:P Flashcards
(55 cards)
the muscles in the pharynx are innervated by which nerve, except for the stylopharnygeal muscle - which is innervated by which nerve?
- all pharynx muscles innervated by: vagus nerve
EXCEPT:
- stylopharyngeus muscles which is innervated by the glossopharyngeal nerve (CNIX).
what is the migrating motor complex?
where can it originate?
what is its functions? (2)
migrating motor complex: propagating contractions every 90-120 mins. 3 phases
- *originates**:
a) stomach - vagus dependent
b) small intestine - vagus independent
functions:
a) clear undigested material
b) prevents bacteria overgrowth
what anatomical features of the colon ensure that peristalsis is modified? [2]
how does bolus move along colon? (2)
what anatomical features of the colon ensure that peristalsis is modified?
- get bulges of outer circular muscle (haustra), which are held together by three bands of circular muscle: taenia
- taenia can contract in either direction
how does bolus move along colon? (2)
- constrictive ring occurs (giant migrating concentration) and haustra disappear (!) from a portion of the ascending colon
~20cm of the colon distal to the constrictive ring lose their haustrations and contract as a unit, propelling faecal material into the transverse colon
cardia and pyloric mucosa:
- where find?
- cell types?
- function?
- what are nuclei like?
cardia and pyloric mucosa:
- *- location**
i) cardia: start / oesph -> stomach
ii) pyloric: end / stomach -> duo
- cell types: columnar epithelium - mucous secreting cells
- function: protec the oesphageal epithelium and pyloric mucosa against gastric juices
- nuceli: small & close to basal domain
Q
sensory innervation of the pharynx is from which nerve?
what are the constrictor muscles called in pharynx? - innervated by?
sensory innervation of the pharynx is from glossopharnygeal nerve
constrictor muscles: superior, middle and inferior constrictors. **vagus nerve innervation
_baso:
- sensory innervation = CNIX
- motor inneration = CNX_**
- which nerve plexuses do u find in the oesphagus? (2) and where do find them?
- *- meissner plexus:** submucosal tissue
- *- auerbach’s plexus:** myenteric - betweeen circ and long. muscle layer
(in the whole body): rank antibodies in their order
IgG most common 75% of Ig are IgG
IgM 3rd most common but 1st to be made
IgA 2nd most common
IgD very low
IgE least common in serum as binds tightly to basophils and mast cells even before interacting with antigen
name of the sphincter muscle which encircles the mouth:?
name of the sphincter muscle which encircles the mouth: orbicularis oris
in the anal and rectal area what are the different cell types in:
colorectal zone?
anal transitional zone?
squamous zone?
in the anal and rectal area what are the different cell types in:
colorectal zone: simple columnar epi
anal transitional zone: transition betwen simple columnar and and stratified squamous epi
squamous zone: stratified squamous
which part of muscaluris muscosa
- becomes internal anal sphincter?
2 extends over sphincter & attaches to CT? - becomes external anal sphincter?
which part of muscaluris muscosa:
circ muscle: becomes internal anal sphincter
long muscle: extends over sphincter & attaches to CT
skeletal muscle: external anal sphincter
which hormone is released when have hypocalcemia?
what is it effects? (3)
what is 1. inhibited by?
fall in calcium: PTH (parathryoid hormone) rises - restores calcium back to normal by:
- Increased renal Ca++ reabsorption.
- Increased bone Ca++ release.
- Increased gut absorption via release of vitamin D (1,25vitD).
The release if PTH is inhibited by raised Ca++ levels.
what is the differnece in the role of the intrisic and extrinsic muscles of mouth?
intrinsic muscle: change shape
extrinsic muscle: change position
orbicularis oris and buccinator are both innnervated by which nerve? [1]
orbicularis oris and buccinator are both innnervated by facial nerve [1]
Q
which antibody is commonly (1/200) deficient?
why is this very often not recognised?
A
IgA deficiency is quite common, yet no one knows they have it.
This is because IgM has a J chain so IgM undergoes a compensatory response and does the same job IgA would
what are two seperate roles of aldosterone? [2]
- restores BP, reabsorbed salt & water lvls (not excrete as much)
- restores K loss !
(two totally differnet systems! )
which muscles of mastiication are involved in:
a) elevation and retraction?
b) elevation and protrusion?
c) depression and protrusion?
d) elevation and protrusion?
a) elevation and retraction: temporalis
b) elevation and protrusion: masseter
c) depression & protrusion: lateral pterygoid
d) elevation and protrusion: medial pterygoid
Q
what is the special and general sensory innervation for the a) anterior 2/3 tongue? b) posterior 1/3 tongue
- *a) anterior 2/3 tongue**
- special: facial -> chorda tympani
- general: lingual nerve (V3)
- *b) posterior 1/3 tongue**
- special: glossopharyngeal
- general: glossopharyngeal
what are the two groups of muscles in the tongue?
how do they move the tongue?
innervated by?
- two groups: intrinsic (superficial) & extrinsic (deep)
- *- intrinsic** changes shape
- extrinsic changes position
- both innervated by hypoglossal nerve (CN XII)
IgD
- role?
- shape??
- how common?
- contains?
IgD
- role: antigen receptor on B cells that have not been exposed to antigens.
- activates basophils and mast cells = make antimicrobrial factors
- *- activates B cells**
- how common: very low levels
describe the structure of IgA and IgM - how many binding sites do they have?
what do they both contain?
IgA: dimer !! (know this) - can form 4 binding sites
IgM: pentamer - can form 10 bindings sites
= form multimers
- both have J chain: (The joining (J) chain is a small polypeptide, expressed by mucosal and glandular plasma cells)
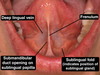
submanidublar gland recieves parasympathetic innervation from which nerve?
- submanidublar gland recieves parasympathetic innervation from facial nerve (CN VII) nerve
how does pit. gland control FSH & LH hormone release?
why is it more complex in women then men?
hypothalamic hormones: GnRH + kisspeptin
regulate release of: FSH and LH from pituitary.
FSH & LH cause sex steroid release (testosterone / oestrogen) , ovulation, spermatogenesis.
in women: estradiol +ve and -ve feedback depends on stage of menstruation
name for the muscle that causes upper oesphapgeal sphincter? [1]
- is produced by which skeletal muscle: cricopharyngeus muscle
- in the small intestine, enzymes are secreted by small intestinal cells called?
- what are the folds called in the small intestine?
- what are the main histological feature of small intestine? (2)
- what are the lieberkuhns crpyts?
- in the small intestine, enzymes are secreted by small intestinal cells called enterocytes
- what are the folds called in the small intestine: plicae circularis
- what are the main histological feature of small intestine: villi (projections of the mucosa) & microvilli
4. lieberkuhns crpyts: gland found in between villi