Male Reproductive Physiology Flashcards
Gonadotropin secretion over the lifetime
when is FSH>LH

Review of male hypogonadism

Hypothalamic pituitary gonadal axis male
Hypothalamus secretes GnRH that stimulates the AP. Ap releases LH and FSH. LH receptors on Leydigs, so stimulates them, mediating production of test and other androgens,
testosterone can cross over to the sertoli cells and stimulate them because they have test receptors as well as being stimulated by FSH . products of this are production of abp, estrogen through synthesis of aromatase, mediating the process of spermatogenesis. the other product is inhibin TYPE B. feeds back onto ap negatively for FSH.
the aspect of regenerating estrogen or DHT, influence negatively at AP and the Hypo

Fetal actions of Test
- when does test present?
- causes what during the last 2-3 motnhs of pregnancy?
- whats it called if this fails

phases of Spermatogenesis:
Mitotic divisions (spermatocytogenesis) starts at puberty and mitotic cycles increase and spermatogonia or stem cells divide to produce daughter spermatogonia, resulting in Primary spermatocytes
Meiosis: primary spermatocytes undergo two divisions. first divsion produces to secondary spermatocytes each w/ a haploid DNA, second division produces two spermatids, each with a haploid # unduplicated
Spermiogenesis: spermatids mature into spermatozoa, ends w/ release of spermatozoa by sertolis

Specific actions of DHT:
- fetal differentiaion of ehat?
- hair?
- sebaceous gland?
- prostate?
- 5a reductase inhibitors

Which enzyme converts T to DHT in peripheral tissue
5a-reductase
Synthesis and secretion of T mechanism

Gonadal sex vs phenotypic sex

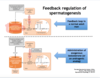
Feedback regulation of spermatogenesis in normal male vs male receiving exogenous Test
Focus on normal set point is being changed by adding more T to circulation. leads to low levels of LH and fsh but more so LH because LH is more sensitive to levels of androgens. repress hypothalmic and pituitary secretion low levels of LH. Leydig cells produce less Testosterone,which is important for spermatogenesis. impact in fertility of this individual.
DHT role in puberty
DHT binds to androgen receptors w/ greater affinity, deficiency of 5a reductase results in ambiguous external genitalia
Biosynthetic pathway of androgens in male:
- mitochondrial enzymes do what?
- what is the rate limiting step?

Where are the spermatogonia located?
- where are the spermatozoa located?
- percentage seminiferous tubules vs interstitium

Male Hypogonadism: Klinefelter
- dysgenesis of what?
- most common karyotype?
- what production is low, and levels of what are high?
= what degree of hypogonadism?

Capacitation of spermatozoa:
- what happens when they contact female fluid?
- what are the changes in the uterine tubes, cholesterol, Ca+2

Seminal vesicles:
produce what?
purpose?
purpose of prostaglandins? how does it work?

Different stages of male sexual function: plasma T and sperm production

Function of sertoli cells:
provide nutrients to differentiating sperm, form tight junctions with each other creating a barrier between testes and bloodstream, secrete an aqueous fluid into the lumen of the seminferous tubule to help transport sperm through the tubules into the epi
Secretions of vas def, seminal vesicles, and prostate gland
vas def secretes fluid rich in citrate and fructose, seminal vesicles secrete fluid rich in citrate, fructose, prostaglandins and fibrinogen.
-prostate secretes milky aqueous solution rich in citrate, calcium, and enzymes
Andropause:
- as men age what happens to sensitivity to LH? leading to?
- what happens to serum LH/FSH?
- what happens to test levels
- loss of sexual activity

Estrogen production in males
- which fluid is it highest in?
- what is the small and big source of estrogen
- potential role in spermatogenesis?

Emission:
- under what innervation?
- what prevents retrograde ejac of semen into bladder?
- is emission same as ejac?

Ejaculation:
-caused by which muscles contracting?

what initiates puberty?
-can this be replicated?

What are the androgens secreted by the testis?
- which is most abundant?
- what happens in target tissues?

Anatomy of male reproductive tract overview

Intracellular mechanism of action of testosterone
- Leydig cell
- Sertoli cell
Leydig cell has LH receptor and does the cAMP and PKA pathway
results in steroidgenesis/testosterone production
Sertoli Cell is stimulated by Test and FSH and does the cAMP and PKA pathway
results in protein synthesis and production of inhibin (inhibits FSH release), androgen binding protein, aromatase.
inhibin B feeds back onto ant pit specifically for FSH

Gonadal dysfunction in males: T deficiency effects based on age of onset
- 2nd-3rd month of gestation:
- 3rd trimester
- puberty
- post puberty

CNS/Nutritional Status and onset of puberty
-what types of things can delay onset of puberty in girls, in general?

Hormonal factors that stimulate spermatogenesis and how they do it
- LH
- FSH
- GH
- Test
- Estrogen

Prostate gland:
- secretes what?
- purpose?

Where is T concentrated and by what?
what is it carried into the peripheral circulation with?
in the seminiferous tubules, t is concentrated by binding ABP
T is carried in the peripheral circulation by SHBG and albumin
What enzymes do the testis lack?
- why is this important?
- which enzyme do they have and what does it do?
- how is T concentrated in the testis?

Male Hypogonadism: Kallman’s
- mechanism
- charecterized by?

Erection
- role of parasympathetics
- what does NO do?
- where does increased blood flow go?
- effect of somatic stimulation?

Fsh stimulates Sertoli to secrete what into the lumen of the sem tubules?
-purpose of this?

Fates of Testosterone:
- how much bound to SHBG, albumin, free?
- how is it excreted

Tissues producing androgens
- test to DHT enzyme
- test to estradiol enzyme

Leydig cells:
- de novo synthesis how?
- store cholesterol as?, how do they make it free again?
- what transfers cholesterol within the mito membranes?

What does LH do to the Leydig cell
-two ways?

Where does spermatogenesis occur?
-types of cells in spermatogenic epithelium, how long does it take, staggering?

Acrosome reaction:
- fusion of what membranes?
- in order to release what?

Supportive function of sertoli
exocrine function of sertoli
endocrine function of sertoli

Another overview of male anatomy

Sperm maturation:
where
how long?
what process occurs here?
important to prevent immature premature acrosome reaction by decapactiation in epi.

First five weeks of gestational life the gonands are?
- during weeks 6-7
- during week 9
first 5 weeks bipotential, 6-7 testes begin to develop in genetic males, week 9 the ovaries begin to develop
how is MPB treated?
how is BPH treated?
Prostate cancer treatment?
signs of testicular cancer?

Anabolic actions of androgens

Benign Prostatic Hyperplasia
- percent of men over 80
- classic signs
- concentrations of DHT in BPH vs non BPH, what does this mean?


just an overview
Semen fun facts:
ph, lifespan, contents in ejac

Erection/Detumescence
- process of erection
- what happens to pudendal nerve
- how does this produce erection?
- what terminates erection?

Test production
- when does it begin?
- what do androgens bind to?

Androgen insensitivity syndrome case:
- girl has normal breasts at age 11, and larger than average at 13. at 16 hasnt menstruated yet, she has testes and a short vagina, no cervix, ovaries, or uterus. she is XY.
- high plasma test and levels of LH
- explain
-lack of androgen receptors in target tissues. testes secrete amh and test in utero. in her case, the AMH made female internal paramesonephric duct degenerate, but her nonresponse to test didn’t remodel the medonephric duct, she became externally female by default

baby has no penis, enlarged clitoris, XX genotype, ovaries, no testes.
-adrenal hyperplasia w/ lack of 21B-hydroxylase.
explain
21B-hydroxylase nromally converts steroid precursors to mineralcorticods and cortisol, with this defect precursurs accumulate, and lean towards production of androgens. causes masculinization of external genitalia. internal organs are female because there was no source of amh.
hyperplasia of adrenal cortex because w/o cortisol negative feedback, ACTH increases and trophies ac
- enlarged clitoris, not developing breasts menstrual periods, voice depening, clitoris growing larger. 5a-reductase deficiency.
- no ovaries, uterus, blind vaginal pouch, small prostate, penis, 46XY. High Test levels, low dihydrotestosterone.
-testes secrete test, vut she lacks 5a reductase to convert it to dihydrotestosterone that would differentiate male genitalia, hair growth, etc.
prenatally amh supressed female internal genitals. test caused modification of mesonephros into male internal because that doesnt require DHT. but without DHT you get no external male genitalia.


