Male Reproductive Histology (Dennis) Flashcards
What are the main functions of the male reproductive system?
- production, nourishment, and temporary storage of sperm
- synthesis/secretion of male sex hormones (androgens)
Where does sperm and androgen production occur?
testes
What structures transport sperm?
- epididymis
- ductus deferens
- ejaculatory duct
- urethra
What structures help produce semen?
- seminal vesicles
- prostate gland
- bulbourethral gland
What are the structures a/w the testes?
- testes: paired organs located in the scrotum, posteriorly a/w the epididymis
- tunica albuginea (TA): dense CT capsule
- TA forms the mediastinum testis (posterior), network of fibrous CT that extends from top to near bottom of each testis
- septa create lobules in which seminiferous tubules are housed
- tunica vaginalis: derived from peritoneum, has an outer parietal layer lining the scrotum and an inner visceral layer covering the tunica albuginea

What structures are a/w the seminiferous tubules?
- septa create 250-300 lobules containing 1-4 convoluted seminiferous tubules lined w/ seminiferous epithelium composed of:
1. sustentacular (Sertoli) cells
2. spermatogenic cells - tubules surrounded by CT and 3-5 layers of flattened, peritubular myoid cells (create peristaltic contractions that help move spermatozoa)
- interstitial cells of Leydig found in between seminiferous tubules

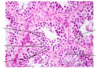
Identify the structures in the following images:

- IC: interstitial cells
- SC: Sertoli cells
- M: peritubular myoid cells
- F: fibroblasts
- SG: spermatogonia
- PS: primary spermatocytes
- ES: early spermatids
- LS: late spermatids

- steroid-producing cells (testosterone) containing lipid droplets, mito, and well-developed sER
- present in between tubules, close to blood vessels and lymphatic channels
- accompanied by myoid cells and fibroblasts
interstitial cells (of Leydig)

Identify the structures in the following images:

- BV: blood vessel
- L: lobule
- LC: leydig cells
- LP: lamina propria
- S: CT septa
- Sc: spermatocytes
- Sg: spermatogonia
- Sn: Sertoli nucleus
- Sp: spermatids
- TA: tunica albuginea
- X: tangential section of tubule w/ lumen obscured
- arrows: spermatid nuclei displaying early shape change

What are the structures/cells a/w seminiferous epithelium?
- SE: stratified epithelium w/ unusual characteristics
- sustentacular (Sertoli) cells: columnar cells w/ extensive processes that surround spermatogenic cells and occupy spaces between them; organize tubules and extend through the full thickness of epithelium; hallmark is cyclops nucleus
- spermatogenic cells: replicate and differentiate into mature sperm; spermatogonia (most immature) rest on basal lamina; spermatids (most mature) are attached to apical portion of Sertoli cell near tubule lumen

- “nurse” cells w/ crypts supporting 30-50 germ cells
- function in: exchange/transport of metabolites and nutritive factors into lumen; exocrine/endocrine secretion; phagocytose residual bodies (spermiogenesis) and effete spermatogenic cells
- bound by tight junctions to form Sertoli cell-to-Sertoli cell junctional complex: creates 50+ parallel lines of fusion along basolateral membranes, establishes blood-testis-barrier
Sertoli cells

What are the different types of spermatogenic cells?
- spermatogonia: clonoally divide (mitosis), located near basement membrane; type A spermatogonia (generates copies of itself and/or differentiates into type B); type B spermatogonia (enter meiotic prophase as primary spermatocytes)
- spermatocytes: two meiotic divisions and inside blood-testes barrier; primary spermatocytes > secondary spermatocytes > spermatids

How is a blood-testis barrier established?
- Sertoli-Sertoli junctional complex divides epithelium into basal and luminal compartments
- complexes establish blood-testis barrier: isolates haploid germ cells (secondary spermatocytes, spermatids, and sperm) from systemic circulation

How do pre-sperm cells move through the seminiferous compartments?
- spermatogonia and early primary spermatocytes are restricted to basal compartment
- primary spermatocytes pass through junctional complex, move from basal > luminal compartment
- mature spermatocytes and spermatids are restricted to luminal compartment

How do spermatids mature and where are they housed during their stages?
- spermatids undrego spermiogenesis and differentiate into mature sperm cells
- round (early) sperm: housed in niches of Sertoli cells
- elongated (late) spermatids: housed in apical crypts of Sertoli cells

- the release of mature spermatids into lumen
- spermatids lose intercellular bridges and mature spermatids are separated
- spermatozoa are fully formed, but not yet functional
- sperm are propelled into epididymal duct
spermiation
What is the general structure of sperm?
- comprised of head, neck, and tail
- head: contains flattened, elongated nucleus; partially capped by acrosome; contains hydrolytic enzymes
- tail: subdivided into middle piece containing mitochondria, principal piece which is the longest segment, and end piece

What is the pathway for sperm transport>
straight tubules
>
rete testis
>
efferent ductules
>
epididymis
>
ductus deferens
>
ejaculatory duct

Seminiferous tubules
- location:
- epithelium:
- support tissues:
- functions:
Seminiferous tubules
- location: testicular lobules
- epithelium: spermatogenic w/ Sertoli and germ cells
- support tissues: myoid cells and loose CT
- functions: produce sperm
Straight tubules
- location:
- epithelium:
- support tissues:
- functions:
Straight tubules
- location: periphery of the mediastinum testis
- epithelium: proximal = Sertoli cells only; distal = simple cuboidal
- support tissues: connective tissue
- functions: convey sperm into rete testis
Rete testis
- location:
- epithelium:
- support tissues:
- functions:
Rete testis
- location: in mediastinum testis
- epithelium: simple cuboidal w/ microvilla and single cilia
- support tissues: dense irregular CT, highly vascular
- functions: collects sperm from seminiferous tubules
Efferent ductules
- location:
- epithelium:
- support tissues:
- functions:
Efferent ductules
- location: from rete testis to head of epididymis
- epithelium: alternating patches of simple cuboidal nonciliated and simple columnar ciliated
- support tissues: thin circular layer of smooth muscle and vascular loose CT
- functions: convey sperm into the epididymis
Epididymal duct
- location:
- epithelium:
- support tissues:
- functions:
Epididymal duct
- location: head, body, tail of epididymis
- epithelium: pseudostratified columnar w/ stereocilia
- support tissues: circular smooth muscle initially, w/ inner and outer longitudinal layers in tail
- functions: sperm maturation and short-term storage, expels sperm at ejaculation
Ducutus deferens
- location:
- epithelium:
- support tissues:
- functions:
Ducutus deferens
- location: extends from epididymis to ejaculatory ducts in prostate gland
- epithelium: pseudostratified columnar w/ fewer stereocilia
- support tissues: fibroelastic lamina propria, inner longitudinal + middle circular + outer longitudinal layers of smooth muscle
- functions: carries sperm from epididymis > ejaculatory duct