Diabetes IV - Renal Manifestations Flashcards
Common causes of nephrotic syndrome

Anti-GBM disease summary

Membranous nephropathy summary
- Nephrotic syndrome
- Caused by sub-epithelial IC formation within the urinary space and subsequent basement membrane proliferation
- Most common in adults
- EM: “Spiked” pattern of BM with large, sub-epithelial, electron dense deposits
- IF: Granular staining with IgG and C3 (usually IgG4)
- Can be primary or secondary
- Primary is idiopathic
- Secondary: caused by autoantibodies that were generated in response to infection, malignancy, autoimmunity, or medications
- Treated by addressing underlying cause if secondary, or with steroids if primary

IgA nephropathy summary

Hydroureter and hydronephrosis
Hydroureter: dilation of the ureter due to distension with fluid
Hydronephrosis: dilation of the renal pelvix and misshapen papillae due to distension with fluid
Primary vs secondary FSGS

Common causes of nephritic syndrome

Clues that you are dealing with idiopathic or adaptive FSGS

Membranous glomerulonephritis summary

The dynamics of K+ in the pathophysiology and management of DKA
- At the onset of symptoms, insulin deficiency causes a shift of potassium out of cells
- However, potassium is also lost due to diuresis with glucose and ketones
- These urinary losses are then limited due to RAAS activation after a period of water loss, resulting in reduced distal Na+ delivery
- Treatment: Potassium is likely to fall with the infusion of saline to treat volume depletion, as RAAS activation will diminish and distal Na+ delivery will increase. Insulin administration will also cause K+ to fall as it is shifted intracellularly.
If a diabetic patients presents with HHS, what affect will treating the HHS have on serum sodium?
Sodium will go up.
Doesn’t matter if they are hyponatremic, normonatremic, or hypernatremic.
As glucose re-enters cells, it will take water with it, decreasing the volume in which the extracellular sodium is dissolved.
Risks of using RAAS blockers in slowing progression of diabetic nephropathy
In the short term, GFR will be worse! Creatinine will rise due to interference with GFR-preserving RAAS mechanisms. However, this will soon be compensated for and proteinuria and blood pressure will decrease.
There is also an increased risk of AKI given that we are blocking a protective mechanism for low-flow conditions, as well as hyperkalemia since we are blocking the principal mechanism of aldosterone production.
In diabetes, the initial insult to the kidney is . . .
. . . local damage to the glomerular capillaries, characterized by thickening of GBM. This will present as “hyperfiltration,” and reduced creatinine, but accompanied by microalbuminuria.
Ultimately, this will progress to podocyte stretching, apoptosis, and secondary focal and segmental glomerulosclerosis with declining renal function.
Acute post-infectious glomerulonephritis summary

Expected renal compensation for a respiratory acidosis
Acute: [HCO32-] = (pCO2 - 40)/10 +24
Chronic: [HCO32-] = (pCO2 - 40)/3.5 +24
Correcting serum sodium for hyperglycemia
Measured sodium [mEq/L] + 0.016 * (Serum glucose [mg/dL] - 100)
ANCA-associated glomerulonephritis summary

Conditions that cause secondary focal and segmental glomerulosclerosis

Primary focal and segmental glomerulosclerosis summary

Delta/Delta
The change (or increase) in the anion gap compared to the change (or fall) in the bicarbonate. This is a tool to determine if there is yet another underlying disorder.
Why is it so important to differentiate primary and secondary FSGS?
Treatments! The treatments are so different.
For primary, immunosuppression is indicated.
For secondary, RAAS blockade is indicated.
Diabetic nephropathy summary
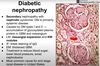
Extraglomerular aspects of diabetic nephropathy
Vascular disease as well due to thickening of the vascular media and sclerosis of the tubulointerstitium
Nodules and glomerular walls will also stain lightly with IgG, as well as albumin. This is just due to the “stickiness” of the glycosylated matrix.
Amyloid nephropathy summary









