemia is split up based upon where in the myeloid line the cancerous cells are coming from by the FAB classification. M0: minimal differentiation, M1: myeloblasts w/no maturation, M2 & M3 present with Auer rods, myeloblasts and promyelocytes, M4 & M5 present with mucosal bleeding, myelomonocytes and monocytes.

A 60 year old man presents with acute onset of fever, fatigue, bone pain and petechial rashes. He has had recurrent infections over the past few months. Labs reveal > 20% myeloid blasts in the bone marrow and anemia. You suspect AML. How do you differentiate AML from ALL when the bone marrow shows the hypercellularity below?
Myeloperoxidase stains for myeloid cells. TdT stains for lymphoid cells.
A 60 year old man presents with acute onset of fever, fatigue, bone pain and petechial rashes. He has had recurrent infections over the past few months. Labs reveal > 20% myeloid blasts in the bone marrow and anemia. What would you expect to see on higher power of this image?

AML shows myeloblasts with granules in the cytoplasm and prominent nucleoli.

A 60 year old man presents with acute onset of fever, fatigue, bone pain and petechial rashes. He has had recurrent infections over the past few months. Labs reveal > 20% myeloid blasts in the bone marrow, anemia and Auer rods on peripheral blood smear. How do you treat this patient?
You do not want to treat Acute Promyelocytic Leukemia (AML M3) with chemotherapy immediately because the Auer rods are peroxidase granules that have precipitated in the cytoplasm. If these are released into the peripheral blood, patients are at high risk for DIC. Acute Promyelocytic Leukemia happens as a result of the PML gene on chromosome 15 translocating to the retinoic receptor gene on chromosome 17, t(15;117). This blocks myeloid differentiation from the promyelocytic stage. If you give retinoic acid the neutrophils will mature, Auer rods will dissipate and then you treat with chemotherapy and the prognosis is good.

A 60 year old man presents with acute onset of fever, fatigue, bone pain and petechial rashes. He has had recurrent infections over the past few months. Labs reveal > 20% myeloid blasts in the bone marrow and anemia. Physical exam reveals gingival bleeding. Peripheral blood smear is shown below. What is causing this patient’s condition?
This patient has Acute Myelomonocytic Leukemia: M4/M5. These types have tissue invasion. Note that the cells on peripheral smear are more kidney bean shaped, differentiated, but still large.
What physical exam maneuver can you perform on a patient with Acute Myelomonocytic Leukemia?
Push on one of the skin lesions. The invasive infiltrates will have a green color for a few seconds due to the myeloperoxidase; this is called “Chloroma”.
A 50 year old woman presents with fatigue and recurrent infections. Physical exam reveals lymphadenopathy and hepatosplenomegaly. Labs reveal anemia, leukocytosis and peripheral blood smear and electron micrograph are shown below. What is causing this patient’s condition?

Chronic lymphocytic leukemia. Note the smudge cell on peripheral blood smear. This happens because the leukocyte loses its ability to apoptose and its membrane gets very thin. The cell “smudges” during slide preparation. Also note that the cell is much smaller, almost the same size as an RBC. He gets recurrent infections because B cells are not differentiating properly and causes a hypogammaglobulinemia.
Why do we group chronic lymphocytic leukemia with small lymphocytic lymphoma?
CLL and SLL are one spectrum of disease seen in 2 different places: CLL in the bone marrow w/islands of monomorphic cells and fat infiltration and SLL invades into tissues (shown below).

What are the main flow cytometry markers used to pick up acute lymphoblastic leukemia? Chronic lymphocytic leukemia?
ALL: CD10 & CD19. CLL: CD19, CD20, CD23 and an aberrant T-cell marker CD5

What cancer is rarely associated with autoimmune hemolytic anemia?
CLL and SLL.
Why is the survival rate for CLL and SLL only 4-6 years?
The cells have a slow turnover rate because they have lost their ability to apoptose.
A 50 year old woman presents with fatigue and recurrent infections. Physical exam reveals lymphadenopathy and hepatosplenomegaly. Labs reveal anemia, leukocytosis and peripheral blood smear and electron micrograph are shown below. What are late complications of this disease?

This patient has CLL/SLL. This can cause skin lesions and transform to a diffuse large B cell lymphoma in 10% of patients and some may transform to acute lymphoblastic leukemia.
A 50 year old man presents with fatigue and recurrent infections. Physical exam reveals lymphadenopathy and massive splenomegaly. Labs reveal anemia, pancytopenia and a dry tap on bone marrow biopsy. What markers do you ask the lab to run for this patient? What is his prognosis?
This patient has a dry tap on bone marrow biopsy, indicating bone marrow fibrosis. This is characteristic of Hairy Cell Leukemia. Markers for this are CD11C, CD25 and CD103. Note that this has a good prognosis with chemotherapy.
A 50 year old man presents with fatigue and recurrent infections. Physical exam reveals lymphadenopathy and massive splenomegaly. Labs reveal anemia, pancytopenia and a dry tap on bone marrow biopsy. Peripheral blood smear is shown below. What is your diagnosis?

Hairy Cell Leukemia. Note the cytoplasmic projections coming from the cells that would otherwise look like the cells seen in CLL.
A 50 year old woman presents with fatigue and recurrent infections. Physical exam reveals lymphadenopathy and massive splenomegaly. Labs reveals increased mature metamyelocytes (basophils, neutrophils and eosinophils shown below) w/WBC over 100,000. What is the prognosis for this patient?

This patient has chronic myeloblastic leukemia. This is caused by c-abl gene from chromosome 9 translocating to the bcr gene on chromosome 22 t(9;22), forming the Philadelphia chromosome, which creates an abnormal tyrosine kinase. 70% of these end in “blast crisis” AML and 30% end in ALL.

A 50 year old woman presents with fatigue and recurrent infections. Physical exam reveals lymphadenopathy and massive splenomegaly. Labs reveals increased mature metamyelocytes w/WBC over 100,000 and anemia. What would you expect to see on bone marrow biopsy?
This patient has CML. This presents with hypercellularity in the bone marrow, you would also see atypical megakaryocytes within the marrow..

What are the common myeloproliferative disorders?
These are from hyper-proliferative neoplastic myeloid precursor cells, caused by mutated tyrosine kinase or JAK2. Diseases include: CML, polycythemia vera and myelofibrosis.
What are the lymphoid leukemias? What are their markers?
ALL (TdT +, B cells: CD19, 20, 21, T cells: CD3, 4, 8) and CLL/SLL (B cell: CD19, 20 and T cell CD5)
What are the myeloid leukemias?
AML and CML
A 15 year old boy presents with SVC syndrome and a superior mediastinal mass. What is your diagnosis? What is his prognosis?
T cell ALL. This has a poor prognosis.
What are the three main classes of lymphomas?
Non-Hodgkin’s Lymphoma, Hodkin’s Lymphoma and Multiple Myeloma.
A 30 year old man presents with generalized fatigue. Physical exam reveals multiple peripheral swollen lymph nodes. Lymph node biopsy shows expanded mantle around the germinal center. What is causing this patient’s condition? What is his prognosis?
Non-Hodgkin’s Lymphoma typically presents with few symptoms. This is a mantle lymphoma, note the expanded mantle on lymph node biopsy. This is due to a t(11,14). The prognosis is poor.
A 24 year old man presents with fever, night sweats and 15 pound weight loss. Chest x-ray reveals mediastinal adenopathy. Biopsy is shown below What is the most likely disease? How do you confirm this? What is his prognosis?
Hodgkin’s Lymphoma. You test for classic Hodgkin’s lymphoma with CD15 and CD30 markers, non-classic Hodgkin’s lymphoma does not have these markers. The patient will have a good prognosis if there are more lymphocytes and fewer Reid-Sternberg Cells (owl’s eye cell in biopsy).
What are 50% of Hodgkin’s lymphomas associated with?
EBV
3 patterns seen in N-H lymphoma
Follicular (B cell), diffuse (80% B cell, 20% T cell) and mantle (B cell) pattern

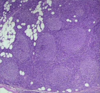
A 60 year old man presents with generalized fatigue. Physical exam reveals multiple peripheral swollen lymph nodes. Further labs reveal a very aggressive B cell lymphoma; however, it is very curable if caught early due to the high rate of cell turnover. Lymph node biopsy is shown below. What is your diagnosis?

This man has a diffuse N-H lymphoma, note the smooth lymph node. This is due to a t(14;18): 30% of which have BCL2 and 30% have BCL6 re-arrangements.
What is a common extra-nodal site for mantle cell lymphomas?
GI tract
A 30 year old man presents with generalized fatigue. Physical exam reveals multiple painless peripheral swollen lymph nodes. Lymph node biopsy shows proliferation of follicles without mantles. What is causing his condition? What is his prognosis?
Note the follicle proliferation without mantles; this is a follicular N-H lymphoma. This is due to t(14;18) bcl-2 expressing mutation and prevents apoptosis. Note that this is the most common adult N-H lymphoma and is difficult to cure due to its indolent nature.
What is your differential for a patient with N-H lymphoma?
SLL (tissue invasive), Lymphoblastic lymphoma (T-cell ALL seen in teenage males) and Burkitt lymphoma (starry sky appearance seen in kids)
A 7 year old girl presents with intussusception. Imaging reveals a leading GI mass. Lymph node biopsy is shown below. History reveals previous infection by EBV. What is causing her condition? What is her diagnosis?

This is the USA variant of Burkitt lymphoma, caused by t(8,14) that causes c-myc to move next to the heavy chain Ig on 14. This causes cells to turn over very rapidly and germinal center macrophages are very active, which causes the starry sky appearance. Prognosis is good for Burkitt lymphoma with chemotherapy because the tumor cells turn over so quickly.
A 7 year old girl presents with a maxillary/mandibular mass. Lymph node biopsy is shown below. History reveals previous infection by EBV. What is causing her condition?

This is the endemic African variant of diffuse N-H lymphoma.
A 60 year old man presents with generalized fatigue. Physical exam reveals multiple peripheral swollen lymph nodes. Further labs reveal a very aggressive B cell lymphoma; however, it is very curable if caught early due to the high rate of cell turnover. What would you expect to see on biopsy?
This man has diffuse N-H lymphoma. This presents with large B cells with prominent nucleoli and large nuclei.

What are the most common lymphomas in kids? In adults?
Kids: 1/3 lymphoblastic lymphomas (T cell ALL), 1/3 Burkitt’s lymphoma, 1/3 diffuse large B cell lymphoma. Adults: 50% diffuse large B cell lymphoma, 50% follicular N-H lymphoma.
Hodgkin’s lymphoma owl’s eye variants
Lacunar and popcorn
Compare the classic Hodgkin’s lymphomas in these categories: R-S cells, EBV, Markers, Background cells, prognosis and differentiating factors.

You always have to look at the background when differentiating these.

How does non-classic Hodgkin’s lymphoma differ from the classic type? How are they similar?
Classic: lymphocyte rich; Non-classic: lymphocyte predominant. Classic: CD15, 30 +, Non-classic: CD15, 30 - & CD20, BCL6 +. Classic: most EBV +, Non-classic: EBV -. Classic: R-S owls eye, Non-classic: L+H RS cells (lymphocyte and histolytic variants and popcorn cells)
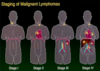
What determines staging of Hodgkin’s lymphomas?
Stage I: 1 LN above diaphragm. Stage II: 2 separate LNs above diaphragm. Stage III: LN below diaphragm. Stage IV: more LNs than III.
A patient presents with a broken skull. He also has renal failure, increased infections and anemia. Labs reveal hypercalcemia and light chain immunoglobulins in the urine. What would you expect to see on histological analysis of this patient’s blood and bone marrow?

This patient has a plasma cell dyscrasia: Multiple myeloma. This is the most common bone tumor in adults and presents with hypercalcemia from bone destruction and Bence Jones proteins in the urine from kidney damage. On histological analysis you would see mature plasma cells w/inclusion bodies. On peripheral blood smear you would see RBCs sticking to each other (Rouleaux formation).

What type of Hodgkin’s lymphoma is this?

Mixed cellularity. Note the “owl’s eye” R-S cells on a background of eosinophils and
What type of Hodgkin’s lymphoma is this?

Non-classic Hodgkin’s lymphoma. Note the lymphocyte predominance behind R-S cells.
A patient comes to see you after a broken vertebra. He also has renal disease, increased infections and anemia. Labs show light chain immunoglobulins in the urine and What is causing his condition? What immunoglobulins are involved?
He has multiple myeloma. Waldenstrom’s macroglobulinemia: IgM precipitates in the cooler regions of the body. Also 55% of inclusion bodies are IgG and 25% are IgA.
A 20 year old woman presents with difficulty breathing. CXR shows multiple nodules in the upper lungs and a pneumothorax. Biopsy of the lung and EM are shown below. What stain do you do to confirm her contain?

Note the Birbeck granules (tennis rackets) on EM and eosinophils. She has Langerhans Cell Histiocytosis, a disorder of Histiocytosis X. This disease is characterized by high levels of eosinophil infiltrate and neoplastic Langerhans cells. These cells have a specific marker, CD1.
Match the chromosomal translocation with its appropriate disease:
*



