Cancer Flashcards
- Solitary or miltifocal
- Move freely during swallowing
- Typically presents asymptomatically
- cold masses on scintiscans
- isolated cervical nodal metz = no prognostic significance
- finely dispersed chromatin impart optically clear, empty appearance “orphan annie eye nuclei” and invaginations that give the appear of inclusions, called pseudo inclusions
- Fibrosis, calcification, cystic, psammoma bodies
- papillary carcinoma
variant of papillary carcinoma
- more aggressive
- high freq RAS mutations
- lower freq RET/PTC
- lower freq of BRAF mutations
Poorly Circumscribed-infiltrative-papillary follicular carcinoma
Papillary carcinoma variant
- Tend to occur in older folks
- all columnar cells
- Intensely eosinophilic cytoplasm lining papillary structure
Papillary carcinoma tall cell variant
Papillary carcinoma tall cell variant: characteristics
- Higher frequencies of vascular invasion
- Higher frequencies of extrathyroidal extension
- Higher frequencies of cervical and distant metz
- BRAF (bad) mutations 55%-100% of cases
- RET/PTC translon often as well
- BRAD and RET/PTC synergistic
- Younger children/individuals
- LN metz in almost all cases
- NO BRAF mutations, ~50% have RET/PTC translocations
- Papillary patter + solid areas of squamous metaplasia “nests”
- Extensive fibrosis through thyroid
Diffuse sclerosing-papillary variant
- Younger children/individuals
- LN metz in almost all cases
- NO BRAF mutations, ~50% have RET/PTC translocations
- Papillary patter + solid areas of squamous metaplasia “nests”
- Extensive fibrosis through thyroid
- Often associated with lymphocytic infiltrate that simulates Hoshimoto’s thyroidits
thyroid neoplasms:
gender, age, malig vs benign, progressive vs indolent,
Solitary palpable nodules US adults: incidence1‐ 10%
- Significantly higher in endemic goitrous regions
- W>M
- Incidence increases throughout life
- Overwhelming majority of solitary nodules are benign
- < 1% of solitary thyroid nodules are malignant
- ~ 15,000 new cases of thyroid carcinoma per year in the US
- Most of these cancers are indolent
features more likely to make a nodule neoplastic vs benign
More likely neoplastic:
– Solitary nodules
– Nodules in younger patients
– Nodules in males
– History of radiation to the head and neck
More likely benign:
– Multiple nodules
– Nodules in older patients
– Nodules in females
– Functional nodules that take up radioactive iodine (hot nodules)
present as discrete, solitary, unilateral and painless masses during routine physical examination
– Larger masses may produce symptoms (e.g difficulty swallowing)
folliciular adenoma
in general non-functional, small subset are hot
Solitary, spherical, encapsulated lesion that is well demarcated from the surrounding thyroid and made up of uniform‐appearing follicles which typically contain colloid
- growth pattern is usually quite distinct from the adjacent thyroid
- Cells are uniform and bland
- Look like surrounding follicular epithelial cells
- Occasionally the cells have eosinophilic, granular cytoplasm (oxyphil or Hürthle cell change)
How do we distinguish it from carcinoma?
The integrity of the capsule is key in distinguishing follicular adenomas from follicular carcinomas
Folliciular adenomas:
- Solitary, spherical, encapsulated lesion
- Well demarcated from the surrounding thyroid • Made up of uniform‐appearing follicles that
- typically contain colloid
- The follicular growth pattern is usually quite distinct from the adjacent thyroid
- Cells are uniform and bland

Fine Needle Aspiration
With or without ultrasound guidance
Very useful in evaluation of thyroid nodules

Diagnosis of Follicular Adenomas: Radionuclide, US, FNA, and surgical resection
-
Radionuclide scan
- Cold Nodules: Nonfunctioning adenomas take up less radioactive iodine than the normal thyroid parenchyma
- Up to 10% of cold nodules are malignant
- Cold Nodules: Nonfunctioning adenomas take up less radioactive iodine than the normal thyroid parenchyma
-
Ultrasonography and fine‐needle aspiration
- “Follicular neoplasm” with ddx of follicular adenoma, follicular carcinoma, or follicular variant of papillary carcinoma
- Ultimately need to evaluate capsule for a definitive diagnosis
-
Surgically resected:
- capsule is evaluated grossly and histologically to exclude carcinoma
thyroid cancer: gender, age, RFs, association with iodine, types
W>M early and middle adult years; W≈M in childhood and late adult life
Exposure to ionizing radiation early in life leads to increased risk of Papillary carcinoma
Dietary iodine deficiency is linked with a higher frequency of follicular carcinomas
Types:
– Papillary carcinoma (>85% of cases)
– Follicular carcinoma (5% to 15% of cases)
– Anaplastic (undifferentiated) carcinoma (<5% of cases)
– Medullary carcinoma (5% of cases)
RET/PTC translocation/inversion
papillary T carcinoma, Tall Cell variant PTC often has this mutation
RAS
Follicular carcinoma and anaplastic carcinoma
PAX8; PPARG
Follicular carcinoma
PI3K
Follicular and anaplastic carcinoma, point mutations and amplifications
PTEN
folliciular and anaplastic carcinomas
most common form of thyroid carcinoma
papillary carcinoma (86%), can occur at any age, 25-50 is the peak period
papillary carcinoma
- Can be solitary or multifocal
- Can be well circumscribed, encapsulated, or infiltrative
- Usually has areas of fibrosis and calcification
- Often cystic
- Nuclei are the key to diagnosis:
- Finely dispersed chromatin, giving them an optically clear or empty appearance
- Ground‐glass or Orphan Annie eye nuclei
- Nuclear groove
- Invaginations of the cytoplasm gives the appearance of intranuclear inclusions (“pseudo‐inclusions”)
pic
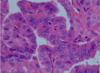
orphan annie nuclei- papillary carcinoma
BRAF
Papillary carcinoma, tall cell variant (55%-100%), poor prognosis
diagnosis. cervical nodal metastasis and PTC. Most common metz, clinical survival rate
- Radionuclide: cold nodule
- FNA can be diagnostic if nuclear features present
- ISOLATED LN metz does not have a significant influence of prognosis
- If metz to other locations beyond LNs, lung is the most common
- 10 yr survival > 95%, less than 40 not as good




