Obstetric Haemorrhage - Antepartum, Intrapartum, Post-partum Flashcards
What is an antepartum haemorrhage?
Haemorrhage from 24 weeks gestation until onset of labour
What is the definition of intrapartum haemorrhage?
Haemorrhage from onset of labour until the end of the second stage of labour
What is postpartum haemorrhage?
Haemorrhage from third stage of labour until the end of puerperium
Management of PPH
Depends on cause
- Tone: Oxytocin and ergometrine (initiates rhytmic contractions of uterus)
- Tissue: Manual evaculation in theatre
- Thrombin: FFP/Platelets/Cryoprecipitate
- Trauma: Suturing
Rarely needed to stop bleeding - balloon tamponade, uterine packing, uterine arteru embolization or ligation, hysterectomy
In the management of primary PPH/massive obstetric haemorrhage, what dose of oxytocin would you give, and at what rate?
Slow IV injection (5IU)
OR
30 IU in 500 ml saline - 125ml/hr
Difference between primary and secondary PPH
- Primary - within 24 hours of pregnancy
- Secondary - within 6 weeks of delivery (24 hours - 6 weeks)
What is a primary post-partum haemorrhage?
Blood loss of >/= 500 ml from the genital tract occuring within the 24 hrs of delivery
(Or >1litre if C-section)
What are causes of primary PPH?
4 T’s - Tone, tissue, trauma, thrombin
- Uterine atony (80%)
- Genital tract trauma
- Coagulation disorders
- Large placenta
- Abnormal placental site
- Retained placenta
- Uterine inversion
- Uterine rupture
Risk factors of atony
- Polyhydramnios
- Multiple gestation
- Prolonged labour
- Excess oxytocin
(normall tone of uterus compresses the blood vessles with it and reduces blood flow)
What is the most common cause of primary PPH?
Uterine atony (90%)
What is uterine atony?
Failure of uterus to contract effectively after delivery, which can lead to an acute hemorrhage, as the uterine blood vessels are not sufficiently compressed

What can cause uterine atony?
- Overdistended uterus
- Prolonged labour
- Infection
- Retained tissue
- Failure to actively manage 3rd stage labour
- Placental abruption
What gential tract trauma can lead to primary PPH?
- Tears
- Episiotomy
- Lacerations of the cervix
- Rupture of the uterus
What problems with placental site can increase the risk of primary PPH?
- Placenta praevia
- Placenta accreta
- Placenta percreta

What are antenatal risk factors for PPH?
- Previous PPH
- Previously retained placenta
- Increasedd BMI
- Para 4 or more
- Antepartum haemorrhage
- Overdistention of uterus
- Uterine abnormalities
- Maternal age >35 yrs
What are intrapartum risk factors for PPH?
- Induction of labour
- Prolonged 1st, 2nd, 3rd stage
- Use of oxytocin
- Precipitate labour
- Vaginal operative delivery
- C-section
How would you manage someone with uterine atony?
- Phyical methods to contract - bimanual compression, massage
-
Medical management
- 500 mcg ergometrine IV
- 30 IU oxytocin infusion
- Consider 250 mg Carboprost
- Consider 800 mg misoprostol PR - if bleeding continues
- Surgical management
What is the general principles to PPH management?
- Supportive - oxygen, fluids, blood
- Empty uterus - deliver foetus, deliver placenta
- Repair genital tract damage
- Treat atony - Massage, bimanual compression, medications
What are the pharmacological options in the management of PPH?
- Oxytocin - slow injection or IV infusion (30 IU in 500ml saline at 125ml/hr)
- Synometrine/ergometrine IM
- Carboprost IM 250mcg every 15 minutes - max 2 mg
- Misoprostol
- Tranexamic acid
In management of PPH, what dose would you give of ergometrine?
500 mcg
What dose of carboprost would you consider using in the management of PPH?
250 mcg
How would you administer carboprost and at what rate?
IM injection at 15 minute intervals
What is the maximum dose of carboprost you should give when managing PPH?
2mg - up to 8 IM injections
What dose of tranexamic acid would you consider giving someone to control PPH?
1g
What are causes of antepartum haemorrhage?
- Unexplained
- Placenta praevia
- Placental abruption
-
Local genital tract lesions
- Cervical erosions/ectropion
- Cervical polyps
- Vasa Praevia
- Cervical Carcinoma
- Cervicitis
- Vulval varicosities
APH of unkown origin is approx 97%
- Anticoagulants
- Bleeding diathesis
What is placenta praevia?
When the placenta is inserted, wholly or in part, into the lower segment of the uterus
What is grade I placenta praevia?
Placenta is encroaching on the lower segment but not the internal cervical os

What is grade II placenta praevia?
Placenta reaches the internal os
What is grade III placenta praevia?
Placenta eccentrically covers the internal os
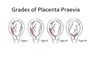
What is grade IV placenta praevia?
Central portion of the placenta covers the internal os

What grade of placenta praevia is the following?

Grade I
What grade of placenta praevia is the following?

Grade II
What grade of placenta praevia is the following?

Grade III
What grade of placenta praevia is the following?

Grade IV
What can increase the risk of developing placetna praevia?
- Prev history of C-section
- Multiparity
- Multiple pregnancy
- Mother > 40 years
- Assisted conception
- Fibroids
- Endometritis
What are symptoms of placenta praevia?
-
Painless PV bleeding after 24 weeks
- Usually small bleeds first
- May have feautres of heavy bleeding
- Uterus non tender, abnormal lie
Why does bleeding occur in placenta praevia?
Due to separation of the placenta as the lower uterine segments form and the cervix effaces - can occur from venous sinuses in lower segment
What must you remember when considering to do a vaginal examination on someone with antepartum haemorrhage caused by suspected placenta praevia?
DO NOT DO A VAGINAL EXAMINATION
How would you investigate suspected placenta praevia?
Abdo ultrasound/Transvaginal ultrasound
(Tends to be found incidentally on routine 2nd trimester scan)
How would you manage someone with placenta praevia?
Major placenta praevia
- Consider hospital admission from 34 weeks gestation
- Delivery by C-section - if edge of placenta is <2cm from internal Os, especially if posterior or thick
What is regarded as minor placenta praevia?
Grade I/II
(if leading edge is in lower segment but not covering os)
What is regarded as major placenta praevia?
Grade III/IV
(placenta covers internal os of the cervix)
What are causes of intrapartum haemorrhage?
- Placental abruption
- Placenta Praevia
- Uterine rupture
- Vasa praevia
What is placental abruption?
Defined as retroplacental haemorrhage and usually involves some degree of placental separation from uterine wall

Types of placental abruption
- Revealed - major haemorrhage
- Concealed - haemorrhage between placenta and uterine wall
- Mixed
What is placental abruption more common in?
- Pre-eclampsia/chronic hypertension (common)
- Multiparity
- Multiple pregnancy
- Increased maternal age
- Previous abruption
- Polyhydramnios
- Smoking
- Cocaine use
-
Trauma
- RTA
- Domestic violence
- Iatrogenic
What is the foetal consequence of placental abruption?
Separation results in reduced gas exchange between foetus and mother, predisposing foetus to hypoxia and acidosis
What is important to remember in relation to the amount of blood PV in the context of placetnal abruption?
May not reflect the total blood loss - may have considerable blood collection in retroplacental space without external loss - known as a concealed abruption
How would you distinguish placental abruption from placenta praevia asa a cause of antepartum haemorrhage?
- Shock out of keeping with visible loss
- Pain constant
- Tender, tense uterus
- Normal lie/presentation
- Foetal heart distressed/abnormal
- Coagulation problems

What is the following type of abruption classified as?

Partial revealed/apparent abruption
What type of abruption is the following?

Complete concealed haemorrhage
What type of abruption is the following?

Partial concealed abruption
What are symptoms of placental abruption?
-
PV bleeding - can be disproportionate with extent of bleed
- Spotting
- Light
- Moderate/severe
- Pain/abdominal tenderness - constant
- Dizziness
- Fetal HR absent/distressed
- Beware pre-eclampsa, DIC, anuria
What are clinical signs of placental abruption?
- Signs of shock - Tachycardia, hypotension, pale, clammy, sweaty
- Tender, tense uterus - hard woody uterus
- Normal lie/presentation
- Distressed foetal HR
- Obvious bleeding
In terms of distinguishing between placental abruption and placenta praevia, what would be the difference in terms of palpation of the uterus?
Uterus would be soft anf non tender in praevia, whereas it would probably be hard and painful/tender/tense in abruption
How would you investigate someone with suspected abruption?
- Bedside - Observations, Foetal CTG
- Bloods - FBC, Crossmatch and group and save, coag screen, Kleihauer test
- Imaging - Abdominal ultrasound + speculum examination (if no sign of praevia), Umbilical artery doppler
How would you manage someone with placetnal abruption?
Depends on clinical picture - could just rest and close supervision of foetal growth
- ABCDE - assess need for O2, fluids/blood resus
- Admit for observations, USS scan, CTG
- Consider delivery - C-section
What are complications of placental abruption?
- Maternal shock/collapse
- Foetal death
- Maternal DIC
- Renal failure
- PPH - couvelaire uterus
What is vasa praevia?
Occurs when the umbilical cord vessels run in the foetal membranes and cross the internal os of the cervix. These vessels may rupture in early labour and this often leads to reapid foetal exanguination

What aspects of the history are particularly important to ask about in antepartum haemorrhage?
- Gestational age
- Amount of bleeding
- Causative factors
- Abdominal pain
- Foetal movements
- Date of last smear
- Previous episodes of PV bleeding
- Previous uterine surgery
- Illegal drugs
- Blood group/rhesus status
- Previous obstetric history
- Position of placenta on last scan
What specifically would you examine when assess a mother with antepartum haemorrhage?
- BP
- Pulse
- Other signs of haemodynamic compromise
- Uterine palpation - size, tenderness, foetal lie, presenting part
When should you never perform a VE?
If placenta praevia has not been axcluded as the cause of bleeding
What is cervical shock?
Vasovagal syncope produced by stimulation of the cervical canal during dilatation may occur
What must you remember about vaginal exams?
No PV until no PP
(No vaginal exam post 24 weeks)
What’s placenta accreta?
When placenta abnormally attached to myometrium - high risk of placenta accreata in a women with placenta praevia and a previous C section
Key diffrences between placental abruption and placenta praevia
-
Placental abruption
- Shock out with keepin with visible loss
- Pain, constant
- Tender, tense woody uterus
- Normal lie and presentation
- FHR: absent/distressed
- Coagulation problems
- Beware DIC, pre-eclampsia
-
Placental praevia
- Dhock in proportion to visible loss
- No pain
- Uterus non tener
- Both may be abnormal
- FHR: usually normal
- Coagulation problems rare
- Small bleeds befor large


