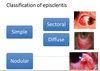
Episcleritis Flashcards
What is episcleritis?
An idiopathic inflammation of the vascular connective tissue that lies between the sclera and conjunctiva
Define Idiopathic
relating to or denoting any disease or condition which arises spontaneously or for which the cause is unknown.
What is scleritis?
A severe inflammatory disease of the sclera which is bilateral in 50% of cases.
How many layers is the sclera made up of and what are they?
3 Layers.
Episclera
Scleral stroma
Lamina fusca

What are the layers of the sclera made up of?
Collagen and proteoglycans
What does the episclera do and where does it lie?
It connects the sclera to the conjunctiva. It lies below the tenon’s capsule.

What are properties of the episclera?
It is a loose connective tissue
- It has a low friction surface allowing free movement of globe in orbit
- It is Highly vascular
- Vessels of the episclera are larger and darker than vessels of the conjunctiva
- Vessels follow a radial pattern
What is the tenon’s capsule also known as?
The Fascia Bulbi
What is the tenon’s capsule?
A thin fibrous sheath that envelops the globe from limbus to margins of optic nerve.
What’s the relationship between the tennon’s capsule and the suspensory ligament of lockwood?
Inferiorly, Tenon’s capsule is thickened to form the suspensory ligament of Lockwood
What is a ligament?
a short band of tough, flexible fibrous connective tissue which connects two bones or cartilages or holds together a joint.
[A suspensory ligament is a ligament that supports a body part]
How are vascular layers of the ocular surface arranged?

What are all the different causes of red eye?
And what are examples of each cause?

How do we diagnose conditions?
SOAP
Subjective - find out what patient complains about ( this can vary)
O- Objective - look at what you see as an eye practitioner
A-assessment- As part of an Investigation - do the right test to get the right Findings
Plan - this could be split into pharmacological or non-pharamcological
(plans should always be time sensitive)
What is the aetiology of episcleritis?
- Idiopathic
- Inflammation of the episclera

Is episcleritis common?
What type of patient is more likely to have episcleritis?
Yes
Females ( 60% of cases are female , 40% of cases are male)

Can we visibly see the episclera?
Normally No as its very deep, however, when it is inflammed we can see it.

Is episcleritis frequently recurrent?
Yes

Is episcleritis self limiting?
Yes
[It is Benign. It does NOT progress to true scleritis]
What age group is episcleritis most common in?
Most common in 40th or 50th decade of life
What are the SUBJECTIVE clinical characteristics of Episcleritis?
- Red eye - usually unilateral
- Acute onset ~12 hours
- Discomfort - mild to moderate –>Non specific irritation i.e. hot/uncomfortable/gritty
- Sometimes mild tenderness on direct palpation (means to touch) (obviously when eyelid is closed)
- Vision unaffected
- Photophobia - (don’t like light) mild to moderate
- Occasionally mild watering (epiphora)
What are the OBJECTIVE characteristics of Episcleritis?
(i.e. what the optometrist sees/is looking for)
Most not associated with systemic condition
- Up to 30% may have systemic association - Collagen vascular diseases: rheumatoid arthritis; systemic lupus erythematosus; inflammatory bowel disease
- Unilateral in half of cases
- May have +ive Previous Ocular History (POH) (i.e. history of earlier episode) - May move from eye to eye
How would the assesment for episcleritis occur and what would we be looking for?
This would be done using a slit lamp.
You would move the conjunctiva to see if it is conjunctivitis or episcleritis.
The anterior chmaber will be quiet - you won’t see any inflammation there.
Use phenylephrine 10%.
How do we identify between episcleritis and scleritis?
We use an important diagnostic tool called phenylephrine 10%.
This will blanch ( this means to whiten out) conjunctival and episcleral vessles.
So basically if the eye is still red after we have added this to the eye, then the diagnosis is scleritis. If the eye isn’t red after installation, the diagnosis is episcleritis.