Foehring - Sensory Spinal Pathways Flashcards
What are the two systems for somesthesis? Fiber types and ascending tracts?
- PROTOPATHIC: anterolateral -> pain, crude touch, and temperature
1. Low spatial/temporal resolution
2. Sm, slowly conducting, lightly myelinated (A-delta) and unmyelinated (C) fibers
3. Lateral spinothalamic tract - EPICRITIC: lemniscal -> form, texture, touch, pressure, slippage, vibration, position (info about internal body: muscles, joints, internal organs)
1. High temporal/spatial resolution
2. Lg, rapidly conducting, myelinated fibers
3. Posterior/posterolateral columns
Which sensory fibers are chemonociceptive? Be specific.
C fibers
What will happen in the case of a lesion to the spinothalamic tract?
- Loss of pain and temp contralaterally, beginning several levels below the spinal cord lesion
What kinds of sensory info do the dorsal columns conduct?
- Vibration
- Joint position sense
- Discriminative touch
Woman presents with bilateral, cape-like loss of sensation in upper extremities, and forehead.
Where would you place this lesion? Dx?
- Midline of the cervical spinal cord —> C2 dermatome extends up to the top of the head (almost forehead)
- Syringomyelia: hole in the center of the spinal cord with LMN findings
Pt comes in for AAA repair. When he awoke from anesthesia post-op, he was unable to move his legs. There were no reported cxs during surgery. On exam, 0-1/5 strength in all leg mm. Lost sensation to pin in both legs up to level of umbilicus. Vibratory sensation and ability to sense joint mvmt in both legs normal.
Where is the lesion? What happened?
- Bilateral lesion in the thoracic cord
- When repairing this, can get thrombus in great radicular artery of Adamkiewicz, resulting in bilateral, anterior lesion of the spinal cord
74-y/o man wakes from sleep with numbness on R side of body. PMH of HTN and diabetes. No other neuro complaints. Elevated threshold to pin, temp, and proprioceptive sensation over right head and body. When touched with a safety pin that was moved from right thorax to his left, he quickly noted the sensation of a sharp object precisely at midline. Vibratory sensation over forehead was felt bilaterally, and only minimally diminished when crossing the midline.
Where was the lesion? What may have caused it? How could you confirm this?
- Left thalamus. Not much of a difference b/t left and right forehead vibration due to radicular nerve fibers. Thalamic lesion classically affects the epicritic and protopathic pathways; hard to affect only these 2 in other parts of the spinal cord/brain stem without affecting other structures
- This could be caused by an ischemic stroke, which tend to occur at night —> do neural imaging (MRI superior to CT in terms of resolution for anatomical structures). Diffusion weighted imaging (MRI) good for detecting ischemia. CT only better for hemorrhage detection.
What is the general arrangement of spinal cord and nerve roots (sensory and motor)?
- MOTOR: motoneuron cell bodies in spinal cord ventral horn, and axons exit ventral horn via ventral roots, traveling in spinal NN to targe mm -> final comm path for motor activation/efferent spinal reflexes
- SENSORY: receptors in skin (cutaneous), mm and joints, and visceral organs, and communicate w/CNS via peripheral processes of pseudo-unipolar sensory neurons with cell bodies outside the spinal cord in the dorsal root ganglia (DRGs)
1. AP’s in DRG cell peripheral process continue in dorsal roots along central process to dorsal horn, then may synapse there, or project up spinal cord to brainstem (depending on type of receptor, and which somesthetic system is involved)

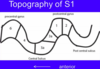
Briefly, describe the dermatomes (image).

What are the classifications of peripheral nerve fibers, incl. motor (table; 8)?
- Motor: A-alpha, A-gamma
- Muscle spindle: Ia, II, A-gamma
- Golgi tendon organ (and Ruffini): Ib
- Posterior/medial lemniscus: A-beta
- Aneterolateral/spinothalamic: A-delta, C
- Autonomic: preganglionic B, postganglionic C

What are some of the different types of somatosensory receptors? At a basic level, how do these work?
- Exteroreceptors: external events
- Proprioceptors: position of joints/muscles in space
- Enteroreceptors: state of internal organs
- Also: chemo, photo, thermo, mechano, and nocireceptors
- Energy from these sources that exist in nature is transduced by sensory receptors into graded electrical signals that are integrated -> when threshold is reached, AP’s are generated

What five types of receptors are found in glabrous and hairy skin?
- PACINIAN CORPUSCLE: lg, lamellar, rapidly adapting mechanoreceptor that detects gross pressure and vibratory skin stimuli (optimal freq 250 Hz)
1. Found in subcu skin, joints, muscle, mesentery - MEISSNER CORPUSCLE: rapidly adapting mechano-receptor sensitive to light touch and vibration <50 Hz
1. Located in glabrous skin, right below epidermis - MERKEL DISKS: slowly adapting mechanoreceptors in skin and mucosa; in glabrous skin, clustered under ridges of fingertips, and clustered into specialized epi structures called “touch domes/hair disks” in hairy skin
- RUFFINI ORGANS: slowly adapting mechanoreceptor in deep layers of glabrous skin that respond to sustained pressure and skin stretch
1. Responsible for detecting objects slipping along skin, and contribute to position sense - FREE NN ENDINGS: no accessory structures; typically responsive to temp and nociceptive stimuli

What is receptor adaptation?
- ADAPTATION: reduced response in face of constant, continued stimulus (see attached image)
1. TOP = no adaptation: AP firing maintained at constant rate as long as stimulus is applied
2. MIDDLE: firing maintained for some time, then freq of AP’s slows, despite maintained stimulus -> slowly adapting receptor
3. BOTTOM: rapid adaptation; brief/transient response

Describe the mechanism of the Pacinian corpuscle sensory receptor.
- Rapidly adapting receptor consisting of free NN ending encapsulated by series of modified Schwann cells (lamellae)
- Pressure applied to lamellae causes lateral mvmt, and corpuscle is distorted; mechanical stimulus transduced to AP at onset of stimulus, followed by adaptation while pressure is maintained
- When pressure released, second AP occurs, so organ signals onset and offset of stimulus, but makes no signals during maintained stimulus
- Transduction via stretch-sensitive ion channels in NN ending, and depolarizations transduced to AP’s at first Node of Ranvier of afferent NN
- Lamellae are accessory structure that determine adaptation in Pacinian corpuscle; w/o lamellae, the corpuscle responds to different stimuli and in a different way

Describe the lemniscal pathway.
- Subcu Pacinian corpuscle (esp. sensitive to vibration) in leg that is rapidly-adapting, connected to lg afferent axon (Ab = T2) that projects via dorsal root into dorsal horn of spinal cord
- Axon continues into ipsilateral, posterior (dorsal) column of spinal cord, and ascends entire spinal cord to ipsilateral medulla (brainstem)
-
First synapse = posterior column nuclei in medulla: nucleus gracilis (L-S), nucleus cuneatus (C-T)
1. NG axons travel in fasciculus gracilis (thin; most medial post column) in spinal cord
2. NC axons travel in more lateral (wedge-shaped), fasciculus cuneatus (T6 is the cut-off) - Axon of 2o neuron (w/cell body in post column nucleus) crosses mid-line of brainstem (decussates) and runs in contralateral MEDIAL LEMNISCUS to part of thalamus involved in somesthesis (synapse #2), the ventral posterolateral nucleus (VPL)
- 3rd order neuron sends axon to ipsilateral 1o somato-sensory cortex, in postcentral gyrus (3rd synapse)

Describe the spinothalamic pathway.
- Free NN ending in skin (cutaneous) of leg (pain, temp receptors usually relatively unspecialized free NN endings) with small, slowly conducting axon (A-delta or C fibers; T3, T4)
- Afferents enter spinal cord via dorsal root, and synapse in ipsilateral dorsal horn (first synapse), unlike lemniscal pathway
- 2nd order neuron (soma in dorsal horn) sends axon across mid-line at same level of spinal cord to contralateral anterolateral funiculus (aka, fasciculus: surface feature indicating underlying axon tract), then turns and ascends through brainstem to VPL in thalamus (synapse #2, contralateral to receptor)
1. NOTE: decussation in anterior commissure of the spinal cord - 3rd order neuron projects ipsilaterally to somato-sensory cortex (post-central gyrus), synapse #3