Lopez Review Flashcards
(42 cards)
Adenylyl cyclase mechanism
E.g. ACTH, LH, FSH, TSH, glucagon
Phospholipase C mechanism
E.g. GnRH, TRH, GHRH,
hormone-receptor complex works as a transcription factor that regulates the rate of transcription of a gene
E.g. thyroid hormones, glucocorticoids, aldosterone, estrogen, testosterone bind to receptor intracellularly and then bind to the SRE site on the DNA
The connections between the hypothalamus & anterior lobe are
The connections between the hypothalamus & anterior lobe are both neural & endocrine!
The connections between the hypothalamus and the posterior pituitary is
neural
1° endocrine disorder:
1° endocrine disorder: low or high levels of hormone due to defect in the peripheral endocrine gland
2° endocrine disorder:
.2° endocrine disorder: low or high levels of hormone due to defect in the pituitary gland
3° endocrine disorder:
3° endocrine disorder: low or high levels of hormone due to defect in the hypothalamus
what is the target of somatostatin?
somatotrophs in the AP, inhibits GH release
what is the target of GHRH?
somatrophs in the AP–> causes release of GH
what is the target of PIF?
lactotrophs. dopamine (PIF) decreases prolactin release
what is the target of TRH?
thyrotrophs in the AP normally; thyrotrophs AND lactotrophs when it is abnormally elevated
when is growth hormone highest and lowest?
adolescence it is highest; adulthood it is lowest
Somatomedins
insulin like growth factor (IGF-1): secreted by target tissues in response to growth hormone: negatively inhibits AP release of GR and positively stimulate hypothalamus to release the somatostatin to inhibit GH release from the AP
Growth hormone effects
- Diabetogenic effects
- increase in blood glucose concentration) • C
- insulin resistance by decreasing glucose uptake & utilization by target tissues
- increases lipolysis in adipose tissue
- Results in an increase of blood insulin
- increased protein synthesis & organ growth
- increased uptake of a.a •
- Stimulates synthesis of DNA, RNA, & protein
- Mediated by somatomedins (IGF-1)
- linear growth
- Stimulates synthesis of DNA, RNA, & protein
- Mediated by somatomedins (IGF-1)
- increases metabolism in cartilage-forming cells & chondrocytes proliferation
…..an important of determinant of GH, IGF-1, & insulin levels
nutritional status: fasting DECREASES somatomedin
- GH deficiency occurs with
- decreased secretion of GHRH due to hypothalamic dysfunction
- decreased growth hormone secretion 1° deficiency (lack of somatomedin feedback)
- GH or somatomedin resistance caused by deficiency of receptors
hyperprolactinemia: feedback system
prolactin negative feedbacks to the hypothalamus and suppresses GnRH (no LH or FSH), inhibits itself by stimulating dopamine release.
……neurons have cell bodies primarily in the supraoptic nuclei of the hypothalamus
ADH neurons have cell bodies primarily in the supraoptic nuclei of the hypothalamus
….. neurons have cell bodies primarily in the paraventricular nuclei of the hypothalamus
oxytocin neurons have cell bodies primarily in the paraventricular nuclei of the hypothalamus
Secretion of ADH is most sensitive to
Secretion of ADH is most sensitive to plasma osmolarity changes! An increase of only 1% in the osmolarity will increase ADH secretion
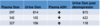
ADH triggers and receptors
what receptors do they act on in the body?
V1 receptors in blood vessels; V2 receptors in the kidneys
triggers: think the “big 3” one for each letter in ADH
- decreased blood pressure on barroreceptors in the cardiac and aortic receptors
- decreased stretch receptors stimulation in the atria
- increased osmolarity
- increased Plasma osmolarity (above 280 mOsm)
- DECREASED Blood pressure
- DECREASED Blood volume
- increased Angiotensin II
- Sympathetic stimulation
- Dehydration
three common trigger points for ADH
1) cardiac and aortic baroreceptors
2) aortic stretch receptors
3) mOsm receptors via interneurons