Exam 2 Flashcards
(730 cards)
What kind of cell is this?

Gram positive
What kind of cell is this?

Gram negative
What color are gram positive bacteria?
Purple
What color are gram negative bacteria?
pink
Which bacteria has a thicker cell?
gram negative
Which bacteria has porins?
gram negative
Where are beta lactamases located in gram positive bacteria?
External space, thus you need to create larger quantities
where are beta lactamases located in gram negative bacteria?
Within in the cell in periplasmic space since it can go through porins
What is the main barrier keeping drugs out of the cell in gram positive bacteria
Bacterial membrane
How many membranes does gram positive bacteria have
1
How many membranes do gram negative bacteria have
two –> inner and outer membranes
What is in gram negative bacteria’s peptidoglycan and how is it cross-linked?
- meso-diaminopimelic acid residue (DAP)
- peptidoglycan is cross-linked by a bridge between the DAP residue of one strand and the terminal D-Ala of another
What is in gram positive bacteria’s peptidoglycan and how is it cross-linked?
- L-lysine residue
- Bridge exists between the L-Lys strand and the terminal D-Ala of the second molecule
What is the enzyme that cross-links the peptidoglycan strands?
transpeptidases
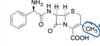
beta lactam antibiotic mechanism of action
- inhibition of transpeptidases that glue the peptidoglycan strands together by cross-linking
- beta lactam antibiotics acylate the transpeptidase Ser residue in the enzyme active site to form stable product, which inactivates the enzyme, inhibiting peptiodglycan cross-linking, which results in a defective bacterial cell wall
What is the reactivity of the beta lactam system due to
- highly strained four-membered ring
Bacterial transpeptidases and catalyzation reactions of host cells
Bacterial transpeptidases do not catalyze reactions with host cell proteins because the bacterial substrate contains unnatural D-Ala amino acid residues that are not found in the host cell proteins
How can resistance to beta lactam antibiotics occur (4)
- decreased cellular uptake of the drug
- mutation of the penicillin binding proteins to decrease their affinity for penicillins
- presence of an efflux pump that pumps the antibiotic out of the cell
- induction or elaboration of bacterial beta lactamases
Rate of hydrolysis of the actylated beta lactamase
Fast, so the enzyme can hydrolyze many drug molecules rapidlyHyd
How much of the US population is allergic to beta lactam antibiotics?
6-8%
How does allergenicity of beta lactam antibiotics occur
Drugs acts like a hapten and acylates host cell proteins, which then raise antibodies that result in an allergic reaction
Cross reactivity in mild reaction of beta lactams
Cephalosporin or carbapenen can be tried since cross-reactivity is 5-15%
Cross reactivity in severe reaction of beta lactams
Cephalosporins and carbapenems are avoided, but aztreonam can be used
*Under the acidic conditions, the main degradation of Pen G are:
- Benzylpenicillenic acid
- Benzylpenillic acid
- Benzylpenicilloic acid
uses achimeric assistance