Approach to Anemia in Small Animals Flashcards
(76 cards)
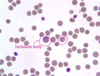
what is anemia
reduction in hemoglobin concentration of the blood
how are red blood cells produced
- stem cells are hematopoietic
- progenitor cell line: precursor cells to RBCs —> rapidly dividing in the bone marrow
- precursor cells: reticulocytes
- mature red blood cells
Slow progression and then exponential division
what cells support the production of red cells
Under the influence of EPO from the kidneys under the influence of renal hypoxia
Stromal cells in the bone marrow produce cytokines which support this process
Iron: stored as hemosiderin in macrophages
describe the breakdowns of the different anemias
non-regenerative
“pre-regenerative”
regenerative (hemorrhage, hemolysis)

what are the causes of non-regenerative anemias (7)
- primary bone marrow disease
- iron deficiency anemia
- anemia of inflammatory disease
- chronic renal failure
- endocrine renal failure
- endocrine disease (hypothyroidism)
- cobalamin deficiency
what are the causes of regenerative hemolytic anemias (4)
- IMHA
- infectious
- oxidative injury
- metabolic disorders
what are the causes of regenerative hemorrhagic anemias (4)
- trauma
- GI ulceration
- hemostatic disorder
- ruptured neoplasm
what are primary bone marrow disease (5)
- pure red cell aplasia
- aplastic anemia
- myelofibrosis
- bone marrow infiltration
- myelodysplastic syndromes
what are the causes of secondary failure of erythropoiesis (5)
- anemia of inflammatory disease
- chronic renal failure
- endocrine disease
- hemoglobin synthesis defects: Fe deficiency
- nuclear maturation defects: cobalamin deficiency
what is pure red cell aplasia
anemia affecting the precursors to red blood cells but not to white blood cells
what is aplastic anemia
a bone marrow failure where all cell lines are reduced (infectious disorders such as FeLV or some toxicities)
what is myelofibrosis
bone marrow failure secondary to replacement of normal marrow elements with fibrous tissue —> crowds it so there’s less space for hematopoiesis to occur
what is bone marrow infiltration
crowding of bone marrow and can cause other cell lines to become affected (lymphomas, etc.)
what is myelodysplastic syndromes
ineffective hematopoiesis —> non-regenerative anemia or other cytopenias (most common in cats)
what is anemia of inflammatory disease
inflammatory process that is influencing the bone marrow’s ability to utilize iron. The iron becomes sequestered —> anemias are mild to moderate and are rarely the reason for the animal’s presenting signs
how does chronic renal failure cause secondary failure of erythropoiesis
ate stage renal failure —> failure of production of EPO
what endocrine diseases can cause secondary failure of erythropoiesis
hypothryoidism
what are the distinguishing clinical features of non-regenerative anemia due to primary bone marrow disease (3)
- clinical signs related to gradual reduction in oxygen carrying capacity –> lethargy/weakness/exercise intolerance
- relatively BAR for degree of anemia
- other cell lines may be affected: thrombocytopenia/neutropenia
what are the distinguishing features of non regenerative anemia due to secondary failure of erythropoiesis
clinical signs relate to primary disease process
what are the distinguishing features of non regenerative anemia due to secondary failure of erythropoiesis in chronic renal failure
PUPD, reduced appetite, weight loss, vomiting
what are the distinguishing features of non regenerative anemia due to secondary failure of erythropoiesis in hypothyroidism
dermatological disease (bilateral symmetrical alopecia)
what are the distinguishing features of non regenerative anemia due to secondary failure of erythropoiesis in Fe deficiency
typically associated with chronic low grade external blood loss due to parasitism (internal or external), ulcerative GI disease, chronic urinary loss (often owners don’t notice the chronic blood loss and patients often present because of severe anemia)
what are the distinguishing features of non regenerative anemia due to secondary failure of erythropoiesis in cobalamin deficiency
typically associated with chronic GI disease, or rarely with genetic defects resulting in inability to absorb vitamin B12
what are the two categories of hemolytic anemia
- immune mediated
- non immune mediated