Haematology: Haem malignancies, proliferative and dysplastic blood disorders (From Module 2 exam) Flashcards
Mainly SAQ revision
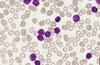
What disease does this blood film suggest?

- ALL
- Could also possibly be AML M0-1
What disease does the following immunophenotype suggest? Sig+, CD5+, Cyclin D1+, CD20+, CD10-, CD23-, BCL6-, MUM1-
- Mantle cell lymphoma
- (abnormal CD5 and Cyclin D1 expression)
What disease does this blood film suggest?

CLL
- Lymphocytosis
- Smear cells
What is the treatment for APML (Acute promyelocytic leukemia)?
-ATRA and arsenic
/////////////////////////////////////////////
-ATRA is All trans retinoic acid
What is the main genetic cause of Burkitt lymphoma?
-Lost regulation of c-myc
Outline clinical presentation of MDS (Myelodysplastic syndrome)
- Signs of bone marrow failure
- fatigue, infections, easy bruising
- Bone marrow hypercellular
- Cytopenia (a dysplastic change of a particular lineage causes the cytopenia of that lineage, i.e anaemia in erythroid dysplasia)
What disease does the following immunophenotype suggest? CD45+, CD13+, CD33+, CD117+, CD34+, HLA-DR+, CD19-, Tdt-
- AML M0/M1/M2
- CD34+, HLA-DR+, (Both markers of immaturity)
-What viruses can cause infectious mononucleosis?
EBV and CMV
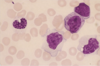
What disease does this blood film show?

CML, in chronic phase
Myelocytes and basophils can be present
Outline the pathophysiology of CML
- Translocation occurs between chromosome 9 and 22, forming BCR-ABL1 fusion gene
- BCR-ABL1 molecule is a constitutively active tyrosine kinase
- Causes downstream activation of oncogenes, such as JAK, PI3K and RAS
- Leading to increased proliferation, survival and clonal expansion of cells with the initial t(9;22) mutation.
Outline the clinical presentation of Adult T-cell laeukaemia/lymphoma (ATL)
- Human T-cell lymphotrophic virus 1 (HTLV-1)
- Hypercalcaemia (Stones, bones, groans etc.)
- Skin rash
- Other things pertaining to ALL or NHL
How does Multiple myeloma lead to bone weakness?
- Multilpe myeloma (MM) cells overproduce RANK ligand
- Leads to activation of osteoclasts
- Imbalance of osteoblast/osteoclast activity leads to osteolytic lesions and bone weakness
Extra info://///////////////////////////////////////////////////////
- Osteoprotegerin (OPG, regulator of normal bone formation) is downregulated (MM endocytosis)
- MM cels produce Dkk-1 which inhibit osteoblasts
- produces sclerostin, which inhibits osteoblasts
Case: A 51 year old woman was admitted to hospital showing: Asthenia(weakness), anorexia, weight loss. No significant findings on physical examination. Haemoglobin 83, WBC 6.5, platelets: 245. ESR 138 (high). IgA 14.1(high). Creatine 290 (high). See serum protein electrophoresis. CD38+, CD56+. What is the most likely diagnosis?

Multiple myeloma
Outline the causes of Marginal zone lymphoma
- Hep C
- H pylori
- Autoimmune causes
What disease does the following immunophenotype suggest? CD30+, CD15+, CD79a-, SmIg-, CD45-, CD34-, Tdt-
Hodgkin lymphoma
(CD30+, CD15+)
///////////////////
You see CD30+ and CD15+, you know its hodgkins lymphome
What disease oes this immunophenotype suggest?CD45-, no SCC, CD19-, CD33+, CD7-, CD13+
-AML M0-M1
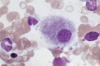
What disease does this blood film suggest?

Multiple myeloma
-Characteristic, pushed off to one side, extended cytoplasm
What are the viruses that can contribute to lymphoma?
EBV (Burkitt, Hodgkin)
HIV (Hodgkin, High grade B-cell lymphoma)
HTLV-1 (ATLL)
Hep C (Marginal zone lymphoma)
Human Herpes Virus (HHV8)
Hep B
What are the most common cytogenetic abnormalities associated with ALL?
- High hyperdiploidy (good prognosis)
- t(12;21)/ETV6-RUNX1 (Childhood, Good prognosis)
- t(9;22)/BCR-ABL1/Ph (older adults, bad prognosis)
- T-ALL: t(10;14)
/////////////////////////////////////////////////
- 11q23 rearrangements/KMT2A (infants, bad prognosis)
- t(1;19)/TCF-PBX1
What is the mechanism of action of Imatinib?
- Imatinib is a tyrosine kinase inhibitor
- It binds to the ATP binding site of BCR-ABL1, preventing ATP from binding and donating it’s phosphate.
- Therefore no activation of oncogenic proteins
What disease does this blood film suggest?

Mantle cell lymphoma
-Characteristic morphology?
Outline the main subtypes of myelodysplastic syndrome
- So it’s classified into these 5 subtypes though a condition can belong to more than one I suppose
- Single lineage dysplasia
- Erythroid dysplasia
- Granulocytic dysplasia
- Megakaryocytic dysplasia
- Multiple lineage dysplasia
- Adult
- Childhood
- Ring Sideroblasts (Single lineage erythroid dysplasia)
- 5q deletion
- Excess blasts
- Excess blasts type 1 (5-9% blasts)
- Excess blasts type 2 (10-19% blasts)
What genes are involved in multiple myeloma?
- IGH gene can be fused with:
- Cyclin D1
- MMSET gene
- Maf
- All leading to overproduction of Ig
Describe the myeloid maturation sequence
Myeloblast,
Promyelocyte,
Myelocyte,
Metamyelocyte,
Band,
granulocyte (e.g Neutrophil)
What blood parameters are associated with CML?
- High white cell count
- Anaemia (Sometimes)
- platelets can be either high or low (Mostly high)
- Basophiliia
What disease does this immunophenotype suggest? CD8-, CD4+, CD7-, CD3+, CD25+, CD5+, CD19-, CD34-, Tdt-
- Adult T-cell leukaemia/lymphoma (ATLL)
- CD25+
//////////////////////////////////////////////////
CD25+: ATLL
Describe the typical blood film of multiple myeloma
- Plasma cells (lymphocytes with extended cytoplasm, usually shifted in one direction.
- Granulation with pale are of ‘golgi zone’
- Roleaux formation
Case: See blood film. Immunophenotype: CD19+, CD5+, CD79b+/-, CD20+, CD2+/-, CD22+. What is the most likely diagnosis?

- CLL
- Smear cells, lymphocytosis
- CD5+, CD79b+,
What are the nucleated cells here?

Nucleated red cells/erythroblasts
What is the main clinical presentation of CML?
- Weight loss,
- Low grade fever
- Abdominal enlargement
What is the characteristic feature of multiple myeloma in a bone marrow aspirate?
>10% plasma cells
outline the pathophysiology of AML M2
- RUNX1-RUNX1T fusion causes the ineffectiveness of CBFalpha
- This leads to decreased differentation and maturation
What disease does the following immunophenotype suggest? CD45+, CD34+, Tdt+, CD20-, CD22-, CD10-, CD19-, CD7+, CD3+, CD2+, CD13-, CD33-, cytoplasmic m-.
T-ALL (T acute lymphoblastic leukaemia)
(CD7 is a t cell thing)
What disease does the following immunophenotype suggest? CD19+, CD20+, CD22+, CD79a+, CD79b+, BCL6+, CD10+(/-), Tdt-, Sig+, CD5-, CD23-, MUM1-, Monoclonal mature IgM (based on kappa:Lambda)
- Burkitt lymphoma.
- Monoclonal mature IgM (kappa 75% of cases/lambda 25% of cases)
- BCL6+ (maintains cells at germinal centre stage of development)
What disease does this lymph node histology suggest?

- ATLL
- Large T lymphocytes
- Reactive cell population (most likely eosinophils)
What are the most common cytogenetic abnormalities associated with MDS
- Del(11q) or –Y (Very good prognosis)
- Normal karyotype or del(5q) (Good prognosis)
- Del(7q) or double independent clones (intermediate)
- Inv(3) or double including -7 or 1del(7q) (Poor prognosis)
- Complex: >3 abnormalities (Very poor prognosis)
/////////////////////////////////////////////////
This is really fringe knowledge you probably dont need to know for path. Just understand that particular cytogenetic abnormalities are associated with/ cause MDS
Case: 66 year old woman, 2 week history of fatigue and pallor. Full blood count showing pancytopenia: Hb 98, WBC 4, platelets 16. No family history. No hepatomegaly or lymphadenopathy. Abdominal CT, mild splenomegaly. Blood film, immature granulocytes, occasional circulating blasts, with granules. Flow cytometry: High FSC, low SCC, cCD79, MPO-, HLA-DR+, CD34+, CD19+, CD20(mostly -), CD10+, CD38-, CD19+, CD45+/-, Tdt+, CD33-, CD13 (mostly-). What is the most likely diagnosis?
- CLL, B-lineage.
- granules rule out MDS
Case: See blood film: Immunophenotype: high FCC, moderate SCC. CD19+, CD5-, CD79b+, CD20+, CD2+/-, CD22+, CD23-, CD10+, monoclonal Ig (Lambda:kappa). t(14;18). What is the most likely diagnosis?
Follicular lymphoma
(Coffee bean/ butt cells)
Herpes zoster can increase incidence of:
-CLL or Hodgkin lymphoma
////////////////////////////////////////////
Don’t ask me how, something to do with constantly stimulating the immune cells to proliferate
The white cell shown is:

A normal large granular lymphocyte.
What is the normal range of haemoglobin?
- Male: 130-180 g/L
- Female: 115-165 g/L
/////////////////////////////////
Major Key Alert
What disease does the following lymph node histology suggest?

- Hodgkin lymphoma
- Sclerosis
- Reed-sternberg cells
What disease does the following immunophenotype suggest? CD45+, CD34+, Tdt+, CD20+, CD22+, CD10(+/-), CD19+, CD7-, CD3-, CD13-, CD33-, cytoplasmic m+.
B-ALL, specifically PreB-ALL
//////////////////////////////////////////////
One of these markers make it a ‘PreB-ALL’ rather than a regular B-ALL but this is beyond path.
What disease does this blood film suggest?

- ATLL
- Pleomorphism. Flower cell morphology
How does multiple myeloma cause kidney failure?
Excess Ig (normally IgG) leads to precipitation of light chains in the renal tubules of the kidney
What haematologial malignancy is Coxiella Burnetti linked to?
Diffuse large B-cell lymphoma (Non-Hodgkin)
//////////////////////////////////
no idea how or why really other than the whole ‘infection causes chronic stimulation and proliferation of immune cells leading to malignancy of those cells’ principle.
What disease does this blood film suggest

- Large cell lymphoma
- large and pleomorphic cell
What disease does this immunophenotype suggest? Large FCC, large SCC, CD117-, CD3-, CD34-, HLA-DR-, CD13+, CD33+, CD45+, CD14-
CML
//////////////////////////
Myeloid cells are CD13+, CD33+
What disease does this blood film suggest?

- Burkitt lymphoma
- mature blasts, with no granules (lymphoid cells)
- Characteristic prominent vacuolation
///////////////////////////////////
This vacuolation is pathognomonic of Burkitt’s Lymphoma
Outline presentation of MALT lymphoma
- Extranodal sites (Bascially a GI cancer)
- Caused by infection (H. Pylori) or autoimmune causes (Coeliacs)
- Immunophenotype: SIg+, CD20+, CD5-, CD10-, CD23+/-, BCL6-, MUM1+/-
- Cytogenetics: t(11;18). Activation of NFkB pathway.
Hypogranular neutrophil, blast cell, stomatocytes. Most likely diagnosis?
MDS
/////////////////////////////////
If no evidence of proliferation
This white cell shows what?

Toxic granulation and vacuolisation.
What disease does the following immunophenotype suggest? CD7-, CD13-, CD19-, CD33+, HLA-DR-, CD117+, CD15-, CD34+
- AML M3 (APML)
- Could also be AML M0, M1, M2
What is the typical presentation of multiple myeloma?
- Back pain
- Fatigue, pallor (anaemia)
- Infections (eg pneumonia)
- Signs of acute renal failure (polydipsia)
What disease does the following immunophenotype suggest? CD11c+, CD103+
Hairy cell leukaemia (A type of CLL)
//////////////////////////////////////
Very fringe, probably not needed for path
The white cell shown is:

An eosinophil
What are the clinical signs and symptoms of CLL?
- Lymphadenopathy
- features of anaemia (fatigue, pallor) (From Bone marrow failure)
- Bruising/purpura from thrombocytopenia (Also from Bone marrow failure)
- rarely hepatosplenomegaly
- Features of immune suppression (Infection)
What is the normal range of red cell count?
- Male: 4.5-6.5 1012/L
- Female: 3.8-4.8 1012/L
What haematological malignancy can coeliacs lead to?
-(non-hodgkin), of M.A.L.T lymphoma,
What are the most common cytogenetic abnormalities associated with CLL?
- Del(6q)
- Trisomy 12
- Del(13q)/miR-15a
-Del(13q)/retinoblastoma gene
- Del(17p)/TP53 loss
- Del(11q)/ATM
//////////////////////////////////////////////////////
This may be a bit too nische for path.
Maybe just remember the retinoblastoma one cause it sounds important.
What disease does this blood film show?

CML
(Left shift, a shift to immature cells)
Myelocyte > promyelocyte > metamyelocyte > Band forms
What kind of white cell is this?

Atypical lymphocyte
- Minimal chromatin condensation, lots of cytoplasm
- Large cell with no granulation
Describe the typical laboratory findings of Hodgkin lymphoma
- Normochromic, normocytic anaemia (without later bone marrow involvement)
- neutrophilia (1/3 of patients)
- ESR raised, CRP raised.
- Raised serum LDH
- Also characteristic histology
What disease is associated with a bone marrow trephine biopsy showing a marked increase in marrow lymphocytes, a nodular pattern of lymphoid accumulation and interstitial infiltration?
CLL
What disease does this blood film suggest?

- MDS
- White cells showing psudeo-pelger cells, agranular myelocytes an neutrophils
//////////////////////////////////////////
In MDS:
- Red cells are usually macrocytic but can be hypochromic.
- Granulocytes reduced in number and show lack of granulation
- Pelger abnormality (single or bilobed nucleus)
- Platelets unusual (usually reduced)
Case: A 38 year old woman of Caribbean origin. Rash of several years duration. Family history of ‘leukaemia’. Shortly before she had developed marked cervical lymphadenopathy and hypercalcaemia. Her skin showed plaque-like infiltrates. Flow cytometry: High SCC, CD2+, CD5+, CD7-, CD4+, CD8+, CD25+, CD71. She had also recently broken her clavicle
ATLL
/////////////////////////////////////////////////
I think of this as ‘Contagious leukaemia’
What is the most prominent cytogenetic abnormality associated with Burkitt lymphoma?
- t(8;14) C-MYC and IgH locus (90%)
- Other translocations of chromosome 8
What disease does this blood film suggest?
- MDS
- Mononuclear megakaryocyte
///////////////////////////////////////////////
- Red cells are usually macrocytic but can be hypochromic.
- Granulocytes reduced in number and show lack of granulation
- Pelger abnormality (single or bilobed nucleus)
- Platelets unusual (usually reduced)
What disease does this blood film suggest?

- One of the myelodysplastic syndromes
- Hypogranular neutrophil
- blast cell
- stomatocytes
Outline the clinical presentation of Burkitt lymphoma
- Painless lymphadenopathy, normally on jaw or abdomen
- History of Epstein Barr virus
- Can affect abdominal organs (Sporadic Burkitt lymphoma)
- Signs of pancytopenia in advanced disease
What disease does this blood film suggest?

- Follicular lymphoma
- Cleft/coffee bean/butt cells pathognomonic
What are the main cytogenetic abnormalities associated with multiple myeloma?
- Del(13q)
- mutations of telomere end of chromosome 14q32 (location of heavy chains, IgH)
- eg. t(4;14) IGH-MMSET1
Describe the typical blood count of a patient with CLL
- Lymphocytosis
- Anaemia
- Thrombocytopenia
/////////////////
Lots of white cells but bone marrow failure
What disease is the following karyotype associated with? 46, XX, inv(16)(p13q22)
AML M4
What are the main sub-types of CLL?
- CLL, regular
- Prolymphocytic leukaemia (PLL)
- Hairy cell leukaemia (HCL)
- Plasma cell leukaemia
- T cell:
- Large granular lymphocytic leukaemia
- T-PLL
- ATLL (Can be classed as a type of CLL or lymphoma)
What is the normal range of white cell count?
3.6-11.0 109/L
////////////////////////////////
Major Key Alert
What is the clinical presentation of CML (symptoms and signs)?
- Fatigue
- Night sweats
- Malaise and weight loss
- Left upper quadrant pain
- Splenomegaly
- Less common (in advanced diseas)
- Bone pain
- Lymphadenopathy
- Skin infiltration
- Extra medullary mass
What is the major complication of CLL?
- Autoimmune haemolytic anaemia: shown by spherocytes and polychromasia
- Direct antiglobulin test would be positive in this case
////////////////////////////////////
Good niche bit of knowledge that I reckon could get you a good extra mark somewhere in the exam
What bacteria can contribute to the development of lymphoma?
Helicobacter pylori (MALT lymphoma)
Campylobacter jejuni
Mycobacterium tuberculosis
Borrelia burdorferi
Chlamydophila psittaci
Outline the treatment for ATLL
Interferon and zidovudine. It’s as good as chemotherapy
////////////////////////
I think this is because of viral cause
What is the normal range of platelet count?
140-400 109/L
///////////////////////////////////////////////////
Major Key Alert
Outline the clinical presentation of Hodkin lymphoma
- Painless lymphadenopathy, more often localised to a single nodal site
- Splenomegaly
- History of Epstein Barr virus or HIV-1
- Consitutional symptoms in widespread disease: weight loss, night sweats, weight loss, etc.
What disease does the following lymph node histology suggest?

-Hodgkin lymphoma
///////////////////////////////////
- Sclerosis
- Reed-sternberg cells
Which is the most common haematological malignancy in children?
ALL
///////////////////////////////////////
It is what it is
What are the genes most commonly involved in CLL?
- P53 (bad prognosis)
- Retinoblastoma gene (bad prognosis)
- MiR15a
- ATM gene
- Loss of P53/del(17p) (bad prognosis)
////////////////////////////////////////////////
Arbitrarily picked the top two to remember since this is a bit to detailed
A child with mediastinal mass, weight loss, anaemia. Most likely diagnosis?
-T-ALL
(thymus enlargement)
What disease does this blood film suggest?
-MDS
////////////////////////////////////////
- Monocytoid cells and an agranular neutrophil
- Red cells are usually macrocytic but can be hypochromic.
- Granulocytes reduced in number and show lack of granulation
- Pelger abnormality (single or bilobed nucleus)
- Platelets unusual (usually reduced)
What is the main cytogenetic abnormality associated with follicular lymphoma?
t(14;18) involving BCL-2 gene (Causing abberrant expression)
//////////////////////////////////////////////////////////
Quite fringe for path
What disease does this lymph node histology suggest?

-Mantle cell lymphoma
///////////////////////////////////////////////////////////
- Characteristic deformed pattern of small lymphocytes with angular nuclei
- Expression of cyclin D1 can also show up
- Located in mantle zone
//Niche but could be useful
What disease does the following immunophenotype suggest? CD45+, CD34-, CD2-, CD13+, CD33+, CD117+, CD235a/Glycophorin+, CD19-
- AML M6 acute erythroid leukaemia
- CD235a/Glycophorin (erythroid marker)
In what disease may CAR-T cell therapy be effective?
-B-ALL (Specific for CD19)
///////////////////////////////////////////////////
But I think this therapy could be adapted to target any malignancy that has a distinguishing CD cell marker
Describe the typical blood count of a non-Hodgkin lymphoma
-In advanced disease there may be anaemia, neutropenia or thrombocytopenia
Describe the pathophysiology of APML
- PML-RARA fusion protein binds NCoR-HD complex
- This leads to inhibition of transcription and in turn a block in cell differentiation
- Retinoic acid (Vitamin A) is unable to exert it’s effect of continuing transcription
Describe how t(12;21) leads to ALL
- RUNX1 encodes CBFalpha, which binds to HAT (Activating transcription)
- In ETV6-RUNX1 fusion, the protein cannot bind to HAT.
- Therefore transcription is not activated (Causing a loss of differentiation?)
What disease does this immunophenotype suggest? CD45-, no SCC, CD10 (mostly+), CD19+, CD34(mostly+), CD5-, HLA-DR(+/-)
B-ALL
/////////////////////////////////////////////////
CD19+ means B cell
What disease does this blood film suggest?

AML
-M2. 1 Aur rod present
//////////////////////////
Aur rods means AML
1 Aur rods means AML M2
many aur rods means AML M3
Outline the symptoms of acute lymphoblastic/Myeloid leukaemia.
- Fever, sweats, weight loss (Systemic malignant symptoms)
- Caused by Bone marrow failure:
- tiredness, bruising and bleeding, infections/sepsis
- Caused by tissue infiltration
- Pulmonary infiltrates -> Shortness of breath, hepatomegaly, splenomegaly, gum hypertrophy
What disease does the following immunophenotype suggest? CD13+, CD33+, CD117+, CD7-, CD2- CD34-, CD41+, CD42+, CD61+.
-AML M7. Acute myeloid megakaryoblastic leukaemia
//////////////////////////////////////////////////////////
-CD41+, CD42+, CD61+ are platelet antigens.
Describe the typical node biopsy of Hodgkin lymphoma
- Sclerosis
- Reed-Sternberg cells/Owl cells
What disease does this lymph node histology (with BCL-6 staining) suggest?

- Follicular lymphoma
- Germinal centre cell origin
- BCL-6 stain +ve
- Also BCL-2 stain +ve in follicles
- Also diffusely CD10 +ve
What disease does the following immunophenotype suggest? CD19-, CD20- CD34-, Tdt- CD38+, CD138+, SIg-, CD7-, CD3-
-Multiple myeloma
////////////////////////////////////////////////////
- CD38, CD138 classic plasma cell markers
- MM cells don’t have SIg
What is the difference between MGUS, smouldering myeloma and multiple myeloma?
- MGUS:
- Monoclonal serum protein: <30g/L
- BM plasma cells: <10% of BM cells
- Multiple Myeloma
-Monoclonal serum protein: >/=30g/L
- BM plasma cells: >10% of BM cells
- Smouldering myeloma:
- Is just asymptomatic multiple myeloma
What disease does this blood film suggest?

- CLL
- Lymphocytosis, smear cells, thrombocytopenia
What disease does the following immunophenotype suggest? CD45+, CD34+, Tdt+, CD20+, CD22+, CD10+, CD19+, CD7-, CD3-, CD13-, CD33-, cytoplasmic m-
B-ALL
////////////////////////////////////////////////
Not sure why other than CD19+ and CD20+ means B cells
What are the lab findings associated with multiple myeloma?
- Calcium raised
- Renal impairment (raised creatinine)
- Anaemia (reduced Hb)
- Bone lesions (osteolytic) on x-ray
Also: /////////////////////////////
- monoclonal protein >/=30mg/L
- Abnormal immunoglobulins on electrophoresis (Monoclonal gammopathy). Excessive amounts of gammaglobulin
- increased serum immunoglobulin-free light chains
- Increased ESR
What disease does this blood film suggest?

ALL
-Could also possibly be AML M0-1
What disease does the following immunophenotype suggest? CD13+, CD33+, CD117+, CD15+, CD11c+, CD14+, CD64+, CD34-, CD19-, CD22-, Tdt-
-AML M5 acute myeloid monocytic leukaemia
///////////////////////////////////////
- CD13, CD33+ are myeloid markers
- CD15, CD11c, CD14, CD64 are monocyte markers
What is the main cytogenetic abnormality associated with Mantle Cell lymphoma?
-t(11;14), Cyclin D1 overexpression (also TP53 mutation)
////////////////////////////////////////
Probably too detailed for path
What is the typical immunophenotype of AML?
CD13+, CD33+, CD117+, -CD 34+ (if immature cells)
What disease does the following immunophenotype suggest? CD45+, CD34+, Tdt+, CD20+, CD22+, CD10-, CD19+, CD7-, CD3-, CD13-, CD33-, cytoplasmic m-
B-ALL, specifically ProB-ALL
////////////////////////////////////////////
What disease does this lymph node histology (with cyclin D1 stain) suggest?

- Mantle cell lymphoma
- expression of cyclin D1
- Located in mantle zone
- Characteristic deformed pattern of small lymphocytes with angular nuclei
Outline the treatment of Multiple myeloma
-Steroids
-Alkylating agents (melphalan)
///-Adds alkyl group to guanine residues, blocks replication, causes lymphopenia.////
-Proteosome inhibitors
///-proteosome required for protein degredation into oligopeptides/amino acids.
- Blocking proteasome leads to decreased amino acids in cell, leading to decreased protein synthesis
- Effective in MM as there is lots of protein production////
-Monoclonal Abs (daratumumab: anti CD38 antibody)
-Immunomodulatory drugs (IMIDS)
What disease does the following immunophenotype suggest? CD34-, Tdt-, CD19+, CD20+,CD23+, CD5+, CD13-, CD33-, CD7-, CD10-, CD79b-, light chain restriction (large disparity between Lambda:kappa)
CLL
/////////////////////////////////
-Not to be confused with mantle cell lymphoma (CD23-, Cyclin D1+)
What complications can arise from TKI therapy?
- Renal impairment
- Nausea and vomiting
- Pancytopenia
- Pleural effusion (From dasatinib)
What is the main translocation associated with CML?
t(9;22)/BCR-ABL1/Philadelphia chromosome
What diseases are caused by Epstein-Barr Virus?
- Burkitt’s lymphoma
- Hodgkin lymphoma
Presentation of tonsillar enlargement and cervical lymphadenopathy. Atypical lymphocytes and atypical mononuclear cells on blood film. Most likely diagnosis?
infectious mononucleosis.
What disease does this blood film suggest?

Multiple myeloma
- Plasma cell. Paler area is golgi zone.
- Roleux formation
Describe the typical blood count of a patient with ALL
- Anaemia
- Thrombocytopenia
- Neutropenia
What disease does this immunophenotype suggest? SIg+, CD20+, CD5-, CD10+, CD23+/-, BCL6+, MUM1-
- Follicular lymphoma (NHL)
- CD10+ main give away
What disease does this lymph node histology suggest?

- Burkitt lymphoma
- Germinal centre cell
- ‘starry sky appearance’
What disease does this immunophenotype suggest? CD45+, some SCC, Tdt-, MPO+, CD13+, CD33+, CD117+, CD34-, HLA-DR-, CD2(+/-)
- APML
- Suggested by abberant T-cell marker expression
/////////////////////////
CD2 is a T cekll marker, so that with Myeloid markers (CD13 and CD33) suggest APML.


