Lecture 12- The ECG Flashcards
(71 cards)
The conduction system
- SA node sends an AP which spreads across atria causing contraction
- AP reaches the AV node, which transmits the AP to the bundle of His through the annulus fibrosus (separates atria from ventricles)
- Bundle of His divides into:
- Right bundle branch- travels along right side of interventricular septum- excising right ventricle
- Left bundle branch- travels along left side of interventricular septum- excites left ventricle
- Right and left bundle branch terminate in extensive network of conducting fibres called purkinje fibresà continue wave of depolarisation through the ventricles
- The impulse conducts across the ventricular myocardium causing contraction

Annulus fibrosis
- Anchors myocardium and cardiac valves
- Electrical insulator between atria and ventricles
- Consists of 4 fibrous rings (coloured blue)

conducting system of the ehart and heart rate: Atria SAN
- Fastest rate of depolarisation in the heart
- Intrinsic firing rate 60-100 times/minute
- Sets heart rate and rhythm- sinus rhythm
conducting system of the ehart and heart rate: atria AVN
- Slow conduction
- Gives time for atria to contract before ventricles
- Intrinsic firing rate without stimulation (such as from the SA node)- 40-60 times/minute
conducting system of the ehart and heart rate: ventricles left and right bundle branch
- Ventricular electrical conducting system cells also have an intrinsic firing rate although not typically manifested
- Intrinsic firing rare 20-40 times/minute - SLLOW
ECG basics
- Records cardiac electrical activity as transmitted to chest wall and limbs
- The signals sent throughout the heart by the conduction system can be picked up on an ECG.
electrodes
the wires you place on the body
Lead
describes the view of the hearts and the recordings on the ECG
how many electrodes used in a 12-lead ECG
10 electrodes are placed on patients body to give 12 views of the heart
how many limb electrodes
4
how many chest electrodes
6 ‘precordial’ electrodes
4 limb electrodes are placed on
bony parts of the body e.g. wrists and ankles

(Ride your green bike- from right wrist and working clockwise when looking at the front of the patient)
red electrode
right arm
yellow electrode
left arm
green electrode
left leg
black elecrode
right leg
- not used for any leads/views
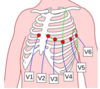
name the 6 chest electrodes (precordial)
V1- right sternal edge (4 th intercostal space (ICS)
V2- left sternal edge (4th ICS)
V3- half way between V2 and V4
V4- mid-clavicular line, 5th ICS
V5- hallway between V4 and V6
V6- mid-axillary line in line with V4
placement of chest electrodes
- V1- right sternal edge (4 th intercostal space (ICS)
- V2- left sternal edge (4th ICS)
- V3- half way between V2 and V4
- V4- mid-clavicular line, 5th ICS
- V5- hallway between V4 and V6
- V6- mid-axillary line in line with V4
It is usually best to place leads V1, V2, V4 and V6 first to help with placement of V3 and V5
each lead/view
–> Each lead/view of the ECG looks at a different part of the heart and is associated with a coronary artery
Multiple leads give us different views of the heart and allows us to see where pathology is- important in myocardial infarction in order to deduce which coronary artery is affected

lateral chest leads
V6, V5, V4

anterior leads
V4, V3, V2
septal leads
V1, V2
V1- V6 are knwon as
the anterior leads
- they ;ook at the front of the ehart












