5 - MZH - Homeostasis 4 - Pancreas and regulation of blood glucose Flashcards
(19 cards)
What is the normal blood glucose level?
4-6 mmol dm3
Define hyperglacaemia and hypoglacaemia
Hyperglacaemia = Blood glucose conc rises abover the norm for a long period of time.
Hypoglacaemia = Blood glucose conc falls below the norm for a long period of time
Where is the pancreas located in the body and what is it’s function?
Behind the stomach in the upper abdomen.
It produces digestive juices and hormones.

What is this microscope showing?

Islets of langerhans within the pancreas
What is in the islets of langerhans and it’s singnificance in the role that the pancreas plays?

Islets of langerhans are composed of:
-
Alpha cells
- Sensitive to low blood glucose conc
- Secretes glucagon
- Cause hepatocytes:
- Glycogenolysis
- Gluconeogenesis
- More fatty acid respiration
-
Beta cells
- Sensitive to high blood glucose conc
- Secretes insulin
- Causes hepatocytes in (and muscle & brain cells):
- Glycogenesis
- More glucose channels
- More glucose conversion to lipids
- More glucose respiration
What are the bulk of the cells in the pancreas used for?
- Used to synthesis and release digestive enzymes.
- Cells are arranged in small groups each called an acinus (plura = acini) surrounding tiny tubules.
- Secretions enter tubules which merge to form the pancreatic duct which enties the secretions into the duodenum.
- Acini then can be described as exocrine tissue.
From which 3 sources can glucose enter the blood from?
- Directly from the diet - As glucose or from the hydrolysis of other carbohydrates.
- glycogenolysis (hydrolysis of glycogen) - From stores in the liver and muscle cells. Liver is the major source here.
- Gluconeogenesis - Production of new glucose from sources other than carbohydrates. In the liver glucose can be made from amino acids + glycerol.
Describe the sequence of events that occur in order to secrete insulin (7)

- Beta cells havea resting potential of -70mV across their cell surface membranes - They’re -ve compared to their surroundings.
- Resting potential is generated by K+ channels which pump out K+ ions and are sensitive to ATP.
- If conc of glucose in bloos plasma rises, glucose enters the beta cells and is respired.
- This results in an increases ATP conc inside the beta cells, causes K+ channels to close.
- Negative resting potential is removed and membrane is depolarised.
- Ca2+ channels in cell surface membrane ioen and Ca2+ ions pass into the beta cells.
- Influx of Ca2+ ions triggers movement of vesicles containing insulin to the cell surface membrane and fuse with it releasing the insulin by exocytosis.

Fill in the blanks


3 ways in which blood glucose conc can be further lowered alongside with beta cells secreting glucagon
- Cellular respiration is increased, using up more glucose and increasing its uptake by most cells
- Rate of glycogenesis (glucose → glycogen conversion) is increased in cells of the liver and muscles
- Rate of conversion of glucose to fat in adipose tissue is increased
How to alpha cells respond to a fall in blood glocose conc?
They secrete glucagon. ONLY liver cells have the specific glucagon receptor on their cell surface membrane.
- Converts glycogen → glucose
- Increase conversion fo amino acids + glycerol into glucose (gluconeogenesis)
What is insulin and glucagon known to act as?
Antagonistically. They act against each other.
How does adrenaline play a role into controlling blood glucose conc?
Adrenaline is produced at times of excitement or stress from the adrenal glands that lie close to the kidneys.
- Causes a rapid break down of glycogen in the liver into glucose which enters the blood stream raising blood glucose levels
- Has a short term effect and is only used when a very rapid response is needed
What is diabetes mellitus?
Diabetes mellitus is a metabolic disorder in which an inability to control blood glucose levels due to a lack of the hormone insulin or a loss of responsiveness to it
What are the 2 types of diabetes mellitus and how are they different?
What causes each of them?
TYPE 1 (insulin dependent) diabetes:
- Arises due to the body being unable to produce insulin.
- Typically appears in childhood.
- May be a result of an autoimmune response when the body’s immune response attacks its own cells, in this case beta cells in the islets of langerhans, it may result from a viral infection.
TYPE 2 (non-insulin dependent) diabetes:
- Usually due to the glycoprotein insulin receptor proteins not responding to insulin.
- Results in a permanently raised blood glucose levels.
- Multiple factors can cause it to arise:
- Obesity
- Lack of regular exercise
- Diet high in sugars, particuarly refined sugars
- Family history
- Being of Afro-Caribbean origin
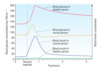
On this graph what would a diabetic’s clood glucose conc and blood insulin conc compare to a non diabetic look like?

Current treatments?
TYPE 1:
- Injections of insulin - can use pig insulin but nowadays insulin can be GM using E.Coli.
- Insulin pump therapy - Small device constantly pumps insulin at a controlled rate into the bloodstream through a needle that is permanently under the skin.
- Islet cell transplantation - Healthy beta cells from a donor are implanted into the pancreas of a Type 1 sufferer.
- Complete pancreas trnasplant.
TYPE 2:
- Weight loss.
- Regular exercise.
- Controlled diet - aiming to balance carbohydrate intake with carbohydrate use.
Future treatments for Type 1 diabetics?
Use of stem cells to grow islet of langerhans cells in the pancreas
We use to use pig insulin but nowadays we use genetically modified E.Coli to produce insulin. Give 6 advantages of using E.Coli produced insulin?
- Exact copy of human insulin, it’s faster and more effective
- Less chance of rejection due to immune response
- Lower risk of infection
- Cheaper to manufacture than to extract from animals
- Easier to produce high quantities to match demand
- Less moral/religous objects to using insulin produced by bacteria than that extracted from animals


