EK B2 Ch6 Musculoskeletal system Flashcards
Bone, Skin, Muscle
Bone marrow
where stem cells are born
bone
think of it as living tissue interacting with other phsyiological systems, responding to hormones dynamic rather than scaffolding inside the body that is static!
skeleton anatomy 1
- Vertebrate skeleton has two divisions
- Axial skeleton: skull, vertebral column, ribs, sternum
- Appendicular skeleton: bones in limbs, shoulders (pectoral girdle), hips (pelvic girdle)
skeleton anatomy 2
- Vertebral column has vertebrae, sacrum, and coccyx
- Vertebrae are cervical (neck), thoracic (chest), lumbar (back) and sacral (pelvic)
- Ribcage has 12 ribs, most fused to sternum, a few attached to cartilage or free floating
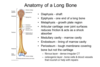
Gross bone structure
- Periosteum is membrane of connective tissue that covers bone
- Compact bone is outer layer, hard and dense
- Spongy bone is inner layer, more porous and less dense
- Diaphysis is long shaft portion of bone
- Epiphysis is bulbous end of bone
- Long bones contain marrow
- Yellow marrow is fatty tissue (in hollow of bone)
- Red marrow is source of blood cells (in spongy bone)
metaphysis and epiphysical line
• Metaphysis is cartilaginous growth zone, between diaphysis and epiphysis (in children) transition area, caritlage converted to bone when long bones grow, how kids get taller cartiaginous region where more bone cells get added! SO IT is sometimes referred to as the growth plate!
There is a line where metaphysis meets epiphysis labeled epiphysis line which shows how far bone growth has gotten, doctor can tell how much more likely they will grow -position of epiphysisal line gives read on how much cartiglate has been pushed into bone

compact bone vs spongy bone
all around parameter of diaphysis is compact bone, hard bone which is really what is responsible for anomotical support, hard part marrow is not compact bone inside of the compact bone surroundings spongy bone, called spongy because pourus so a lot of holes in it, not as strong
Bone marrow in center…
Bone marrow all through center of bone
red bone marrow gives rise to blood cells
yellow marrow which is fatty deposits, so a lot of fat in bone
periosteum
thin membrane around outside of bone called periosteum
cartilage
- Cartilage is an elastic connective tissue, provides joint cushioning
- Cartilage contains chrondrocyte cells and extracellular collagen
- Embryonic skeleton is cartilaginous, becomes bone (ossification)- process still going on in long bones when kid is growing, happens early in skull, carilaginous skeleton gives way to skeleton, but in long bones to get kid to keep going remains carilaginous until bone growth is finished
- Metaphysis is cartilaginous, permits bone elongation
- Adult cartilage in ear, nose, ribcage, between spinal vertebrae, and in joints as fully grown adults have bits of cartilage in ears, verebtrates other joints because it provides really good cushioning* really really painful when two bones rub directly together in a joint so having cartilage there to cushion that keeps it comfortable for people
what kind of cells make up cartilage
chrondrocyte cells
osteon
= Haversion system what looks like if have cross section osteocytes are bone cells
canal in middle of one of these systems called Haversion canal where blood vessels and nerves are found, the osteocytes bone is hard as it grows and gets stronger it creates this hard extracellular matrix around itself, but osteocytes are living cells in bone, problem for evolution to solve to keep these cells alive in bone even when building fortress around themselves so bone would be strong, system of canals and little passages haversian canal is where blood vessels are, like Venice, so oxygen nutrients move out through that canal system diffuse out and reach osteocyte, then carbon dioxide and waste go back through center and enter blood supply, without it osteocytes would not be able to stay alive

Osteoblasts
Osteoblasts build up bone (ossification) BLASTS BUILD BONE UP
Osteoclasts
Osteoclasts break down bone (resorption) BREAK DOWN BONE. CHEW BONE UP *not to be confused with reabsoprtion
Bone remolding
Bone constantly beign adjusted, broken down or built up, can change shape, its an active tissue, as bone is developing osteoblasts, the bone building cells are what is really active
Osteoblasts secrete collagen* collagen forms a web on that web there are these crystals called hydroxy appetite crystals that get deposited on the collagen that makes bone hard and what gives bone its strength, made of calcium, phosphate and hydroxide ions*
crystals deposited on collagen
hydroxyapatite, but if unpack what is in a hydroxyapatiate crystal made of= it is made of calcium, phosphate and hydroxide ions to make hard crystal structure what gives bone its strength
osteocytes
trapped in extracellular matrix with hydroxyapatite crystals, older cells so need whole osteon system set up to nurish those cells!
Osteocytes are the longest living bone cell, making up 90–95% of cells in bone tissue in contrast to osteoclasts and osteoblasts making up ~5% (40). Osteocytes form when osteoblasts become buried in the mineral matrix of bone and develop distinct features.

Hyperactivity of osteoclasts →
Hyperactivity of osteoclasts → osteoporosis, which is when bone gets fragile and brittle and broken down, if osteoclasts are too active can weaken bone breaking down bone and making it less strong
parathyroid hormone and calcitonin
inc amount of calcium in blood
calcitonin dec amount of calcium in blood
so parathyroid hormone stimulates osteoclasts so if trying to release calcium from bone by breaking down bone, cells stimulated are osteoclasts break down bone
ex why bones broken down ballerinas not enough calcium, on flip side calcitonin trying to reduce amoutn of calcium in blood will stimulate other kind of cells to build bone, after age of 30 don’t build bone* so after that having enough calcium is about maintaining bone mass, which will then be there for a lifetime
bone mass and aging
- Bone mass is gained only until age 30
- After age 30, bone loss exceeds bone formation
- Very low bone mass → osteoporosis
- Postmenopausal women more susceptible to osteoporosis after menopasue when women have less estrogen much more susceptible to osteoporosis, why falls and hip fracture are such a big concern when taking care of elderly especially elderly women
Tendon
Tendon attaches muscle to bone
THINK:
“Tara must be a bully” tendons connect muscle to bone
joints are classified by
how much joints can move relative to each other
skull is a good example of that, we don’t want bones of cell skipping around, called immovable or fibrous joint btw bones
slightly movable joints- best example verbrate, move around a bit to absorb shock, fact can move a bit helps absorb shock
have the joint that can move the most bones can move the most, called free movable or synovial joints
synovial fluid
Freely movable/synovial joints = full movement (e.g., knee, elbow, shoulder)
Synovial joints have capsule with synovial fluid, are covered by connective tissue
can get infections, tares in ligaments connecting two bones at the knee, tons of conditions that involve these joints like knee or shoulder
cartilage critical in joints
muscles in the body

muscles in body come in pairs! one has to relax one has to work, agonist produces movement, antagonist one that if it contracted it would cause the opposite movement!

muscle class
• Abductor moves away from the midline (lifting arms, or moving away fingers)
“I have to move away from my diet to get abs”
• Adductor moves towards the midline (adding to center)

muscle

- Muscle generates force and permits movement
- Muscle contraction squeezes vessels, aiding in blood circulation and lymph movement
- Muscle contraction important for thermoregulation (shivering releases heat)
- All muscle contraction depends on Ca2+ skeletal muscle plays a really big role with circulatory system, keep blood moving through veins through action of skeletal muscle, need skeletal muscle movement to keep circulation normal, muscle contraction also important for thermoregulation, when get cold use our muscles to shiver and produce heat** in everything we say about muscle contraction Calcium plays a starring role, different muscle cells but all muscle cells involve calcium***

skeletal muscle
Skeletal is striated
voluntary
multinucleate
innervated by somatic nervous system
striated= means looks like it has stripes
voluntary= so we can decide to contract our skeletal muscle or we can decide to run or lift a cup or whatever
multinucelated= meaning really striking when look at skeletal muscle cells, sooo weird have 20 nuclei look like row of eyeballs but normal for skeletal muscle cells
innervated by somatic nervous system, called motor system or the somatic system, the nerves that give instructions for skeletal structures, these are the nerves somatic neurons that axons extend a great distance from spinal cord to big toe synapse with acetylcholine there is a neuromuscular junction there between neuron and skeletal muscle cell, when acetylcholine binds to its receptor in skeletal muscle cell the muscle cell contracts

Cardiac

cardiac muscle cell is striated, involuntary, 1 or 2 nuclei, innervated by autonomic nervous system
- 1 or 2 nuclei v important**
- Contracts and relaxes rhythmically, coordinated by a pacemaker
- Cardiac muscle fibers/cells are electrically coupled by gap junctions with structure called intercalated discs in thin heart muscle need free flow of ions from one to the next to get the whole heart to contract all together come back to this in circulatory chapter this is just a little preview
- Intercalated discs are physical and electrical junctions between muscle fibers
- Cardiac muscle fibers are branched, in a mesh
- Innervated by autonomic nervous system, which can influence contraction rate/strength
- Like skeletal muscle, cardiac muscle is striated, but unlike skeletal muscle, cardiac muscle cannot be consciously controlled and is called involuntary muscle. It has one nucleus per cell, is branched, and is distinguished by the presence of intercalated disks.

smooth muscle
- Smooth muscle is not striated, is involuntary
- Organization of muscle is less regular
- One nucleus per cell
- GI tract, blood vessels, arteries, bladder
- Smooth muscle fibers may be connected by gap junctions
- Contracts slowly and contraction is sustained
- Innervated by autonomic nervous system, meaning automatic not voluntary

Neurogenic =
Neurogenic = nerve impulse generates muscle contraction
-muscle cells must have an input from nervous system to contract
Myogenic =
• Myogenic = muscle generates its own contraction, able to generate own contractions, in petri dish and watch it beat cool and weird, can still be influenced by nervous system, have ability to contract on own but nervous system can tell them to contract faster or slower, still controlled by nervous system in ways that are really important, so skeletal muscle is neurogenic, it has to have input from nervous system, acetylcholine, nervous muscular junction
cardiac and smooth muscle are myogenic but nervous system still plays a role
When sarcometer contracts what changes?
H and I change, ones that spell Hi go away
SR
stores a lot of calcium, lot in SR, as action potentials go down through its tubules they trigger voltage gated calcium channels on the membrane of the SR
- so when the action potential gets there calcium channels open in the membrane of the SR, and we said that the Ca concentration in SR is much greater and Ca concentration is lower in cytoplasm, means calcium is going to go out into cytoplasm, also said calcium is crucial for muscle contractions
MOVES DOWN ITS CONCENTRATON GRADIENT*
Calcium greater in SR and less in cytoplasm, so going down gradient!!! Why want this!
Synaptic terminal of motor neuron
acetylcholine binds to muscle cell, get action potentials, action potentals go deeper into cell cause calcium to be released into cytoplasm
head of myosin
The head of myosin has to bind to actin, don’t want myosin binding all the time or contracting all the time, see how it is regulated, if look closely on lefthand side of figure, if you see how look at orange beads of actin and grey rope wound around them, little holes in beads being covered up by grey rope –>what that is showing is that the little holes represent binding sites where myosin can attach to actin
Grey rope is a protein called tropomyosin
And at rest tropomyosin is covering the binding sites where myosin would bind to actin, and then there are also these purple proteins called troposin

Role of Ca2+ in muscle contraction
binds to troponin, troponin protein changes shape, pushes tryopomosin out of the way and exposes the sites on actin where myosin can bind
point of diagram when calcium binds to purple tropoin protein causes this shift so actin grey stuff moves and myosin can actually bind to actin*
trypomosin= grey rope
protein troponin= purple thing, Ca2+ ions bind to troponin protein on actin filament

power stroke cycle
trying to understand how action potential, signal from neuron causing action potential makes sacromere go in and shorten how myosin binding to actin can pull actin so more overlap between the two kinds of protein and that is what this image is about
calcium makes actin available to be bound to myosin but actual contraction is powered by ATP*** how exactly does ATP cause actin and myosin to move, kinda of weird mechanism
- myosin head low energy confirmation bound by ATP, not hydrolyzed or used yet
- ATP is hydrolyzed to ADP and Pi. The potential energy from ATP is transferred to myosin head, so what we are suppose to see is that the myosin head is in a different position in its high energy confirmation
- when myosin is in its high energy confirmation across bridge forms, so that just means myosin actually binds to actin
- ADP and phosphate group are released, potential energy stored in myosin is being used or converted to kinetic energy to push the actin push the thin filament moves toward center of sacromere
- Then returns to low energy confirmation, attached to actin takes ATP coming in in step five to release the myosin from the actin, ATP needed to detach from actin, pushing actin more and more but every time and cycle requires another ATP

why need atp for myosin….
idea need atp for myosin to let go of actin helps explain rigermortis, bodies stifen after they die is becuase not producing atp anymore and so all through the body myosin gets stuck to actin in a rigid state*
power stroke cycle 2
- if do muscle contraction and then really relax way to stop this is to pump calcium out of cytoplasm
- another thing ATP is important for in muscle cells is to sequester and pump ATP back into sacroplasmic reticulm, then if you remember that mechanism with tropomyosin, if calcium is not present then the binding sites on actin for myosin will get covered up again* so then myosin cannot bind to actin and muscle contraction cannot occur* how we would relax at the end of all of this

muscles, atp and energy
Muscle needs lots of ATP and is rich in mitochondria
- Rigor mortis is ATP depletion, can’t release myosin cross bridges
- Second storage compound is creatine phosphate
- Creatine phosphate + ADP → creatine + ATP
- Third storage compound is glycogen → breakdown to glucose → ATP
- Repeated contraction causes O2 debt and ATP depletion
- During O2 debt, anaerobic glycolysis produces lactic acid
Creatine phosphate
Create a little of atp through substrate level phospholraytion
More creatine in muscle cells can make more atp
Muscle cells can make some small additional amount og ATP from creatine phosphate and that gives them extra atp, another way can boost their atp ability*
when exercising hard
can do anerobic respiration and fermentation, causes lactic acid to build up in cells what is the muscle burn you get when exercising really hard
temperature and muscles
when muscles contract a lot of atp energy is released as heat, why get pretty hot when exercise but can harness that when cold by shivering
tetanus and muscle tone
- Single electrical stimulation of muscle causes a simple twitch
- Summation of twitches provides a smooth contraction
- Smooth, sustained contraction is called a tetanus
- Muscle tone (tonus) occurs from partial contraction of some muscle fibers
tonus
muscle tone contraction all the time, just sitting there have some muscle tone to maintain position
fast twitch muscles
what sprinters need, rely on anaerobic respiraiton
glycolysis through glycogen
fast twitch muscles do not have as much of a blood supply so look white, lesser blood supply is because function with less oxygen do more anaerobic respiration, innovated by motor neurons with very large diameters, very frequent signals or action potentials can be delivered
Or like body builders*
fast twitch muscles 2
great for generating bursts of force but white fibers get tired easily so sprints rather than marathons
Fast-twitch = white muscle
Fast-twitch has few mitochondria and little myoglobin
Fast-twitch gets energy from glycolysis and glycogen
Fast-twitch innervated by motor neurons with large diameter axons
Good for generating lots of force quickly, but fatigues easily
slow twist muscles
good for marathon runners, sustained activity, want slow twitch muscles, do everything to have more slow twitch muscle, if do a different kind of exercise, long distance runners have to do everything to have as much red fibers as they can have
Slow-twitch = red muscle
Slow-twitch has lots of mitochondria, myoglobin, well vascularized
Slow-twitch gets energy from aerobic respiration
Slow-twitch innervated by motor neurons with small diameter axons
Good for long-term aerobic exertion
skin
- Skin is a multifunctional organ
- Acts as a protective covering from microbes, injury, UV light
- Provides sensory reception (e.g., touch, temperature)
- Relatively impermeable to water
- Key for thermoregulation
- Skin has excretory function via sweating (water, salts, urea) how can cool off by sweating
- Hair, nails, oil glands, milk glands derive from skin
Callus
Callus = area of skin thickened in response to irritation
skin layers, epidermis
- Three major skin layers: epidermis, dermis, and hypodermis/subcutaneous
- Epidermis is outermost layer of skin, has 5 layers or “strata”
- Stratum corneum is top protective layer of epidermis (dead cells) top layer
- Stratum basale is deepest layer of epidermis (dividing cells) bottom layer, lowest level of epidermis is where we have stem cells dividing and what basically happens is cells divide and differentiate and move up through layers to top of outer layer of epidemis, by the time they reach very top layer of stratum corneum dead and sluff off, so epidermis is constantly regenerating itself cells constantly differentiating and moving up through epidermis

epidermis pigmented
- Epidermis is pigmented with melanin, produced by melanocytes -produces diff ethnicities, its role is to absorb uv light which causes dna damage so of course we want to absorb it
- Melanin absorbs UV light, protecting skin
Dermis
if get cut and bleed means gone down to dermis where blood vessels are
- Dermis is underneath epidermis
- Dermis contains blood vessels, sweat glands, hair follicles, and collagen, less collagen in dermis causes skin to sag
hypodermis
- Subcutaenous/hypodermis is underneath dermis
- Subcutaenous layer is mainly fat, provides insulation, lack of fat here is skin saging as well again

skin and thermoregulation
• Skin regulates body temperature through radiation and sweating
• Skin is cooler than the rest of the body***
• Dilated capillaries promote heat loss, if body wants to conserve heat capillaries can constrict, other way to use skin to cool off is sweating
• Constricted capillaries conserve heat
- Sweating is critical to regulate internal body temperature; when sweat released onto surface of skin it evaporates, cooling process
- During high activity, body temperature must be maintained
- Sweat allows additional heat loss through evaporation
skin and thermoregulation 2
part of homeostatsis is about keeping body temperature within narrow range, when talking about nervous system really hypothalamus sending directives in terms of what the body needs to do in terms of warming up or cooling down
metaphylsis border…
border called growth plate or ephiphyseal line, metaiphyseal plates; bone replaces cartilage at the epiphyseal plate on an xray this spot can tell how much more the kid is going to grow, so represents a border btw place that is still cartilage and bone, if lots of cartilage that hasn’t turned into bone yet kid will still keep growing; if not much left kid is done growing, or getting taller
it is called both also called metaphylsial plate, ephiphyseal line
bone resporption means=
MEANS BONE BREAK DOWN**** which of the following would contribute to osteoporosis, a dec in bone density often found in post menopausal women- what osteoclasts do and what parathyroid hormone would inc, the inc bone resportion
which of the following decreases when a sarcomere contracts?
- boundaries of sarcomere are Z lines, when sarcomere contracts Z lines get shorter! closer together! -the purple represents the myosin, thick filaments and the orange represents actin the thin filaments; sarcomere contracts when myosin and actin slide relative to each other meaning they overlap with each other more****
- region of overlap inc so how sarcomere as a whole gets smaller, like hands sliding past each other overlapping more, none of your fingers are getting shorter just overlapping more
- the I band is actin with NO OVERLAPPING MYOSIN, so when do have more overlap I band will get smaller*
-A band represents the whole length of the myosin, D just says length of thin filaments don’t get smaller just overlap more with myosin*
-H represents thick with no overlaping thin filaments, so could also say this changes because get NO overlap, so that area dec

- A drug responsible for smooth muscle relaxation would be least likely to cause=
- this turns on where you have smooth muscle!*** so this drug is only going to target smooth muscle, so can definitely cause A. dilation of peripheral blood vessels, because that is smooth muscle, same with b. relaxation of msucles along with gastro-intestinal tract
- c. is skeletal muscle, relief of pain caused by muscoskeletal tension in the forearm
- d. reduced musclar tension in bladder wall, this is also true becuase bladder surrounded by smooth muscle*
- Calcium ions are critical for contraction of:
- do not need all same muscle contractions, exactly what Calcium does for skeletal but need calcium for all three types for how to contract: cardiac, smooth, and skeletal muscle all need calcium
- answer all of the above!

Atp’s role** in power stroke
- ATP binds to myosin head before myosin is attached to actin, which allows myosin to release from actin
- atp binds to myosin allows it to let go of actin
- number 1. atp bound to myosin
- second step for ATP to be hydroyzled, energy in ATP gets transfered to myosin head as go from 12 oclock to 3 oclock
- myosin head high energy confirmation, energy from atp now in myosin head*, atp’s job is done in a way
- THEN myosin binds to actin that is the point here, you do not need ATp in the step where myosin binds to actin** cross bridge, energy in myosin head is used to push actin to the left
- 9’ oclock myosin head in low energy configuration, need another ATP to release myosin from actin, then cycle can start over!
- myosin pushes actin then lets go, then pushes and lets go happens many many times in course of single muscle contraction* lots of actions of myosin to make shortening of sarcomere and therefore shortening of the whole muscle*

anatomy of long bone image

voluntary muscle ex.
skeletal muscle, like cerebral cortex
spinal cord also contributes to voluntary control of muscles, remember if something controlled by me* if I control the muscle function then I will use either my cortex or my cord which happens to start with a C*
so controled and voluntary= cortex or cord comes in handy*
involuntary control ex.
cardiac and smooth muscle
stuff going on beyond me, beyond my self control, if beyond me will have to use either brain stem or neuronal tissue that sits besides spinal cord to cause involuntary contraction of muscle*
myosin steps
- myosin uses atp to crawl around/down actin rope to create ATP energy
- step 1= 1. atp binds to myosin head, 2. myosin releases actin** so that is what happens it touches actin, atp comes and it gets released! so in the next step looks to have released* ATP attached to it still* now on ext step 3. atp hydrolyzes phosphate gets pulled off of it*
- step 2= atp goes to ADP + Pi phosphate group, releases energy to cock myosin protein into a high energy state* so step 2 this thing gets hydrolyzed releases energy, know atp is the energy currency of biolgoical systems* can really imagine it as changing confirmation spring loads that protein to go into a step to crawl along the myosin, so step 2 plus energy, then can say it cocks the myosin protein or enzyme to high energy* can imagine it whinds the spring or loads the spring to high energy confirmation* high energy confirmaton of protein just means shape so phosphate group still attached but gets detached from the rest of atp to adp so changes confirmation with energy protein in new shape
myosin steps part 2
- atp bids to myosin “head” –> myosin releases actin. end of step one causes myosin proteint o get released, then at end of step 1 naturall step 2 hydrolzyes to atp phosphate releases enrgy allows myosin protein to get cocked at high energy protein next run of actin filament
- so at end of step 2 “cocks” the myosin protein to high energy conformation* now when that phosphate group releases* so when started just sitting here
- step 3- phosphate group released from myosin, releases energy of cocked position, causing myosin protein to push on the actin, its the power stroke in enegine the mechanical movement, original release atp to adp in phosphate puts in spring loaded position, when phosphate releases it it releases the spring* what that does is it pushes on the actin filament* pushes on actin, if imagine myosin fixed then whatever actin it is attached to moves to the right, where get fundamental muscle reaciton
- step 4. ATP released and then we are exactly where we were before did step 1, just one rung furhter to the left on actin molecule*
where is tropomyosin
- so tropomyosin protein coils around actin*
- important thing about it coiled around it and attached to actin by another protein called troponin*
- when a muscle is not contracting, turns out tropomyosin is blocking myosin still an area of research not 100% clear tropomyosin blocks myosin to attach to actin where it normally attaches, or sometimes it is attached to actin but stops it from releasing and sliding, so bottom line is tropomyosin blocks the myosin head*** from crawling up the actin*** either physically blocking active binding site
- only way to make it unblocked is for troponins to change shape, only way to do that is high calcium ion concentration*** high enough concentration of calcium ions binds to troponin, changes confirmaiton of troponin enough to mvoe confirmation of tropomyosin

tropomyosin 2
normally blocks the myosin head
when have a high calcium ion concentration* they bind to troponin* and then the troponin changes their confirmation and moves the tropomyosin out of the way* then these guys can start walking up the actin, or pushing the actin to teh right, however want to view it
- if low calcium ion concetration then calciums get released from troponin, if concetration becomes really low here these guys start to live so troponin goes back to standard confirmation* and that makes the tropomyosin block the myosin again**
without calcium…
tropomyosin is blocking hte ability of myosin to attach where it needs to attach and slide up actin
if calcium concentration is high enough they will bond to troponin, nails down tropomyosin wound around actin, when change their confirmation with calcium ions it moves the tropomyosin out of way so myosin can do what it does
building up a way for muscles to contract and how to control muscles contracting if high calcium concentration within cell the muscle will contract!!
if low calcium concetration then these will release, be blocked and muscle will relax again!
sarcoplasmic reticulum
- it has calcium ion pumps on membrane
- what these do is they are atpases, meanign use atp to fuel pumps, have atp come in atp attaches to it, calcium ion attaches to it
- when atp hydrolyzes into adp and phosphate group (Pi) changes confirmation of protein and pumps calcium ion in
- so resting muscle has a very high concetration of calcium ions on the inside; when muscle needs to contract calcium ions get dumped out to cytoplasm of cell, can bound to troponin and do everything just talked about- what we care about how does it know when to dump rest of its ions inside cell!
- this area is what the actin filaments and myosin heads and all of the rest of the troponin and tropomyosin, all exposed to environment over there
for muscle cells, acetylcholine
- released into synpase, so receptor on msucle cell get acetylcholine and then allows sodium to flow into muscle cell
- causes action potential in muscle cell, postive charge high enough to threshold channel triggers next vltage gated channel allowing more sodium to flow in
- then action potential goes down T tubule, chemical signal goes down next action potential down t tubular connected to sacroplasmic reticulm, get positive enough right around there complex of protein triggers release of calcium!
- when action potential gets far enough, mystery box triggers open for Ca ions to escape sarcoplasmic reitculum outside into inside of cell, cytoplasm of cell
- so when muscle relaxes Ca goes into sarcoplasmic reitcum then when it gets signal dumps it back out into cytoplasm
6.
actin
thin filaments
Think: “All actresses try to be thin”
Image of role of Ca2+ in cell
TO BIND TO TROPONIN PROTEIN and change shape, pushing tropomyposin out of the way

tetanus
• Smooth, sustained contraction is called a tetanus
Myosin
Thick filaments
think: going on instagram everyday is a sin, makes you thick aka dumb
sins make you thick, dumb
each muscle fiber
is composed of a bundle of myofibrils, which are composed of actin and myosin (the thin and thick filaments)
thermoregulation by muscle
Contraction is ~ 40% efficient, rest of ATP energy is released as heat
Involuntary shivering is body producing heat by muscle contraction
Two types of muscle fibers
fast-twitch and slow-twitch
Calcitonin
Calcitonin decreases blood Ca2+ → stores Ca2+ in bone
Calcitonin promotes bone formation and osteoblast activity
Parathyroid hormone
Parathyroid hormone increases blood Ca2+ → releases Ca2+ from bone
Parathyroid hormone promotes bone resorption
Bone composition and Haversian system
Bone is composed of cells and a hard matrix
Matrix contains collagen and hydroxyapatite (calcium phosphate)
Haversian systems/osteons are circular units of organization in bone
Haversian canals = microscopic canals that contain capillaries and nerves
Lamellae = concentric matrix layers around Haversian canals
Lacunae = pits, occupied by osteocytes (bone cells)
Canaliculi = canals connecting lacunae and Haversian canal
Haversian canals 2
Haversian canals = microscopic canals that contain capillaries and nerves
Lamellae
Lamellae = concentric matrix layers around Haversian canals
Lacunae
Lacunae = pits, occupied by osteocytes (bone cells)
Canaliculi
Canaliculi = canals connecting lacunae and Haversian canal
Bone remodeling
Bone is living and is remodeled continuously (turnover)
Critical for repair and Ca2+ regulation
Two key cell types=
- Osteoblasts build up bone (ossification)
- Osteoclasts break down bone (resorption)
Osteoblasts secrete collagen, allowing hydroxyapatite deposition → hard matrix
Osteoblasts trap themselves in matrix, become osteocytes
word remodeling stands for resportion and formation!
Bones thicken in response to mechanical stress (e.g., stronger muscles, physical activity)
Ligaments
Ligament attaches bone to bone
BBL
Joint
Joints are meeting points of bones
Immovable/fibrous joints
Immovable/fibrous joints = fused bones in skull
Osteoarthritis
Osteoarthritis = cartilage degeneration in joint, joint pain, and inflammation
Muscle pairs and joints
Muscles act in pairs (flexor, extensor)
Agonist is muscle that produces the motion
Antagonist is muscle that elicits the opposite motion
Agonist contracts, antagonist relaxes
Example: to bend arm, biceps = agonist, triceps = antagonist
z-line
Neighbouring, parallel lines that define a sarcomere.
motor units and neuromsuclar junctions
Skeletal muscle is controlled by motor neurons
Motor unit = one motor neuron and the muscle cells it controls (can be 1000s)
Neuromuscular junction = synapse between axon terminal and muscle
Neuromuscular junction = motor end plate
Acetylcholine release from axon causes depolarization of muscle fibers
Depolarization of muscle fibers causes action potential in muscle
Skeletal muscle structure

A skeletal muscle is composed of 1000s of elongated cells
One muscle cell (many nuclei) = a muscle fiber
Plasma membrane = sarcolemma
Cytoplasm = sarcoplasm
ER = sarcoplasmic reticulum
T-tubules are tubular invaginations of sarcolemma
T-tubules permit rapid depolarization and action potential propagation
Each cell/fiber contains several myofibrils
A myofibril is an end-to-end assembly of many sarcomeres
The sarcomere is the unit of contraction

Sarcomeres 1

Striations in muscle = regularly repeating sarcomeres
Sarcomere has thin actin filaments and thick myosin filaments
Z line at end of sarcomere is region of anchored actin filaments
A, H, I, M bands are within sarcomere
I band = actin only (with no overlap of myosin)
H zone = myosin only (with no overlap of actin)
M band = band in center of H zone, crosslinks and aligns myosin filaments
A band = full length of myosin plus any overlapping actin
Myosin forms cross-bridges with actin molecules in A band
During contraction: I band and H zone shrink
Contraction is based on filaments sliding past each other
Actin alone not getting shorter or myosin alone not getting shorter but they slide so overlap more with eachother

I band
I band = actin only (with no overlap of myosin)
The area adjacent to the Z-line, where actin myofilaments are not superimposed by myosin myofilaments.
H zone
H zone = myosin only (with no overlap of actin)
The area adjacent to the M-line, where myosin myofilaments are not superimposed by actin myofilaments.

M band
M band = band in center of H zone, crosslinks and aligns myosin filaments
The line at the center of a sarcomere to which myosin myofilaments bind.
A band =

A band = full length of myosin plus any overlapping actin
The length of a myosin myofilament within a sarcomere.

Molecular mechanism of muscle contraction
Motor neuron releases acetylcholine at neuromuscular junction
Acetylcholine binds receptor and causes depolarization of sarcolemma
Action potential travels across membrane and through T-tubules
Depolarization triggers Ca2+ release from sarcoplasmic reticulum via Ca2+ channels
Ca2+ ions bind to troponin protein on actin filament
Troponin protein changes shape, pushes tropomyosin away
Myosin-binding site on actin filament is now exposed
Myosin head (bound with ADP + Pi) binds actin filament
Myosin head releases ADP + Pi and undergoes power stroke
Actin filament is pulled during power stroke
ATP binds myosin head, allowing myosin to detach
ATP is hydrolyzed to ADP + Pi, cocking myosin head
Cycle repeats and muscle contracts
When motor neuron stops firing, acetylcholinesterase degrades free acetylcholine
Ca2+ is pumped back into sarcoplasmic reticulum
Muscle relaxes
Sarcomere 2

- many sarcomere contracts at same time, when a sarcomere gets shorter thousands and thosuands of times then the muslce as a whole gets shorter, this is one little unit. but if every one little unit gets shorter than macroscopically big picture hte muscle as a whole is getting shorter causing movement of some kind
- edges of sarcomere are defined by Z lines, those red vertical lines at the edges
- within the sarcomere there is myosin which is red in this picture and actin which is blue
- notice top picture and bottom picture: ends/edges moving closer in, those red vertical lines that define the left and right side slide in closer together adn then you have mroe overlap between teh blue and hte red *** the blue itself is not shortening if to measure the length of the red by itself not shortenign just overlapping more
- H band defined in middle by definition, so it is the part where only have myosin with no overlaping actin, so when the contraction which has more overlap occurs then the H band by definition gets shorter* gets smaller and the part within overlap goes away becuase you have mroe overlap* true of I band also shrinks actin blue without overlaping red and that you have less of
whole idea with contraction mroe overlap, and H and I are both defined as regions without much overlap so they shrink*

The sliding filaments model (sarcomere contracting)

The sarcomere and the sliding filament model of contraction: During contraction myosin reaches along actin myofilaments compressing the I and H bands. During stretching this tension is release and the I and H bands expand. The A-band remains constant throughout as the length of the myosin myofilaments does not change.
The amount of force and movement generated by an individual sarcomere is small. However, when multiplied by the number of sarcomeres in a myofibril, myofibrils in a myocyte and myocytes in a muscle, the amount of force and movement generated is significant.
When they overlap more many sarcomeres would be contracted and when they loverlap less the sarcomeres and the muscle are relaxed*
Z lines are the end of sarcomere, the boundaries of the sarcomere they shrink as well during contraction, causes a dec in distance btw the z lines of the sarcomere*
During contraction myosin ratchets along actin myofilaments compressing the I and H bands. During stretching this tension is release and the I and H bands expand. The A-band remains constant throughout as the length of the myosin myofilaments does not change.

T- tubules details
t-tubules- invaginations or folds in plasma membrane, plasma membrane dips down into the cell but it forms these tubule structures going deeper into the cell which helps action potential which initially going down memraben to be conveyed deeper into the cell*
- those red arrows represent action potentials in image traveling along plasma membrane, and dive down through the t-tubule system, just these kind of like invaginations
NOT MICROTUBULES these are just tunnels**** which allow action potentials to get down to where sarcoplasmic reticiulum is and then voltage changes can cause calcium to be released from SR, then calcium can go and bind to trypoonin and then etc but the action otential needs to get down to where the SR is becuase tha tis where the calcium is, how to think about tubules path action potentials can follow deeper into cell so can trigger next steps in muscle contraction*
this image of neruon synapsing on muscle cell

what does innervated mean?
if certain muscle cell is innervated by certain part of nervous system means that is the part of nervous system that sends signals to that muscle cell: so say cardiac muscle is innervated by autonomic nervous system specifically parasympathetic and sympathetic branch, part of nervous system that synapses with cardiac muscle, giving signals to cardiac muscle**
Sliding filament model 2

The sarcomere is the region in which sliding filament contraction occurs.
During contraction, myosin myofilaments ratchet over actin myofilaments contracting the sarcomere.
Within the sarcomere, key regions known as the I and H band compress and expand to facilitate this movement.
The myofilaments themselves do not expand or contract.
The sliding filament model describes the process used by muscles to contract. It is a cycle of repetitive events that causes actin and myosin myofilaments to slide over each other, contracting the sarcomere and generating tension in the muscle.
To understand the sliding filament model requires an understanding of sarcomere structure. A sarcomere is defined as the segment between two neighboring, parallel Z-lines. Z lines are composed of a mixture of actin myofilaments and molecules of the highly elastic protein titin crosslinked by alpha-actinin. Actin myofilaments attach directly to the Z-lines, whereas myosin myofilaments attach via titin molecules.
Surrounding the Z-line is the I-band, the region where actin myofilaments are not superimposed by myosin myofilaments. The I-band is spanned by the titin molecule connecting the Z-line with a myosin filament.
The region between two neighboring, parallel I-bands is known as the A-band and contains the entire length of single myosin myofilaments. Within the A-band is a region known as the H-band, which is the region not superimposed by actin myofilaments. Within the H-band is the M-line, which is composed of myosin myofilaments and titin molecules crosslinked by myomesin.
Titin molecules connect the Z-line with the M-line and provide a scaffold for myosin myofilaments. Their elasticity provides the underpinning of muscle contraction. Titin molecules are thought to play a key role as a molecular ruler maintaining parallel alignment within the sarcomere. Another protein, nebulin, is thought to perform a similar role for actin myofilaments.

cross bridge cycle
The model of contraction- the molecular mechanism whereby myosin and acting myofilaments slide over each other is termed the cross-bridge cycle. During muscle contraction, the heads of myosin myofilaments quickly bind and release in a ratcheting fashion, pulling themselves along the actin myofilament.
At the level of the sliding filament model, expansion and contraction only occurs within the I and H-bands. The myofilaments themselves do not contract or expand and so the A-band remains constant.

Thin and thick filaments are organized into functional units called ___
sarcomeres



