Fallopian tube/broad lig/ovary tumors Flashcards
hadatids of morgani: what is its histology?
hadatids of morganin- paratubal cysts, most common primary lesion of the fallopian tube. lined by serous (tubal) epithelium (ciliated columnar)
translucent cysts filled with serous fluid on the broad ligament
hadatids of morganin- paratubal cysts, most common primary lesion of the fallopian tube. lined by serous (tubal) epithelium (ciliated columnar)
mesothelioma tumor of the fallopian tube
adenomatoid tumor- occur subserosally on the tube or in the meosalpinx. BENIGN
usually 1/2 of the cells are stage 1 @ diagnosis
primary adenocarcinoma
presents as a dominant tubal mass that may be detected by pelvic examination. Others come to attention because of abnormal discharge, bleeding, or (occasionally) abnormal cells in a Pap smear. nearly 40% are dead within 5 years, with higher stage tumors pursuing an even more aggressive course.
primary adenocarcinoma
most common lesions encountered in the ovary are….and what kinds are there?
functional/benign cysts and tumors. three types: mullerian epithelium, germ cell, sex cord stromal cell
One of the rarest gynecologic cancers
primary adenocarcinoma of the fallopian tube
serous cancer that may arise from the fallopian tube initially: in what group are they more common?
this is a primary adenocarcinoma of the ovary: most common in
Postmenopausal Caucasians
very common in the ovary, and originate from unruptured graafian collicles
cystic follicle
usually multiple, filled with serous fluid and lined by a gray glistening membrane, can be diagnosed by both palpation and US, may cause pain
cystic follicle in the ovary
lined by rim of bright yellow tissue containing luteinized granulosa cells, can rupture and cause a reaction. what age group would these appear in?
Luteal cysts women of reproductive age , present in normal ovaries
central morphological abnormality: numerous cystic follicles or folliciular cysts that enlarge the ovaries
Polycystic ovarian syndrome (PCOS)
PCOS associations
DM 1, obesity, premature atherosclerosis
PCOS etiology
not fully understood but they think it involves enzymatic dysregulation
seen mostly in post-menopausal women, may overlap with PCOS in younger women
stromal hyperthecosis
characterized by uniform enlargement of the ovary, usually bilateral. what complications does it pose?
stromal hyperthecosis: virilization, acanthosis nigricans
diagnosed with type I DM. Patient is obese, XX, and returns to your office a year later presenting with masculine features and complaining of missing multiple menstrual cycles.
PCOS: hyper-androgenism, menstrual abnormalities, polycystic ovarie, chronic anovulation, decreased fertility
a 58 yo female presents with a mustache. US reveals bilateral ovarian enlargement
stromal hyperthecosis
perafolliicular zone expands, follicles regress and appear nodular
theca lutein hyperplasia of pregnancy
ovarian tumors by age: 20-45 vs 45-65
20-45 most likely benign, 45-65 mostly benign but malignancy will more likely occur in older groups
carcinoma associated with borderline tumors or endometrosis
type 1 low grade carcinoma
arises from serous intraepithelial carcinoma
type 2 high grade serous carcinoma
“tube like epithelium” in these tumors, and account for 40% of all ovarian cancers
serous tumors (cystic neoplasms)
Serous tumors: benign, borderline, and malignant together =
30% of ovarian tumors, 50% of ovarian epithelial tumors
most common serous tumors in 20-45 yos and 45+
benign/borderline = 20/45, 45+ = malig
BRCA1 and BRCA2
increased susceptibility to ovarian cancer, almost always high grade serous carcinomas with TP53 mutations
genetic mutations ass w/ low grade serous tumors
KRAS, BRAF, ERB2, wild type TP53
ovarian tumors account for ___ of all cancers and ____ most common cause of cancer caused mortality
3% of all cancers, 5th most common
if ovarian tumors are only 3% of all cancers, why are they the 5th leading cause of mortality caused by cancer?
Because most ovarian cancers have spread beyond the ovary by the time of diagnosis, they account for a disproportionate number of deaths from cancer of the female genital tract.
High grade tumors
high frequency TP53 muts, all BRCA1/2 mut ass w/TP53 mutations
serous ovarian tumors total% and bilaterality by %:
benign 60%; 25% bl
borderline 15%; 30% bl
malignant 25%; 65% bl
mucinous ovarian tumors by total % and bl %
benign 80%; %5 bl
borderline 10%; 10% bl
malignant 10%; < 5 % bl
Frequency of malignancy (> < = etc)
Serous borderline tumors> endometrioid tumor > undifferentiated > clear cell > [granulosa ~ = metastatic teratoma] > [mucinous borderline ~= other tumors unnamed] > benign teratoma (1%)
bilaterality by frequency
malignant serous tumor > metastatic teratoma > [clear cell ~= endometrioid] > borderline serous > benign serous> teratomas all together > borderline mucinous > benign mucinous > malignant mucinous > benign teratoma (rare for bilaterality to occur at all)
risk factors for malignant serous cystadenocarcinoma and reduced-risk factors
Risk factors:
- Nulliparity (low parity)
- Family/hereditary history. Heritable mutations: BRCA1 and BRCA2 (serous cystadenocarcinoma)
Reduced-risk Factors
- birth control pills
- tubal ligation
cystic lesion projecting from ovarian surface– no epithelial thickening, and no papillary projection
benign serous tumor: KRAS, ERB,2, BRAF, TP52 mutations
cystic lesion with papillary epithelium in a fibrous wall, contains an increased number of papillary projections

borderline serous cystadenoma

Serious cystcadenocarcinoma: the cyst has been dissected open to expose solid masses with nodular capsules, the masses are papillary
complex stromal papillae, stratification of the epithelium, nuclear atypia, but no invasion of the stroma see
epithelial proliferation often grows in a delicate, papillary pattern referred to as “micropapillary carcinoma,”
what is this tumor, and what is it thought to be the precursor of?
serous borderline tumor, thought to be a precursor to serous cystadenomcarcinoma
- CA-125
- HE4
- CA-125 (used to monitor recurrence/progression)
- HE4 (new, same purpose as above)
what percent of endometrioid carcinoma coexist with endometriosis? What is the peak incidence of tumors associated with endometriosis?
About 15% to 30% of cases with endometrioid carcinoma coexist with endometriosis.
peak incidence of endometrioid tumors associated with endometriosis occurs a decade earlier than that of endometrioid carcinomas that are not associated with endometriosis
10-15% of all ovarian cancers
endometrioid carcinoma
what kind of tumor is shown here
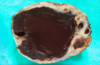
chocolate cyst found in endometriosis
15-20% arise with _________ and these occur a ______ than those that arise without endometriosis
15-30% are accompanied by ___________
endometrioid tumors
- 15-20% arise with ovarian endometriosis and these occur a decade earlier than those that arise without endometriosis
- 15-30% are accompanied by uterine endometrial carcinoma (synchronous primaries)
15-20% of all ovarian tumors
teratomas
what would we see increased in the individual from whom this biopsy was taken?
what are two names for it?
how common is it?

” glomeruloid” structures (Schiller-Duvall bodies): Yolk sac tumor AKA endodermal sinus tumor
Most common germ cell tumor in children
Increased serum AFP (hyaline droplets)
Increased serum AFP (hyaline droplets)
- Yolk sac tumor AKA endodermal sinus tumor
- Most common germ cell tumor in children
- Increased serum AFP (hyaline droplets)
- “glomeruloid” structures (Schiller-Duvall bodies)
dermatoid cyst
- mature teratoma (benign), almost always lined by skin-line epithelium
- may also have hair, teeth, sebaceous material
- young women of reproductive years
- found in association with inflammatory limbic encephalitis
occasionally absorbed into wall of a mucinous cystadenoma
mature teratoma (Dermatoid cyst)
teratoma with karyotype 46, xx. significance
- almost all benign ovarian teratomas
- arises from ovum after first meiotic division
tumor composed almost entirely of thyroid tissue
monodermal tumor- stromi ovarri- may be functional and cause hyperthyroidism
intestinal tissue found inside the tumor
carcinoid tumor- 5HT secreting, almost always unilateral but still has to be distinguished from a metastatic tumor
tumors found almost always in prepubertal adolescents and young women
immature malignant teratomas, mean age ~18, all germ layers present, frequently penetrates capsule and spreads locally or distantly
CHEMO IS GENERALLY CURATIVE FOR STAGE 1
express OCT4, OCT4, Nannog, and 33% have KIT tyrosine kinase mutations
dysgerminoma. a small number also produce chorionic gondaotropin
usually appear in 20s/30s. associated with pseudohermaphrodism. what endocrine function does this tumor have?
dysgeminomia: most have no endocrine function but a few produce chorionic gondotropin
alpha fetoprotein
yolk sac tumors, second most common malignant tumor of germ cell origin
characteristic histologic feature: a glomerulus like structure composed of a central blood vessel enveloped by tumor cells within a space also lined by tumor cells
Schiller duval body- found in yolk sac tumors

papillary serous cystadenocarcinoma.

psammoma bodies often found in serous carcinomas but are not pathognomonic
composed of cells that resemble cells of developing ovarian follicle
granulosa cell tumors: divided into adult and juvenile granulosa
cuboidal to polygonal cells that grow in anastomosing cords, sheets, or strands
granulosa cell tumors
small distinctive glandlike structures filled with acidophilic material recall immature follicles
“cell exner bodies” seen in granulosa cell tumors
granulosa cells tumors and their clinical significance
- may elaborate estrogen causing precocious puberty in young girls
- in grown women, may be associated with proliferative breast dz, endometrial hyperplasia, endometrial carcinoma
theca cell tumors: why are these preferable to others?
granulosa cell tumor that is almost never malignant.
biomarker of granulosa cell tumors
inhibin
foxL2 gene mutation
97% of granulosa cell tumors
plump spindle cells with lipid drops; fibroblasts
thecomas; fibromas
endodermal sinus tumor
aka yolk sac tumor
Meigs syndrome
fibromas, hydrothorax, ascites
~1/2 of these tumors have an mRNA splicing dysfunction
DICER1 gene in Sertoli-Leydig cell tumors
- Hirsutism, diabetes, multiple cysts
- Ascites, psammoma bodies, elevated CA-125
- Schiller-Duval bodies, AFP, hyaline droplets
- Fibroma, pleural effusion, ascites
- Hypertension, diabetes, obesity
- Call-Exner bodies, DUB, KIT mutation
- PCOS
- Papillary serous cystadenocarcinoma (high grade carcinoma)
- ………
chocolate cyst
endometrioid tumor: ectopic endometrioid tissue within ovary with cyst formation
sheets of uniform “fried egg” appearing cells, hCG and LDH are common tumor markers
dysgerminoma
28 year old woman with acute lower abdominal pain rushed to the OR for emergency surgery
ovarian torsion
- Infrequent but significant cause of acute lower abdominal pain
- Reproductive age median age 28, second peak postmenopausal
- Tube often involved
- If not considered delay can lead to vascular compromise of adnexa and subsequent infarction
- 5th most common cause of gynecologic surgical emergency
causes of hirsutism
- most often idiopathic
- PCOS
- non-classical CAH (less frequently)
the most common symptoms associated with tumor or cancer invasion
- Abdominal pain and distention
- urinary and gastrointestinal tract symptoms due to compression
- vaginal bleeding are the most common symptoms.
% of ovarian tumors that are benign and % that are bilateral
60%, 25%

granulosa cell tumor attempts to form structures that resemble primitive follicles, as seen at the left. Most of these tumors are histologically benign, but some are malignant.
Reinke crystalloids
hilus cell tumor- leydig ell neoplasms composed entirely of lipid-leydig cells.
bilateral metastasis composed of mucin producing signet ring cancer cells
most of gastric origin
a complex endocrine disorder effecting the fallopian tube. whare is this syndrome characterized by?
PCOS:
- hyperandrogenism
- menstrual abnormalities,
- polycystic ovaries,
- chronic anovulation,
- decreased fertility
overweight young woman presenting with infertility, oligomenorrhea and hirsutism
PCOS
most common ovarian mass overall
cystic follicle
commonly spread to the surface of the peritoneum and associated with ascites
serous carcinoma, both high and low
endometrioid adenofibromas
rare, benign
how are endometrioid carcinomas distinguished from serous and mucinous tumors?
presence of tubular glands resembling benign or malignant endometrium
Serous tumors: ages
mucinous tumors: ages
serous tumors: 20/45 (benign) serous tumors, 45+ malignant
mucinous tumors: midlife
most common presenting symptoms in ovarian tumors
- Abdominal pain and distention
- urinary and gastrointestinal tract symptoms due to compression by the tumor or cancer invasion
- vaginal bleeding are the most common symptoms.
mutation of KRAS proto-concogene is a consisent genetic alteration found in these tumors
mucinous
Type 1 carcinomas of the ovary include
low grade serous, mucinous, endometrioid
type 2 carcinomas of the ovaries include
high grade serous carcinoma
high grade serous carcinoma usually arises from what?
CIS from the fallopian tube or inclusions cysts within the ovary
type 1 ovarian carcinoma tumor progression
arise from benign tumors (cystadenomas)–-> borderline tumors--> low grade serous, endometrioid, mucinous carcinoma
type 2 ovarian carcinoma progression
CIS (unidentified) from fallopian tube fimbrae epithelia OR an ovarian inclusion cyst –> high grade carcinoma (Type II)
Benign and borderline subtypes are uncommon in this ovarian tumor
endometrioid
- stromal papillae with columnar epithelium
- architectural complexity and epithelial stratification
- complex micropapillary growth
- invasion of underlying stroma
- serous cystadenoma
- serous borderline tumor
- low grade serous carcinoma
- hgih grade serous carcinoma


