Lower GI pathology Flashcards
How can lower GI pathology be categorised?
Congenital
Acquired:
- Mechanical
- Infection
- Inflammation
- Ischaemia
- Tumour
What are “general effects” of large bowel pathology?
Disturbance of normal function (diarrhoea, constipation)
Bleeding
Perforation/fistula formation
Obstruction
+/- Systemic illness
What are congenital diseases of the large bowel?
Atresia/stenosis
Duplication
Imperforate anus
What is Hirschsprung’s Disease?
- Absence of ganglion cells in myenteric plexus,
- Distal colon fails to dilate
- 80% male
- Constipation, abdominal distension, vomiting, ‘overflow’ diarrhoea
- Associated with Down’s syndrome (2%)
- RET proto-oncogene Cr10 + other
What are appropriate investigations for Hirschsprung’s Disease?
What is the treatment for Hirschsprung’s Disease?
Clinical impression
Biopsy of affected segment: Hypertrophied nerve fibers but no ganglia.
Treatment: Resection of affected (constricted) segment (frozen section).
What are mechanical diseases of the large bowel?
Obstruction
Adhesions
Herniation
Extrinsic mass
Volvulus
Diverticular disease
What is a volvulus?
Complete twisting of a loop of bowel at mesenteric base, around vascular pedicle.
Intestinal obstruction +/- infarction
Small bowel (infants)
Sigmoid colon (elderly)
What is the pathogenesis of diverticular disease?
High incidence in West
Low fibre diet
High intraluminal pressure
“Weak points” in wall of bowel
90% occur in left colon
What types of imaging can be used to diagnose diverticular disease?
Barium enema
Endoscopy
What are complications associated with diverticular disease?
Pain
Diverticulitis
Gross perforation
Fistula (bowel, bladder, vagina)
Obstruction
What are inflammatory diseases of the bowel?
Acute colitis:
- Infection (bacterial, viral, protozoal etc.)
- Drug/toxin (esp.antibiotic)
- Chemotherapy
- Radiation
Chronic colitis:
- Crohn’s
- Ulcerative colitis
- TB
What are the effects of infection?
Secretory diarrhoea (toxin)
Exudative diarrhoea (invasion and mucosal damage)
Severe tissue damage + perforation
Systemic illness
What is pseudomembranous colitis?
Antibiotic associated colitis
Acute colitis with pseudomembrane formation
Caused by protein exotoxins of C.difficile
How is pseudomembranous colitis diagnosed and treated?
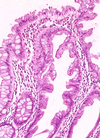
Histology: Yellow-white mucosal plaques or pseudomembranes; may resemble polyps or aphthoid ulcers of Crohn’s disease. Mucopurulent exudate erupts out of crypts to form a mushroom-like cloud with a linear configuration of karyorrhectic debris and neutrophils that adheres to surface.
Laboratory: C. difficile toxin stool assay.
Therapy: Metronidazole or Vancomycin.
What is ischaemic colitis/infarction?
Acute or chronic.
Most common vascular disorder of the intestinal tract.
Usually occurs in segments in “watershed” zones, e.g. splenic flexure (SMA and IMA) and the rectosigmoid (IMA and internal iliac artery).
Mucosal, mural, transmural (perforation).
What is the aetiology of ischaemic colitis?
Arterial Occlusion: Atheroma, thrombosis, embolism
Venous Occlusion: Thrombus, hypercoagulable states
Small Vessel Disease: DM, cholesterol emboli, vasculitis
Low Flow States: CCF, haemorrhage, shock
Obstruction: Hernia, intussusception, volvulus, adhesions
What are the two forms of inflammatory bowel disease?
Crohn’s disease
Ulcerative colitis
What are the causes of inflammatory bowel disease?
Aetiology unclear.
- Genetic predisposition (familial aggregation, twin studies, HLA)
- Infection (Mycobacteria, Measles etc)
- Abnormal host immunoreactivity
What are the signs and symptoms of inflammatory bowel disease?
- Diarrhoea +/- blood
- Fever
- Abdominal pain
- Acute abdomen
- Anaemia
- Weight loss
- Extra-intestinal manifestations
What is the epidemiology of Crohn’s Disease?
Western populations
Occurs at any age but peak onset in teens/twenties
White 2-5x > non-white
Higher incidence in Jewish population
Smoking
What are the clinical features of Crohn’s?
- Whole of GI tract can be affected (mouth to anus)
- ‘Skip lesions’
- Transmural inflammation
- Non-caseating granulomas
- Sinus/fistula formation
- ‘Fat wrapping’
- Thick ‘rubber-hose’ like wall
- Narrow lumen
- ‘Cobblestone mucosa’
- Linear ulcers
- Fissures
- Abscesses
What are extra-intestinal manifestations of Crohn’s Disease?
Arthritis
Uveitis
Stomatitis/cheilitis
Skin lesions:
- Pyoderma gangrenosum
- Erythema multiforme
- Erythema nodosum
What is the epidemiology of ulcerative colitis?
Slightly more common than Crohn’s
Whites > non-whites
Peak 20-25 years but can affect any age
What are clinical features of ulcerative colitis?
Involves rectum and colon in contiguous fashion.
May see mild ‘backwash ileitis’ and appendiceal involvement but small bowel and proximal GI tract not affected.
Inflammation confined to mucosa
Bowel wall normal thickness
Shallow ulcers