Histo/Phys of The Menstrual Cycle Flashcards
- Squamous-columnar junction, does it always stay the same?
- transformation zone? why important
- what does HPV infect specifically, what does adenocarcinoma affect
transformation zone is dynamic, as age, hormones change, pregnancy, zone moves. squamous columnar jxn is part of this zone.
- squamous epithelial cells become metaplastic, replace cells of the endocervix
- transformation zone cells are much more sensitive to HPV
- HPV is squamous only, adenocarcinoma is glandular tumors of the columnar endocervix

Thelarche
Adrenarche
Menarche
thelarche is breast development, adrenarche is increase in adrenal androgen secretion, menarche is beginning of menstrual
- structures
- layers
- type of epithelium, cells in mucosa
- types of muscle


- what phase?
- how can you tell by looking at epithelium?

loss of surface columnar epitheal cells, glands dying, necrotic fragments
Turner syndrome:
- most common cause of congenital what
- 50% of cases are what genotype
- germ cells don’t develop, characterized by what?
- due to ovarian failure, female turners may have elevated what levels?

- what causes the induction of the LH surge?
- as luteal phase begins, what begins to decrease, this reflects negative feedback by what?
- as gonadotropin levels fall so do what?

Contraceptive effectiveness of OCPs is due to what?
- what is their net effect?
- what level do they work at?
- progestin effect?
progestin only ocps cause cervical mucus to thicken and become sticky/insufficient.
impair the motility of the uterus/oviducts

Polycystic ovarian syndrome:
- most common cause of what
- when does it usually manifest
- various combinations of unexplained?
- clinical manifestation?

During follicular phase major product of follicle is?
- theca doesnt have what?
- granulosa doesn’t have what?
*theca cells are closer to blood supply, can take in cholesterol or denovo, they have 3bhsd (pregnenolone to progesterone) and they have CYP17 17ahydroxylase (progesterone to androstenedione) also have 17B-HSD which can convert androstenedione into testosterone: small amounts.
most of the androstendione goes over to granulosa cell over the basal lamina and is converted into estradiol due to presence of aromatase (CYP19)

Name structures
- epithelial lining of superficial functional layer of endometrium.
- glands in the superficial functional layer
- which layer source of regeneration
Layers of muscle in myometrium

**myometrium not responsive to hormones

Ovarian hormones drive morphological /functional changes of the endometrium:
- size of endometrium during menses vs secretory phase?
- basal body temp?
higher levels of estrogen during pre ovulatory follicular phase lower basal body temperature.
higher levels of progesterone by corpus luteum raise BBT

structures?
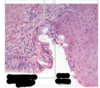
what phase is this?


- what phase, how long does it last?
- what initiates it?
- what happens to functional layer, spiral arteries
- what is now responsive to progesterone
- endometrial gland description


which phase, how can you tell.

secretory, more glands, more curvy (tortuous)
Cervix:
Endocervix: type of epithelium, what does it secrete, regulated by? cysts?
ectocervix: type of epithelium, continous with which epithelium?
- where does vagina get its lubrication?
gets lubrication from endocervix/greater and lesser vestibule glands

early in follicular phase vs late in follicular phase:
- sensitivity of gonadotrophs to GnRH early vs late
- what causes change in sensitivity

menstrual phase:
-what happens if fetilizaton did not occur?

Endometriosis:
- characterized by growth of what type of tissue outside the uterus?
- most commonly involves?
- clinical presentation

Follicular phase:
- begins and ends with? what day?
- granulosa cells increase production of what? purpose?

negative feedback by inhibins
-why is it important
inhibit FSH secretion and have an intraovarian effect of decreasing androgen production, which can have secondary effects on intrafollicular estrogen production
positive feedback HPO
- at end of what phase?
- estradiol levels through 1st half vs 2nd half
- threshold for how long before reversal in sensitivity?
- causes surge in what?
- what other rising hormone helps facilitate surge

Proliferative phase:
- after menstruation how long does it take to restore endo?
- proliferation of what layer of cells
- endometrium goes from .5 mm to how many during proliferative?
- what stimulates this phase?
- what does this stimulant do to the stromal components of the endometrium?
- induces the synthesis of what type of receptors in endometrial tissue?
estrogen causes the stromal components of the endometrium to becoe highly developed. estrogen also induces the synthesis of progestin receptors in endometrial tissue. Estrogen primes endometrium for action of progesterone.
progesterone opposes the action of estrogen on the epithelial cells of the endometrium: inhibits epithelial cell proliferation but promotes proliferation of the endometrial stroma. Stimulate 17B-HSD and sulfotransferase. converts estradiol to weaker compounds.

phases of endometrial cycle
menses, proliferative phase, secretory phase
gonadotropin levels throughout life of a female
in a fetus/infancy, during second trimester/before six months, associated w/ need for development of male or female charecteristics.
- during puberty quiescent system might have to do with low levels of estrogen at this time,
- during puberty we start to see pulsatile nature of gonadotropin release at night during REM, not well known.
- but in reproductive years you see day and night pulsatile secretion
- during menopause we have decrease in estrogen and progesterone, removes some of the negative feedback, so higher levels of FSH and LH

**memorize**



H-p-ovarian axis
-what secretes inhibins/activins? what do they do
-
hyp secretes GnRH which stimulates AP to secrete LH/FSH
- LH stimulates theca cells, which don’t have aromatase to make estradiol, so they send their androstendione to granulosa cells, but it does have 17 a hydroxylase with 17,20 lyase, so progesterone is made. limited test being made.
- Granulosa cells are stimulated by FSH, and later on LH. early in follicular phase granulosa cells convert androstendione to estrogen, during luteal phase they make progesterone



Secretory phase:
- corresponds to which phase of ovarian?
- early secretory phase characterized by?
- middle to late secretory phase characterized by?
- thickness and contents of endometrium, endometrial glands.
- progesterone role.

after onset of menstruation HP axis returns to what pattern?

Uterus
-Body has what three layers
endometrium (mucosa), which has superficial functional layer, and basal layer
myometrium
adventitia or serosa (perimetrium)
Blood Supply to Uterus:
- uterine artery, and uterine branch of ovarian do what?
- what is main artery running through myometrium, and what does it give off?
- which arteries supply the basal layer
- which supply the functional layer?
- what happens during menstruation?
arcuate artery in myometrium gives off radial branch, straight arteries supply basal. jxn of straight and spiral where they constrict, dilate, constrict, repeat. causes functional layer to die

Turnder syndrome additional info

Menorrhagia
dysmenorhea
oligomenorrhea
amenorrhea
last two commonly due to dysfunction of what?

PCOS:
- LH, FSH, T levels
- what happens to follicles?
- DHEA levels?

what phase, how can you tell

deeper blood vessels, glands are short straight and empty. see surface layer of columnar cells again
what is occuring mid to late luteal phase?
- describe levels of estradiol, progesterone, inhibin, gonadotropin, LH during mid luteal
- late luteal, what causes decrease in levels of prog. estradiol, inhibin

structures?
what phase is this?
how long does it last?
- caused by what?
- characterization of spiral arteries and endometrial glands.


type of feedback through most of menstrual cycle? how does it work
- estrogen/progestin affect
- net effect is to reduce?
estrogens and progesterones feed back negatively on hypo and pituitary, net effect is to reduce LH and FSH
Inhibins:
- produced by which cells
- what stimulates these cells
- right before ovulation, LH can also stimulate which cells?
- what does it inhibit? where?

During luteal phase, major products of corpus luteum are?
-structural change in vascularity
structural change, vascularization being close to both theca and granulosa. both cells can produce progesterone, but only thecal 17 hydroxyprogesterone as well as androstendione. androstendione is important because estradiol production. early on there is transient inhibition of aromatase so main product is progesterone, but as that inhibition is lifted estradiol becomes substantial. with vascularization, granulosa cells have more steroidgenic activity due to ability to take cholesterol from the blood. LH surge increases expression of StAR, CYP11A1 (side chain cleave) and 3B-HSD
-granulosa lack 17ahydroxylase, important for 17 hydroxyprogesterone

structures
- layers of mucosa
- type of epithelium
- what is special about LP
- muscularis layer contains
- advential layer
- superior part of vagina comes from, infeior distal part comes from?

superior vagina comes from paramesonephric ducts, distal comes from urogenital sinus endoderm

Luteal phase:
- follicle transforms into what?
- what does it produce, purpose?
- luteal phase begins and ends on what days

Before ovulation, LH and FSH act on developing follicle,
after?
corpus luteum
Ovarian cycle
has what two cycles, what do they correspond to in endometrial cycle
follicular phase coincides with proliferative phase of endometrial cycle
-luteal phase coincides w/ secretory phase of endometrial cycle
Where else can you get estrogens?
in a non pregnant woman, what is primary circulating estrogen?
- ovarian de novo synthesis of?
- do ovaries have aromatase?
- what enzyme does liver have that can convert estradiol/estrone into estriol?

Cellular events that result in synthesis/secretion of gonoadotropins:
- binding of GnRh to Gpcr activates what?
- activated PLC leads to formation of what, which ends up stimulating PKC?
- what does PKC do -Difference between LH/FSH, what determines specificity?
- what causes exocytosis/release of gonadotropins?
during follicular phase dominancy of estrogen as positive feedback, during luteal phase, progesterone
inhibin b is follicular phase, inhibin A during luteal. males only have inhibin B

-name the structures

Menopause:
- definition
- average age
- due to reduction in ? and low levels of?
- LH/FSH levels?
- perimenopause symptoms, treatments



