AMD Flashcards
What is AMD?
Age Related Macula Degeneration - this is a degenerative disorder of the macula causing significant visual loss
Why are we so interested in AMD?
Leading cause of irreversible visual impairment in the Western World (Bourne et al., 2013)
What are the two types of AMD?
Dry and Wet AMD
What may dry AMD also be referred to as?
Atrophic/non-neovascular AMD
What may wet AMD also be referred to as?
Neovascular/exudative AMD
Which type of AMD is more common - dry or wet?
Dry AMD - it accounts for 90% of cases
What are the early signs of dry AMD ?
- Drusen ≥63µm
- RPE (retinal pigment epithelium) hyper/hypo pigmentation
- RPE (retinal pigment epithelium) atrophy
What are the late signs of dry AMD?
Geographic atrophy - sharply demarcted areas of atrophy (i.e. when the center portion of the vision, the macula, starts to lose the actual cells in the retinal layers. )
What are the signs of wet AMD?
- Choroidal neovascularisation (CNV) which can lead to scarring (disciform)
- Macular oedema
- Sub retinal fluid (SRF) - which is a Serous detachment of neurosensory retina
- RPE detachment (also known as a PED) or a tear of the RPE
- Haemorrhages – these can be Sub, intra or pre retinal
- Exudates
Also includes:
- Retinal angiomatous proliferation (RAP)
- Polypoidal choroidal vasculopathy (PCV)
What are the classifications/ degrees of AMD?

What is pathogenesis?
The manner of development of a disease
What is the first sign of dry AMD?
What is a disadvantage of using this as a diagnosing factor for AMD?
Basal Laminar Deposits - these are lipid deposits in Bruch’s membrane (which occur as a result of failure of the RPE to process cell debris).
They are only present in histology (histopathology) i.e. you can only view these on a microscope as a slide from someones eye (not via a direct ophthalmoscopy or otherwise) ( it is highlighted in the picture by the red circle).
[This sign is used as a histopathological marker for AMD)

What is the difference between druse and drusen?
- Plural = drusen
- single = druse
What is the first clinically visible sign of dry AMD?
Drusen
What are drusen?
- Extracellular deposits between RPE and Bruch’s memebrane
- Derived from immune mediated and metabolic processes in RPE, consist of Lipofuscin, amyloid, complement factors
- [These are age-related and common in 60+ px]
What are the different types of drusen?
Hard and soft drusen
What are the clinical features to consider when looking at drusen?
Its size:
- Small ( in which case the type is hard) ≤63µm
- Intermediate 63-125µm
- Large >125µm
The type of drusen:
- i.e. whether it is hard , soft or confluent (meaning a merge of both)?
Whether it is asscoiated with any pigmentary changes e.g. hypo or hyper-pigmentation.
What are the yellow specs in the image shown?

Small hard drusen
[These are not only limited to the macula region but the periphery too]
What are the yellow specs in the image below?

Intermediate (bc of their size) Soft (bc of the blurred circel margins) drusen
What can be seen in the blue circle (2)?
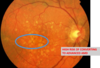
Confluent drusen - when this is present you will be able to see both soft and hard drusen and then areas where they are merging.
In the blue cirle RPE chnages can also be seen.
If both drusen and RPE chnage scan be seen what is the patient t risk of developing?
Adanced / Late (dry) AMD
What RPE changes can be see circled in blue (2)?
Therefore is this a sign of early or late , dry or wet AMD?

Hyperpigmentation
Pigment clumping
Early Dry AMD
What happens in geographical atrophy?
We experience a loss of RPE cells which causes unmasking of choroidal blood vessels
What can be seen highlighted in one of the circles?
Is this early or late , dry or wet AMD?

In the yellow circle - unmasking of choroidal blood vessels can be seen (as a result of geogrpahical atrophy) , areas of hypopigmentation
In the blue circle - Drusen
Black circle - RPE chnages - hyperpigmentation , hypopigmentation.












